 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Population-Based Survey for Drug Resistance of Tuberculosis -- Mexico, 1997The World Health Organization (WHO) estimates that 90 million cases of tuberculosis (TB), resulting in 30 million deaths, will occur during the 1990s (1). To address this problem, WHO has recommended a comprehensive strategy of directly observed treatment, short-course (DOTS) * (2). Although DOTS results in cure rates of greater than or equal to 80% (3 ), the worldwide emergence of strains of Mycobacterium tuberculosis (MTB) resistant to antimycobacterial agents threatens this strategy for TB control (2). In 1994, WHO and the International Union Against Tuberculosis and Lung Disease (IUATLD) proposed the establishment of a global surveillance program to monitor drug resistance (2). In 1997, the Secretary of Health of Mexico, in collaboration with CDC, developed and implemented a national survey of drug resistance for TB as part of the global project on TB drug resistance. This report describes study results for three states in Mexico (Baja California, Oaxaca, and Sinaloa) and presents the first population-based TB drug-resistance data available for that country. For this study, the 31 states and Federal District of Mexico were categorized by reported TB incidence in 1994 into three strata (high, medium, and low incidence). Nine of these 32 areas were randomly chosen in proportion to the number of cases reported in each strata. Baja California (high), Sinaloa (high), and Oaxaca (medium) were selected as the first of the nine to participate in the survey (Figure_1). Cases were enrolled from two of the country's five major public-sector health-care agencies, the Secretaria de Salud Administracion (Secretary of Health) (SSA) and the Instituto Mexicano de Seguro Social (Mexican Institute of Social Security) (IMSS); these two agencies together provide health-care service to approximately 80% of the population and diagnose and manage 90% of reported TB cases. During January-April 1997, physicians, epidemiologists, and laboratory workers from these agencies in all three states received extensive training from SSA in conducting the survey. During April 1- October 31, physicians completed patient enrollment forms for all patients submitting at least one sputum sample for evaluation for pulmonary TB. All acid-fast bacilli (AFB) smear-positive samples were sent to the state laboratories for inoculation onto Lowenstein-Jensen media and were forwarded to the Instituto Nacional de Diagnostico y Referencia Epidemiologicos (National Diagnostic and Epidemiologic Reference Institute) (INDRE) in Mexico City for species identification and testing for drug susceptibility to isoniazid, rifampin, pyrazinamide, streptomycin, and ethambutol using the radiometric method (4). The reference institute and CDC exchanged and tested 20 MTB isolates on two separate occasions for quality-control monitoring; there was a discrepancy in one drug for one isolate, for an accuracy rate of 97.5%. In this analysis, resistance to one or more drugs was defined as resistance to isoniazid, rifampin, or pyrazinamide -- the three drugs that constitute first-line treatment in Mexico. Resistance to one or more drugs was defined as primary for patients who had never taken anti-TB drugs and as acquired for patients reporting previous treatment with anti-TB drugs. Multidrug-resistant (MDR) TB was defined as resistance to at least isoniazid and rifampin (2). Primary resistance was considered to reflect infection with a resistant organism, and acquired resistance was considered to reflect the development of resistance during the course of previous therapy. During the study period, 816 patients were officially reported with AFB smear-positive pulmonary TB: 351 from Baja California, 110 from Oaxaca, and 355 from Sinaloa (Table_1). Of these, 602 (74%) were enrolled in the study; MTB isolates were available for drug-susceptibility testing from 440 (73%) patients. Of the remaining specimens, 22% had no growth, 4% were contaminated, and 1% had nontuberculous mycobacteria. Of patients with MTB isolates, 24% had a history of prior TB treatment. The median age of patients was 36 years (range: 10-99 years); 69% were male. No difference was observed between patients with culture-positive and culture-negative isolates by age or prior history of TB. Primary resistance to one or more of the three current first-line drugs used in Mexico was 12%; acquired resistance was 50% (Table_2). Levels for both primary and acquired drug resistance did not differ significantly by state or by patient age or sex. Levels of combined resistance (primary and acquired), which represent an approximation of the overall level of drug resistance to isoniazid, rifampin, pyrazinamide, ethambutol, or streptomycin the community, were 26% (113 of 440) for one or more of the five drugs, 18% (79 of 440) for isoniazid resistance, and 6% (28 of 440) for MDR TB. Patients with acquired resistance were significantly more likely than patients with primary resistance to have resistance to one or more of the three first-line drugs (prevalence rate ratio {PRR}=4.0; 95% confidence interval {CI}=2.8-5.7), to have isoniazid resistance (PRR=3.6; 95% CI=2.5-5.4), and to have MDR TB (PRR=12.4; 95% CI=4.8-32.3). Reported by: R Acosta Bermudez, P Acosta Blanco, G Anzaldo Flores, S Balandrano Campos, C Barron Rivero, D Casteneda Nava, P Contreras Ramos, A Flisser, MD, G Jaime Anzaldo, P Kuri Morales, MD, AR Marquez Fiol, MD, L Olivares Delgado, C Ruiz Matus, MD, AJ Santaella Solis, MD, JI Santos Preciado, MD, F Soriano Miranda, R Tapia Conyer, MD, Secretary of Health; A Zarate Aguilar, MD, IH Fernandez Garate, MD, JA Rivera, MD, J Navarrete Espinoza, MD, Mexican Institute of Social Security, Mexico City. JE Cornejo, MD, J Islas Torres, MD, D Ontiveros, MD, J Robledo Vasquez, MD, M Rodriguez Lomeli, MD, E Romo Rodriguez, A Zimbron, MD, ML Volcker, Baja California State Dept of Health. A Beltran Zazueta, MD, P Ferreiro Gastelum, MD, E Llausas Magana, S Pantoja Olvera, E Quinones Mejia, Sinaloa State Dept of Health. F Aguirre Gordillo, MD, MR Castellanos Morales, MD, P Diaz Garcia, MD, A Vasquez Hernandez, Oaxaca State Dept of Health. TB/Mycobacteriology Br, Div of AIDS, STD, and TB Laboratory Research, National Center for Infectious Diseases; International Activity, Div of Tuberculosis Elimination, National Center for HIV, STD, and TB Prevention; and an EIS Officer, CDC. Editorial NoteEditorial Note: This is the first population-based study of TB drug resistance from Mexico. Compared with results from 35 countries participating in the WHO/IUATLD global project on TB drug-resistance surveillance during 1994-1997, Mexico would have had the ninth highest level for primary resistance to at least one of the four first-line drugs (isoniazid, rifampin, ethambutol, and/or streptomycin) at 18% (pyrazinamide resistance was not evaluated). The United States ranked 14th with a level of 12% (2). In 1996, 8% of TB cases in the United States occurred in persons born in Mexico (5). The 1993-1996 U.S. surveillance data about persons with TB who were born in Mexico and the findings from the survey of persons born in Mexico described in this report indicate similar rates among patients for primary isoniazid resistance (9% and 11%, respectively) and primary MDR TB (2% and 2%, respectively) (6). The findings in this report are subject to at least three limitations. First, although surveillance for TB improved in the three surveyed states during the study period, the ability to assess data representativeness is limited by underreporting and notification delays. For example, the study in Oaxaca enrolled more patients than the number of persons officially reported as having smear-positive pulmonary TB. Second, 26% of the persons reported to the SSA with AFB smear-positive TB were not enrolled in the study, and 27% of the samples submitted could not be cultured. However, patients with positive cultures did not differ significantly from those with negative cultures by age or prior treatment history. Third, findings presented here are from only three of 31 states in Mexico and the Federal District; although the states are geographically dispersed, they may not be representative of the nation. The findings of this survey have lead to improved TB control in Baja California, Oaxaca, and Sinaloa. All three state laboratories now have implemented the capacity to culture for MTB. Although smears rather than cultures are recommended by WHO as the basis of initial TB diagnosis in countries with limited resources, the newly developed culture capacity in the three states will be useful in surveillance efforts and in the management of cases not responding to routinely recommended treatment regimens. In part as a result of this survey, the Secretary of Health of Mexico, in an effort to limit increases in drug resistance, is planning to initiate a four-drug treatment regimen by adding ethambutol to the current three-drug regimen. Four-drug regimens are recommended by CDC and the American Thoracic Society for communities with primary isoniazid resistance of greater than or equal to 4% (7). A second action to limit drug resistance that is being implemented by the Secretary of Health is to expand the DOTS program to the entire country. In addition to preventing the development of drug resistance, national strategies that are feasible in Mexico are needed to treat patients with MDR TB. As changes are made in the TB program, trends in MTB drug resistance will need to be monitored by implementing ongoing surveillance or performing periodic surveys. Further collaborative international efforts will be needed to improve TB control in the United States and Mexico. References
DOTS consists of 1) committing to a sustainable national TB program; 2) detecting cases among symptomatic patients self-reporting to health services, using smear microscopy; 3) administering standardized short-course chemotherapy with direct observation of treatment; 4) establishing a regular drug supply of essential anti-TB drugs; and 5) establishing and maintaining a standardized recording and reporting system that allows assessment of treatment results. Figure_1 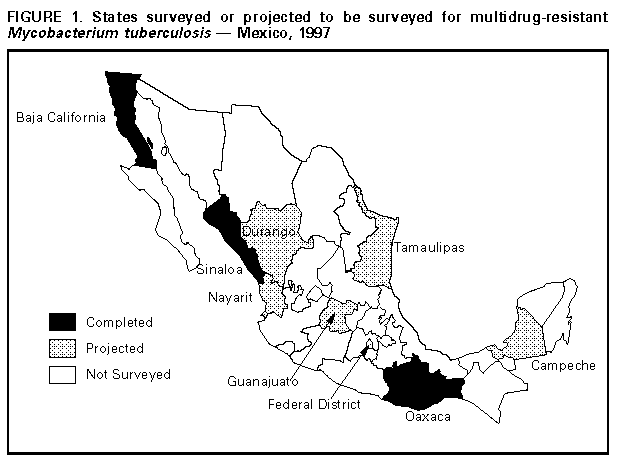 Return to top. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 1. Number of acid-fast bacilli smear-positive pulmonary tuberculosis (TB) cases,
number and percentage of enrolled patients with smear positive pulmonary TB, and
number and percentage of isolates recovered from those patients -- selected states,
Mexico, April-October, 1997
===============================================================================================
Patients enrolled in study Isolates recovered +
No. cases -------------------------- --------------------
State reported * No. (%) No. (%)
----------------------------------------------------------------------------------------
Baja California 351 298 ( 85) 216 (72)
Oaxaca 110 159 ( 100) & 104 (65)
Sinaloa 355 145 ( 41) 120 (83)
Total 816 602 ( 74) 440 (73)
----------------------------------------------------------------------------------------
* Source: Secretary of Health of Mexico.
+ Mycobacterium tuberculosis isolates available for drug susceptibility testing.
& Because of underreporting and reporting delays, some patients enrolled in the study may not
have been officially reported.
===============================================================================================
Return to top. Table_2 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 2. Number and percentage of sputum-smear positive pulmonary tuberculosis
(TB) patients with drug-resistant Mycobacterium tuberculosis isolates, by drug to
which the isolate was resistant and by TB treatment history + -- Baja California,
Oaxaca, and Sinaloa states, Mexico, April-October 1997
=====================================================================================================================
Previous treatment *
All cases ----------------------------------
(n=440) No + (n=308) Yes & (n=99)
---------- ------------ ------------- Prevalence
Drug No. (%) No. (%) No. (%) rate ratio @ (95% CI **)
------------------------------------------------------------------------------------------------------------------
Isoniazid 79 (18) 35 (11) 41 (41) 3.6 (2.4- 5.4)
Rifampin 37 ( 8) 7 ( 2) 27 (27) 12.0 (5.4-26.7)
Pyrazinamide 23 ( 5) 4 ( 1) 18 (18) 14.0 (4.9-40.4)
Ethambutol 24 ( 6) 9 ( 3) 14 (14) 4.8 (2.1-10.8)
Streptomycin 66 (15) 34 (11) 28 (28) 2.6 (1.6- 4.0)
Any first-line drug ++ 90 (21) 38 (12) 49 (50) 4.0 (2.8- 5.7)
Multidrug-resistant && 28 ( 6) 5 ( 2) 20 (20) 12.4 (4.8-32.3)
Five drugs @@ 10 ( 2) 2 ( 1) 8 ( 8) 12.4 (2.7-57.6)
------------------------------------------------------------------------------------------------------------------
* Patients with culture-positive TB for whom complete data about treatment history was
available; n=407.
+ Isolates from persons who reported no history of TB treatment are considered to have
primary drug resistance.
& Isolates from persons who reported a history of previous treatment with anti-TB drugs are
considered to have acquired drug resistance.
@ Rate in the previously treated group divided by the rate in the previously untreated group.
** Confidence interval for the prevalence rate ratio.
++ Resistance to Isoniazid, rifampin, or pyrazinamide.
&& Resistance to at least isoniazid and rifampin.
@@ Resistance to Isoniazid, rifampin, pyrazinamide, ethambutol, and streptomycin.
=====================================================================================================================
Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/05/98 |
|||||||||
This page last reviewed 5/2/01
|