 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Necrotic Arachnidism -- Pacific Northwest, 1988-1996Although spider bites are common in many parts of the United States, most domestic spiders are not substantially venomous to man. The best known exceptions are widow spiders (Latrodectus spp., including the black widow L. mactans) and brown spiders (Loxesceles spp., particularly the brown recluse, Lox. reclusa). However, cases of arachnid envenomation from the hobo spider (Tegenaria agrestis) are being reported increasingly in the Pacific Northwest. This report summarizes investigations of three cases of T. agrestis bites among persons in Idaho, Oregon, and Washington; spider bites reported to U.S. poison-control centers during 1994; and emphasizes the need for physicians in the northwestern United States to consider this species as a cause of toxic arachnidism. Case Reports Case 1. On November 23, 1995, a 10-year-old boy residing in suburban Portland, Oregon, was bitten on the lower leg while asleep in bed. Within 48 hours, two swollen and erythematous lesions 3-4 cm in diameter developed around the site of the bite. Both were hot to the touch, with central blistering. Seven days after the bite, necrosis and skin sloughing developed, and his entire leg and ankle were red and edematous. The patient reportedly was febrile and nauseated and had severe headaches. Treatment included oral diphenhydramine hydrochloride and alternating local applications of heat and ice. After 30 days, ecchymotic residua were still visible, but local tenderness was diminished. Migraine-like headaches persisted for 4 months. Pesticide applicators who inspected the house reported that it was infested with T. agrestis spiders. Case 2. On October 8, 1992, a 42-year-old woman residing in Bingham County, Idaho, who had a history of phlebitis felt a burning sensation on her left ankle while at work at a convenience store. She rolled up the leg of her pants and found a crushed brown spider, subsequently identified as T. agrestis. The pain on her ankle persisted, and within 3 hours she was dizzy and nauseated and had a severe headache. An erythematous lesion with a vesicular center was noted several hours later; by the next day the vesicle had ruptured, leaving an open ulcer with a diameter of approximately 2 mm. During the next 10 weeks the ulcer deepened and expanded to a diameter of approximately 30 mm, circumscribed by a blackish margin. The patient sought medical care on December 26, 1992, and received a course of antibiotics. The ulceration continued to enlarge, and swelling of the leg and toes impaired walking. A venogram in July 1993 indicated deep venous thrombosis, which did not respond to standard therapy. The lesion healed slowly between May and November 1994, but left a cratered scar. The patient remains unable to work in situations requiring standing or walking. Case 3. In late January 1988, a 56-year-old resident of Spokane, Washington, was bitten by a "bug" on her right thigh. Within 24 hours, she developed a severe headache, nausea, and altered mentation. Although symptoms persisted, she did not seek medical attention until February 16, 1988, when she began to bleed from her ears and other orifices. She was admitted to a hospital with a diagnosis of aplastic anemia, pancytopenia, and thrombocytopenia. An eschar on her leg was consistent with necrosis from a spider bite. Despite transfusion therapy, the patient developed severe internal hemorrhage and died in early March 1988. T. agrestis spiders were abundant along railroad tracks adjacent to the patient's home during an inspection of the patient's neighborhood of residence. Spider Bites Reported to Poison-Control Centers During 1994 Some persons who suspect they have been bitten by spiders and some physicians who treat spider bites contact poison-control centers for advice or information; most of these centers use a standard coding scheme for classifying calls. In 1994, poison-control center log reports compiled by the American Association of Poison Control Centers listed 9418 spider bites (Table_1) (1). Of these, a disproportionate number (1027 {10.9%}) was reported to poison-control centers in Idaho, Oregon, and Washington, which comprise approximately 4% of the U.S. population. A specific kind of spider was noted for 246 of these bites, including 66 (27%) that were classified as brown recluse bites (there is no coding category for hobo spiders). Adapted from: CD Summary 1995;14(no. 22), Center for Disease Prevention and Epidemiology, Oregon Health Div, Oregon Dept of Human Resources. Reported by: DK Vest, Idaho Falls, Idaho. WE Keene, PhD, M Heumann, MPH, Center for Disease Prevention and Epidemiology, Oregon Health Div, Oregon Dept of Human Resources; S Kaufman, MD, West Linn Pediatric Clinic, West Linn, Oregon. Editorial NoteEditorial Note: Although envenomating spider bites in the Pacific Northwest often are erroneously attributed to brown recluse spiders, most such bites are caused by hobo spiders (formerly also known as "aggressive house" spiders). In Idaho, Oregon, and Washington, venomous spider bites usually are reported from areas with well-established populations of hobo spiders (2). T. agrestis spiders often are found in the homes of persons with these bites; recluse spiders are never found (3). Lox. reclusa and other Loxosceles species are not found in the Pacific Northwest (Figure_1) (4). The local effects of T. agrestis envenomation are similar to those of brown recluse bites -- a syndrome described as necrotic arachnidism (5). Although many bites occur without substantial envenomation, the cases described in this report illustrate the possible severe outcomes for hobo spider envenomation. Similar local reactions can result from the bite of yellow sac spiders (Cheiracanthium spp.), which are widely distributed in North America and elsewhere (6). The bite of the hobo spider usually is initially painless. A small area of induration may appear within 30 minutes, surrounded by an area of expanding erythema that can attain a diameter of 5-15 cm. Blisters develop within 15-35 hours; soon thereafter the blisters can rupture with a serous exudate encrusting the cratered wound. An eschar can develop with underlying necrosis and eventual sloughing of affected tissue. Lesions generally heal within 45 days, but can result in a permanent scar; healing can require up to 3 years if the bite occurred in fatty tissue. The most common systemic symptom is a severe headache -- occurring as soon as 30 minutes after the bite, and usually within 10 hours -- that can persist for a week. Other symptoms can include nausea, weakness, fatigue, temporary memory loss, and vision impairment. Protracted systemic effects, including aplastic anemia, intractable vomiting, or profuse secretory diarrhea, are rare but may be associated with death (7). Optimal treatment for necrotic spider bites is not well defined (5). Systemic corticosteroid therapy may be of benefit if any substantial hematologic abnormalities are noted other than a moderate leukocytosis. Surgical repair may be necessary in severe cases of ulcerative lesions, but should not be initiated until the primary necrotizing process is completed (5). T. agrestis is native to Europe and probably was introduced into the Seattle area in the 1920s or early 1930s (8); it subsequently has spread as far as central Utah and the Alaskan panhandle (Figure_1). Hobo spiders build funnel-shaped webs in dark, moist areas, often in wood piles, crawl spaces, or around the perimeters of homes (9); they rarely climb vertical surfaces and are uncommon above basements or ground level. Hobo spiders are moderately large (7-14 mm body length; 27-45 mm leg span) and brown with grey markings. They can move quickly (up to 1 m/second) (2), and can bite if provoked or threatened. Mature spiders are abundant from mid-summer through fall when males, which are more venomous than females, wander in search of females (9). Practical control strategies should emphasize personal protection rather than attempted eradication of T. agrestis populations. Exposure can be reduced through the use of gloves and other clothing that covers the skin while working in crawl spaces and similar locations and through precaution when retrieving firewood or other items stored in potentially infested areas. Screens on basement and ground-floor windows and insulation strips under doors may reduce the risk for spider infestation. Venomous spider bites are not reportable in any state, and there are no reliable estimates of the incidence of such bites or how often medical attention is sought for them. The addition of a specific designation for hobo spider envenomations in poison-control center report classifications may provide better information on how frequently these bites occur. Medical references should be updated to acknowledge causes of necrotic arachnidism other than Loxosceles spp. References
TABLE 1. Reported spider bites to poison-control centers -- United
States and Pacific Northwest, 1994
=======================================================================
United States * Pacific Northwest +
------------------- -----------------------
Type of spider No. (%) No. (%)
-----------------------------------------------------------------------
Black widow 2120 ( 22.5) 139 ( 13.5)
Brown recluse 1835 ( 19.5) 66 ( 6.4)
Tarantula 82 ( 0.9) 41 ( 4.0)
Other/Unknown 5381 ( 57.1) 781 ( 76.1)
Total 9418 (100.0) 1027 (100.0)
-----------------------------------------------------------------------
* A total of 65 reporting poison-control centers that represent 83% of
the U.S. population (1).
+ A total of three reporting poison-control centers that represent 100%
of the population in Idaho, Oregon, and Washington. Source: 1994
Annual Report of the Toxic Exposure Surveillance System for each
state, published by each state's poison-control center.
=======================================================================
Return to top. Figure_1 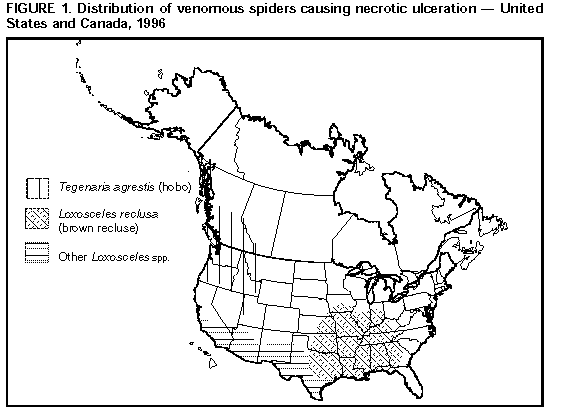 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|