 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Contraceptive Practices Before and After an Intervention Promoting Condom Use to Prevent HIV Infection and Other Sexually Transmitted Diseases Among Women -- Selected U.S. Sites, 1993-1995Because heterosexual contact is the most common mode of human immunodeficiency virus (HIV) transmission among women (1), development of effective strategies to reduce sexually transmitted HIV infection is critical. In addition, because most women at risk for HIV infection are reproductive aged (14-44 years), effective use of contraceptives is important to prevent unintended pregnancies (2,3). Latex condoms used by males, when used consistently and correctly, are highly effective at reducing the risk for HIV infection and other sexually transmitted diseases (STDs) (4); however, hormonal contraceptive methods or surgical sterilization are more effective for preventing pregnancy (5). One possible effect of encouraging women to use condoms for HIV/STD prevention with their male partners is that women may discontinue use of hormonal contraceptive methods. To assess whether encouraging women to use condoms for HIV/STD prevention affects their contraceptive practices, CDC analyzed longitudinal data on contraceptive methods and condom use for HIV/STD prevention that were collected as part of a randomized trial evaluating HIV-counseling methods during August 1993-June 1995 (6). This report summarizes the findings of the analysis, which indicate that, among reproductive-aged women who were encouraged to use condoms for HIV/STD prevention, consistent condom use for HIV/STD prevention increased among women using each contraceptive method studied. In addition, most women using hormonal contraceptive methods continued to use them after the intervention, and the overall proportion of women protected against pregnancy increased. * Women included in this analysis (1793 {55%} of eligible women) were HIV-negative, heterosexual, and reproductive-aged STD patients of inner-city clinics in Long Beach and San Francisco, California; Denver, Colorado; Baltimore, Maryland; and Newark, New Jersey, who agreed to participate in the HIV-prevention counseling trial. To participate in the study, women had to have reported having had vaginal sex during the preceding 30 days and had to have come to the STD clinic for a full diagnostic examination. As part of the study, participants completed an interview at enrollment, received HIV-prevention counseling or education encouraging consistent condom use with all male sex partners, and completed a follow-up interview 3 months after enrollment. Both interviews included questions about condom use during vaginal sex during the preceding 3 months. Women also were asked about their pregnancy intentions and methods they were using to prevent pregnancy. Contraceptive methods reported at enrollment and at follow-up, in descending order of contraceptive effectiveness, were 1) sterilization (i.e., tubal ligation, vasectomy, or medical infertility by self-report); 2) hormonal contraceptives (i.e., oral, injected, or implanted); 3) latex condoms used by men; 4) other barrier methods (i.e., diaphragm or spermicides of all forms; 5) minimally effective methods (i.e., rhythm or withdrawal); and 6) no method. Women reporting more than one contraceptive method were classified based on the most effective contraceptive method reported (5). Because condoms can be used for both HIV/STD prevention and contraception, questions about frequency of condom use for HIV/STD prevention were asked separately from those about contraceptive methods. Consistent condom use was defined as use of condoms during every episode of vaginal intercourse during the preceding 3 months. Of the 1793 women who participated in the trial, longitudinal data about contraceptive use and condom use for HIV/STD prevention were available at both the enrollment and follow-up interviews for 1303 (73%) women; of these, 1173 (90%) reported having had vaginal sex at least once during the 3-month study interval. Study participants were predominantly young (median age: 24 years) and racial/ethnic minorities (51% non-Hispanic black, 19% Hispanic, and 7% races other than non-Hispanic white), and most (60%) were unemployed. The characteristics of these women were similar to those of all women attending these inner-city STD clinics (6). The median age at first sexual intercourse was 15 years. During the 3 months preceding the enrollment interview, the median number of male partners was one, the median number of vaginal sex episodes was 12, and 973 (83%) women reported having a male partner they considered their primary ("main") sex partner. At the enrollment visit, 32% of participants had at least one STD (syphilis, gonorrhea, chlamydia, trichomonas, pelvic inflammatory disease, or herpes simplex virus) diagnosed. After receipt of counseling to encourage consistent condom use, most (75%) women who reported using hormonal contraception at enrollment also reported hormonal contraceptive use at follow-up. In addition, 56% of women who reported using no method or minimally effective contraceptive methods at enrollment subsequently were sterilized (3%) or began using condoms (43%) or hormonal methods (10%) as contraception (Table_1). Of the 249 women who reported using hormonal methods at enrollment, four (2%) were sterile, and 188 (75%) reported still using hormonal methods at follow-up. The other 57 (23%) women were either using condoms (12%), other barrier methods (1%), minimally effective contraceptive methods (3%), or no method (1%); were pregnant (3%); or wanted to become pregnant (3%). Of the 345 women who reported using condoms for contraception at enrollment, 236 (68%) were still using condoms for contraception at follow-up, and 42 (12%) reported using hormonal methods or being sterilized. Of the 223 women using minimally effective contraceptive methods or no method at enrollment, 96 (43%) reported using condoms for contraception at follow-up, and 29 (13%) reported using hormonal methods or being sterilized. From enrollment to follow-up, consistent condom use among all 1173 women increased from 13% at enrollment to 36% at follow-up (p less than 0.001, McNemar's chi-square) (Figure_1). Consistent condom use increased among women regardless of contraceptive method reported at enrollment: for the 208 women who were sterile, from 8% to 34%; for the 249 women who used hormonal methods, from 10% to 31%; for the 345 women who used condoms, from 28% to 47%; for the 15 women who used other barriers, from zero to 33%; and for the 223 women who reported using minimally effective methods or no method at enrollment, from 1% to 30%. Reported by: JM Douglas, MD, Denver Dept of Health; T Hoxworth, PhD, Colorado Dept of Public Health and Environment. J Rogers, MS, M Iatesta, MPA, New Jersey Dept of Health and Senior Svcs. F Rhodes, PhD, CK Malotte, DrPH, Long Beach Dept of Health and Human Svcs, California State Univ, Long Beach; GA Bolan, MD, C Kent, MPH, San Francisco Health Dept. J Zenilman, MD, A Lenz, MPA, Baltimore City Health Dept, Maryland. Project RESPECT Study Group. Behavioral Interventions and Research Br, Div of Sexually Transmitted Diseases Prevention, and Prevention Svcs Research Br, Div of HIV/AIDS Prevention-Surveillance and Epidemiology, National Center for HIV, STD, and TB Prevention, CDC. Editorial NoteEditorial Note: The findings in this report indicate that, among the reproductive-aged women who were encouraged to use condoms for HIV/STD prevention, consistent condom use for HIV/STD prevention increased among women using each contraceptive method studied. In addition, although some women who are encouraged to use condoms for HIV/STD prevention may discontinue use of hormonal contraceptives, 75% of participants in this study who were using hormonal contraceptives at enrollment continued to use them after the condom-promotion intervention. From enrollment to follow-up, only 12% of women changed from using hormonal contraceptives to using condoms for contraception. Furthermore, approximately half of the women who were using minimally effective or no contraceptive methods at enrollment changed to using more effective contraceptive methods after the condom-promotion intervention, and of women using condoms for contraception, the proportion using them consistently nearly doubled from enrollment to follow-up. Thus, for women who were neither sterilized nor using hormonal contraceptive methods at enrollment, the risk for unintended pregnancy at follow-up was reduced because of the increase in consistent condom use for HIV/STD prevention or the use of other effective contraceptive methods. The findings in this report are subject to at least two limitations. First, because the study sample was not representative of all women in the United States at risk for HIV infection or other STDs, these findings may not be generalizable to all U.S. women at risk for HIV infection or other STDs. Second, because the study is based on self-reported data, the results cannot be validated and may be subject to bias; furthermore, condom use may have been overreported. Overall, most (75%) women reported that their sex partners used latex condoms, and many (36%) used them consistently after the intervention. Many sexually active women are at risk for HIV and other STDs, and use of latex condoms by their sex partners is an effective strategy for preventing HIV/STDs among women. For the women described in this report, condom promotion increased condom use but did not adversely influence effective contraception strategies. Counselors, clinicians, and other public health providers should continue to educate women about the benefits of consistent, correct use of latex condoms for HIV/STD prevention. In addition, effective contraceptive strategies should be promoted to women who do not want to become pregnant. References
* Single copies of this report will be available until May 1, 1998, from the CDC National AIDS Clearinghouse, P.O. Box 6003, Rockville, MD 20849-6003; telephone (800) 458-5231 or (301) 217-0023. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 1. Number and percentage distribution of the most effective contraceptive method * used by women participating in a condom-promotion intervention, by time period -- Long Beach and San Francisco, California; Denver, Colorado; Baltimore,
Maryland; and Newark, New Jersey, 1993-1995 +
=====================================================================================================================================================================================================================================================
Pregnancy intention/Contraceptive method at 3-month follow-up
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Do not intend to become pregnant
Pregnancy intention/ ---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Contraceptive Other Minimally Intend to become
method Sterilization Hormonal Condom barriers effective No method Pregnant pregnant
at -------------- ----------- ----------- ---------- ------------ ------------- ----------- ------------------
enrollment No. (%) & No. (%) No. (%) No. (%) No. (%) No. (%) No. (%) No. (%) Total
-----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Do not intend to
become pregnant
Sterilization 207 (100) 0 -- 0 -- 0 -- 0 -- 0 -- 1 (<1) 0 -- 208
Hormonal 4 ( 2) 188 (75) 31 (12) 2 ( 1) 7 ( 3) 3 ( 1) 7 ( 3) 7 ( 3) 249
Condom 4 ( 1) 38 (11) 236 (68) 2 ( 1) 10 ( 3) 14 ( 4) 27 ( 8) 14 ( 4) 345
Other barriers 0 -- 0 -- 8 (53) 2 (13) 1 ( 7) 1 ( 7) 3 (20) 0 -- 15
Minimally effective 1 ( 3) 7 (18) 12 (32) 1 ( 3) 8 (21) 4 (11) 4 (11) 1 ( 3) 38
No method 6 ( 3) 15 ( 8) 83 (45) 0 -- 8 ( 4) 37 (20) 24 (13) 12 ( 6) 185
Pregnant 2 ( 3) 8 (14) 15 (26) 0 -- 6 (10) 2 ( 3) 24 (41) 1 ( 2) 58
Intend to become 0 -- 2 ( 3) 19 (25) 0 -- 3 ( 4) 9 (12) 11 (15) 31 (41) 75
pregnant
Total 224 258 404 7 43 70 101 66 1173
-----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
* Contraceptive methods in descending order of contraceptive effectiveness were 1) sterilization (i.e., tubal ligation, vasectomy, or medical infertility by self-report); 2) hormonal contraceptives (i.e., oral, injected, or implanted); 3) latex
condoms used by men; 4) other barrier methods (i.e., diaphragm or spermicides of all forms); 5) minimally effective methods (i.e, rhythm or withdrawal); and 6) no method.
+ n=1173. Because of rounding, percentages may not total 100%.
@ All percentages are row percentages.
=====================================================================================================================================================================================================================================================
Return to top. Figure_1 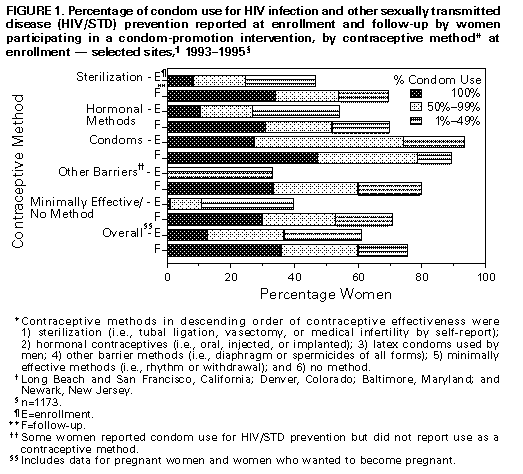 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|