What to know
- CDC uses statistical and mathematical modeling to estimate the burden of COVID-19-associated illnesses, outpatient visits, hospitalizations, and deaths in the United States.
- A multiplier model approach to disease burden estimation, similar to that used to estimate the burden of influenza, is used to estimate the burden of COVID-19.
- Overall, COVID-19 continues to affect the health of people and healthcare systems in the United States.
Overview
Since the onset of the COVID-19 pandemic, the burden of COVID-19-associated illnesses, outpatient visits, hospitalizations, and deaths in the United States has varied. The public health burden of COVID-19 is influenced by numerous factors, including:
- the characteristics of circulating variants of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.
- population immunity to circulating variants from both prior infection and vaccination.
- access to and utilization of medical care, including antiviral medication.
COVID-19 is no longer a nationally notifiable disease, meaning COVID-19 cases are no longer reported to CDC. Therefore, CDC uses statistical and mathematical modeling to estimate the weekly cumulative burden of COVID-19-associated illnesses, outpatient visits, hospitalizations, and deaths in the United States.
Preliminary estimates of the burden of COVID-19 are based on weekly reported hospitalizations with laboratory-confirmed SARS-CoV-2 infections for the time period of reference. Estimates of the cumulative burden since October 1 of the current year begin once sufficient data are available for producing stable estimates with updates occurring weekly through September 30 of the following year.
The methods used to estimate preliminary COVID-19 burden estimates are similar to the approach used to estimate the preliminary burden of influenza estimates12345. Differences between the COVID-19 and influenza modeling approaches include the model inputs, the modeling assumptions, the analytic age groups used, and how uncertainty is estimated and incorporated into the model.
More details about the methods used to estimate the weekly hospitalization burden of COVID-19 can be found in a recent publication.6
How CDC estimates the cumulative burden of COVID-19
Hospitalizations
Laboratory-confirmed COVID-19-associated hospitalization rates are obtained from the Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). COVID-NET is a collaboration between CDC, the Emerging Infections Program network, the Council of State and Territorial Epidemiologists, and selected state and local health departments in the United States that conduct population-based surveillance. COVID-NET data come from hospitals that serve approximately 10% of the U.S. population.
To estimate national COVID-19–associated hospital admissions from COVID-NET data, CDC used a hierarchical Bayesian modeling approach, namely, the Conditionally Autoregressive–Random Effects (CAR-RE) model. 6The CAR-RE model accounts for dependencies across weeks in COVID-NET reported hospitalizations via conditionally autoregressive (CAR) and site-level random effects (RE) to reflect unmeasured differences among participating COVID-NET sites. Additionally, the CAR-RE model approach enables estimation of the uncertainty in the derived national hospitalization counts due to extrapolation from the areas covered by COVID-NET surveillance to the entire US population.
Modeled hospitalization counts are adjusted to reflect under-detection using both the estimated probability that an inpatient is tested for SAR-CoV-2 infection and the expected sensitivity of the utilized tests. Testing is subject to provider discretion, facility policy, and test availability. The data on testing can lag, so testing data from recent prior years are applied to the current season estimates.
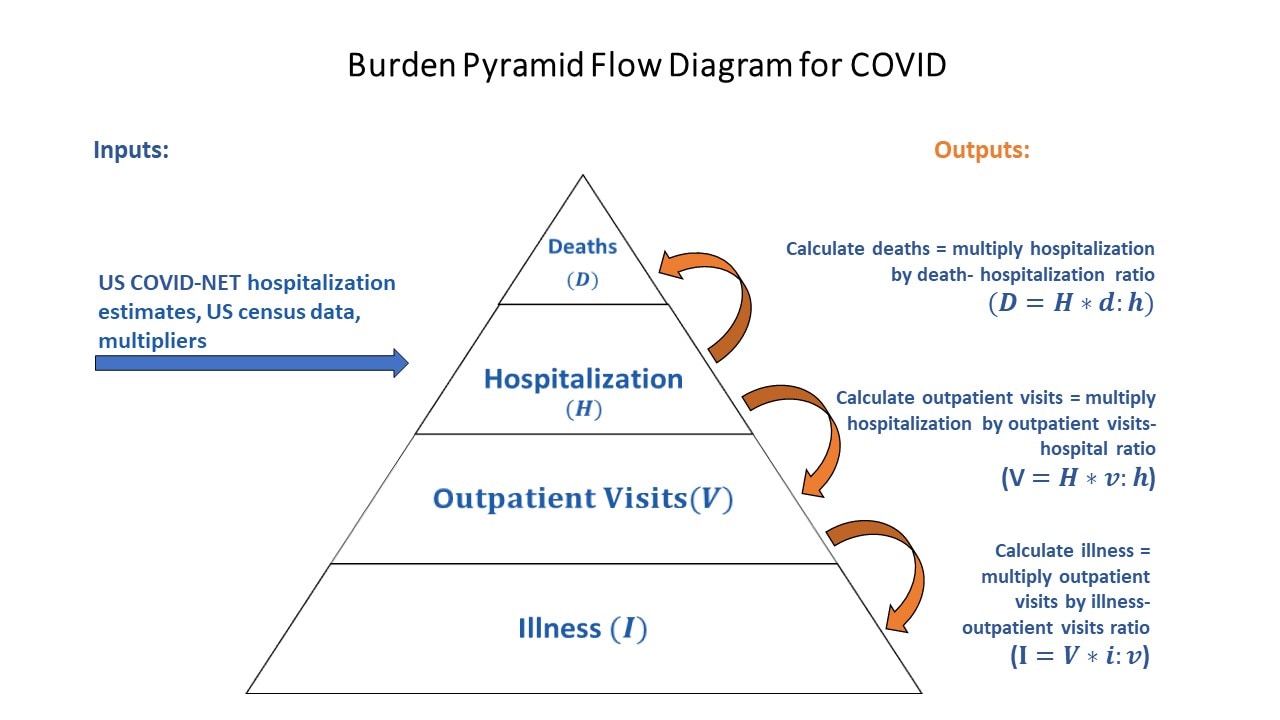
The adjusted COVID-19–associated hospitalization estimates are then used to estimate additional measures of COVID-19–associated burden including illnesses, outpatient visits, and deaths via a probabilistic mathematical multiplier model using Monte Carlo simulations.
How CDC estimates COVID-19 outpatient visits and illnesses in the United States
With the estimated national-level counts of age-specific COVID-19-associated hospitalizations, the number of outpatient visits and illnesses are estimated through age-specific ratios. A range of ratios were extracted from published literature since January 2022, ongoing studies, and input from subject matter experts to generate a range of age group-specific ratios for these estimates. These ratios included the number of outpatient visits due to COVID-19 per COVID-19-associated hospitalizations and the number of COVID-19 illnesses per COVID-19 outpatient visit.
Ratio ranges of hospitalizations to symptomatic illnesses, outpatient visits, and deaths were estimated using statistical models. These outcome-specific ratio ranges are applied to the estimated number of hospitalizations to generate a range for the number of illnesses, outpatient visits, and deaths. All outcomes (illnesses, outpatient visits, hospitalizations, and deaths) were combined to derive the total estimated burden range.
How CDC estimates COVID-19-Associated Deaths in the United States
It has been recognized that COVID-19 is underreported on death certificates. 7COVID-19 may lead to death from other causes that are secondary complications of COVID-19, such as myocardial infarction, stroke, pulmonary embolus, or bacterial pneumonias; these COVID-19 associated deaths may be attributed to these other causes on death certificates. Additional reasons for underreporting may be that patients aren't always tested for COVID-19, particularly older adults who are at greatest risk of COVID-19 complications and death, and not all deaths related to COVID-19 occur in the hospital.
Because there is underreporting on death certificates, only counting deaths where COVID-19 was recorded on a death certificate would greatly underestimate COVID-19's true impact. Modeling strategies are therefore commonly used to estimate total COVID-19 associated deaths. The methods used to estimate the number of COVID-19 associated deaths were adapted from similar methods used for estimating influenza deaths.12345
In-hospital deaths among those hospitalized with laboratory-confirmed SARS-CoV-2 and observed in COVID-NET were adjusted for under-detection of COVID-19. Adjustments were based on the frequency and sensitivity of SARS-CoV-2 testing among those who died in the hospital with pneumonia, influenza, and/or COVID-19–like illnesses.
In addition, death certificate data were used to estimate how likely COVID-19–associated deaths were to occur outside the hospital. Death certificates that have pneumonia, influenza, or COVID-19 causes (P&I), other respiratory and circulatory causes (R&C), or other non-respiratory, non-circulatory (non-R&C) causes of death were examined. The proportion of these deaths that occurred while in the hospital was then estimated using data provided by the National Center for Health Statistics (NCHS). Information on the causes of death from COVID-NET was used to determine the mixture of P&I, R&C, and other coded deaths to include in the investigation of death certificate data. Finally, once the proportion of COVID-19–associated deaths that occurred outside of the hospital was estimated, the death-to-hospitalization ratio was estimated.
Data needed to estimate COVID-19–associated deaths may lag for up to two years. When death certificate data were not available for the year being estimated, adjusted values based on data observed in prior years were used and estimates updated when more current data became available.
Limitations of COVID-19 Burden Estimates
These estimates are subject to multiple limitations.
- Rates of COVID-19–associated hospitalizations are based on data reported to COVID-NET that are current as of the time estimates are made. Weekly case counts may differ as data are updated by COVID-NET sites. 8The most updated unadjusted rates of hospitalization for COVID-NET sites are available on COVID-NET Interactive.
- National rates of COVID-19–associated hospitalizations and in-hospital deaths are adjusted for the frequency of SARS-CoV-2 testing and the sensitivity of SARS-CoV-2 diagnostic assays, using a multiplier approach. However, data on testing practices during the current year may not be available at the time of estimation. In such cases, rates are adjusted using data from prior years. Burden estimates from a given year are updated at a later date when data on contemporary testing practices become available.
- Estimates of COVID-19–associated illnesses are made by multiplying the number of outpatient visits by the ratio of illnesses to outpatient visits. The estimates of COVID-19–associated outpatient visits are made by multiplying the number of hospitalizations by the ratio of hospitalizations to outpatient visits. These ratios are based on published literature, ongoing studies, and expert review and input. Substantial limitations in the published literature for age-specific estimates heighten the uncertainty of the ratios. In addition, estimates may not be accurate if circulating variants cause more or less severe illness, or if patterns of care-seeking change.
- Estimates of COVID-19–associated deaths rely on information about location of death from death certificates. However, death certificate data for a given year may not be available at the time of estimation. When this occurs, death certificate data from prior years where these data are available from the National Center for Health Statistics are used. Specifically, the model uses the frequency of COVID-19-associated deaths that have cause of death related to pneumonia or influenza (P&I), other respiratory or cardiovascular (other R&C), or other non-respiratory, non-cardiovascular (non-R&C) to account for deaths occurring outside of a hospital by cause of death. If these frequencies are not available from a given year at the time of estimation, the frequencies of each cause of death from the most recent year of data available are used.
- Reed C, Chaves SS, Daily Kirley P, et al. Estimating influenza disease burden from population-based surveillance data in the United States. PLoS One. 2015;10(3):e0118369. https://doi.org/10.1371/journal.pone.0118369
- Rolfes, MA, Foppa, IM, Garg, S, et al. Annual estimates of the burden of seasonal influenza in the United States: A tool for strengthening influenza surveillance and preparedness. Influenza Other Respi Viruses. 2018; 12: 132– 137. https://doi.org/10.1111/irv.12486
- Centers for Disease Control and Prevention. Estimated influenza illnesses and hospitalizations averted by influenza vaccination – United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2013 Dec 13;62(49):997-1000. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6249a2.htm
- Reed C, Kim IK, Singleton JA, et al. Estimated influenza illnesses and hospitalizations averted by vaccination–United States, 2013-14 influenza season. MMWR Morb Mortal Wkly Rep. 2014 Dec 12;63(49):1151-4.
- Reed C, Angulo FJ, Swerdlow DL, et al. Estimates of the Prevalence of Pandemic (H1N1) 2009, United States, April–July 2009. Emerg Infect Dis. 2009;15(12):2004-2007. https://dx.doi.org/10.3201/eid1512.091413
- Devine O, Pham H, Gunnels B, et al. Extrapolating Sentinel Surveillance Information to Estimate National COVID-19 Hospital Admission Rates: A Bayesian Modeling Approach. Influenza and Other Respiratory Viruses. https://onlinelibrary.wiley.com/doi/10.1111/irv.70026. Volume18, Issue10. October 2024.
- Excess natural-cause deaths in California by cause and setting: March 2020 through February 2021 | PNAS Nexus | Oxford Academic (oup.com
- COVID-NET | COVID-19 | CDC
