 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Age-Specific Excess Deaths Associated with Stroke Among Racial/Ethnic Minority Populations -- United States, 1997Stroke was the third leading cause of death in the United States in 1997 (1). During 1950-1996, age-standardized stroke death rates declined 70% for the entire U.S. population (2); however, the decline varied among racial/ethnic populations (1). The estimated number of stroke deaths by race/ethnicity and age illustrate the differences in stroke mortality that may be used to direct prevention efforts. This report presents an analysis of stroke mortality by age and racial/ethnic group; the findings indicate that for persons aged 35-64 years, excess stroke deaths and higher risk for stroke mortality occurred among members of U.S. racial/ethnic minority populations than among the non-Hispanic white population. Excess death is the difference between the number of deaths observed in a racial/ethnic group and the number of deaths that would have occurred in that group if it had the same death rate as the non-Hispanic white population (3). Relative risk is the ratio of the stroke death rate of the minority group compared with that of the non-Hispanic white population accounting for differences in population size. The 1997 death certificate data were used to determine excess death and relative risk for stroke mortality by racial/ethnic group (non-Hispanic blacks, Hispanics, American Indians/Alaska Natives [AIs/ANs], and Asians/Pacific Islanders [As/PIs]) and by age group (35-44, 45-54, 55-64, 65-74, 75-84, and greater than or equal to 85 years). Non-Hispanic whites in each age group were the referent group. Observed stroke deaths were those for which the underlying cause of death listed on the death certificate by a physician, medical examiner, or coroner was International Classification of Diseases, Ninth Revision (ICD-9), codes 430-438. Demographics on death certificates (e.g., age, race, and ethnicity) are reported by funeral directors usually on the basis of observation or are provided by family members. National mortality statistics were based on information from death certificates filed in state vital statistics offices and were compiled by CDC (1). Expected deaths were calculated by multiplying the number of persons in each age-specific racial/ethnic group by the death rates in the corresponding non-Hispanic white group. Age-specific excess deaths were calculated by subtracting the observed deaths from the expected deaths for each age-specific group. Relative risks were calculated by dividing the death rate for each age-specific group by the corresponding death rate for non-Hispanic whites. The number of excess stroke deaths was largest for non-Hispanic blacks and As/PIs aged 35-84 years (6370 and 220, respectively) (Table 1); no excess stroke deaths occurred among non-Hispanic blacks and As/PIs for persons aged greater than or equal to 85 years. Hispanics and AIs/ANs aged 35-64 years had 242 and 41 excess stroke deaths, respectively; no excess stroke deaths occurred for Hispanics and AIs/ANs aged greater than or equal to 65 years. The relative risk for stroke mortality among racial/ethnic groups compared with non-Hispanic whites decreased with age (Figure 1). Non-Hispanic blacks had approximately four times the relative risk for persons aged 35-54 years, three times for persons aged 55-64 years, and approximately equal relative risk for persons aged greater than or equal to 85 years. AIs/ANs had almost twice the relative risk for stroke mortality than non-Hispanic whites among persons aged 35-44 years and 1.3 times for persons aged 45-64 years; the risk was lower among persons aged greater than or equal to 85 years. As/PIs had approximately 1.3 times the relative risk of stroke mortality among persons aged 35-64 years and a lower relative risk among persons age greater than or equal to 85 years. Among Hispanics, the relative risk for stroke death was approximately 1.3 times higher among persons aged 35-64 years, and approximately equal to non-Hispanic whites among persons aged greater than or equal to 65 years. Reported by: Cardiovascular Health Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion; and an EIS Officer, CDC. Editorial Note:The findings in this report highlight the excess number of stroke-related deaths among non-Hispanic black, AIs/ANs, As/PIs, and Hispanics compared with non-Hispanic white adults, especially among those aged 35-64 years. Excess deaths among racial/ethnic groups compared with non-Hispanic whites might be the result of greater prevalence of risk factors for stroke (e.g., obesity, uncontrolled hypertension, physical inactivity, poor nutrition, diabetes, and smoking) and other factors (e.g., lower socioeconomic status, predisposition for greater disease severity, and poor survival at younger ages) (4,5,7). Excess stroke deaths also may result from barriers to adequate medical care, including preventive, diagnostic, and therapeutic interventions (4) and health insurance coverage (5). Non-Hispanic blacks, As/PIs, and Hispanics have lower rates of health-care coverage than non-Hispanic whites (6); however, availability of health insurance or high-quality care does not indicate complete access to or use of medical care. Other barriers include lack of trust in the health-care system and fear of invasive medical procedures (5), transportation difficulties, and unfamiliarity with early warning signs of stroke (5). Despite progress in preventing and treating risk factors for stroke (e.g., increases in the use of antihypertensive therapy), the increasing prevalence of heart disease, diabetes, and obesity in the United States has increased the relative risk for stroke, particularly among blacks (4). Racial/ethnic differences in susceptibility to hemorrhagic and ischemic stroke subtypes are related strongly to uncontrolled high blood pressure and smoking (7). The increased frequency of intracerebral hemorrhages among blacks is attributable mostly to greater occurrence of hypertension (7). The greater number and severity of strokes in some racial/ethnic groups may be associated with differences in hypertension prevalence and control in all age groups (8). The data in this report are subject to at least four limitations. First, misclassification of race/ethnicity on death certificates and in the population census may result in understated reported death rates among AIs/ANs, As/PIs, and Hispanics. For the same reason, death rates for black and white populations may be overstated (9). Second, although variations among subpopulations may exist, the burden of stroke deaths is not shown for subgroups within the larger racial/ethnic groups. Third, the smaller sizes of populations of As/PIs and AIs/ANs can result in unstable estimates and produce overstated or understated death rates from year to year. Finally, this analysis did not control for stroke risk factors. Reducing stroke mortality among groups at highest risk largely depends on reaching them before unhealthy behaviors are adopted. Public health interventions can be community-based or can target persons at greatest risk. For example, in 1999, CDC began Racial and Ethnic Approaches to Community Health 2010 (REACH), community-based, culturally appropriate approaches to reduce cardiovascular disease and stroke among racial/ethnic populations. The national Brain Attack Coalition educates the public about the early warning symptoms of stroke to increase the likelihood of early diagnosis and prompt, effective treatment. Targeted research and evaluation among racial/ethnic populations may help identify differences among subpopulations related to lower socioeconomic or educational levels or related to adverse environmental factors. CDC is working with 11 state-based prevention and education programs that aim to reduce cardiovascular disease and stroke by improving nutrition, increasing physical activity, and promoting healthy behaviors. References
Table 1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size. TABLE 1. Excess deaths associated with stroke,* by race/ethnicity and age group -- United States, 1997
* International Classification of Diseases, Ninth Revision codes 430-438. Return to top. Figure 1 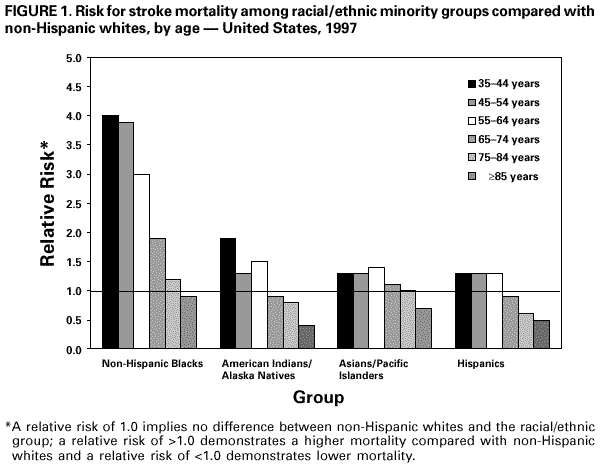 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 2/10/2000 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
This page last reviewed 5/2/01
|