 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Preliminary FoodNet Data on the Incidence of Foodborne Illnesses --- Selected Sites, United States, 1999Please note: An erratum has been published for this article. To view the erratum, please click here. Each year in the United States, an estimated 76 million persons experience foodborne illnesses (1). CDC's Emerging Infections Program Foodborne Diseases Active Surveillance Network (FoodNet) collects data on nine foodborne diseases in selected U.S. sites to quantify and monitor foodborne illnesses (2--4). This report describes preliminary surveillance data for 1999 and compares them with data from 1996--1998. The data suggest that the incidence of the foodborne illnesses under surveillance declined during 1999 compared with 1996 primarily as a result of decreases in campylobacteriosis and shigellosis and indicate substantial regional variation in the incidence of foodborne diseases (Figure 1). In 1996, active surveillance began for laboratoryconfirmed cases of Campylobacter, Escherichia coli O157, Listeria monocytogenes, Salmonella, Shigella, Vibrio, and Yersinia enterocolitica infections in Minnesota, Oregon, and selected counties in California, Connecticut, and Georgia. In 1997, surveillance for laboratoryconfirmed cases of Cryptosporidium and Cyclospora infections was added. In 1998, the surveillance area for Connecticut became statewide and active surveillance began in selected counties in Maryland and New York. In 1999, the remaining counties in Georgia and eight counties in the metropolitan Albany, New York, area were added, covering 25.6 million persons (1998 population estimate) (5). To identify cases, surveillance personnel contacted each clinical laboratory in their surveillance area either weekly or monthly depending on the size of the clinical laboratory. Cases represent isolation of a pathogen; most specimens were obtained for diagnostic purposes from ill persons. Duplicate isolations of the same pathogen from the same person within 1 year were excluded from the analysis. Preliminary 1999 incidence of pathogens was calculated using the number of cases of isolated pathogens that FoodNet had identified at clinical laboratories as the numerator and 1998 population estimates as the denominator (5). Final incidence will be available after 1999 population estimates are available. 1999 SurveillanceDuring 1999, 10,697 laboratory-confirmed cases of nine diseases under surveillance were identified: 4533 of salmonellosis, 3794 of campylobacteriosis, 1031 of shigellosis, 530 of E. coli O157 infections, 474 of cryptosporidiosis, 163 of yersiniosis, 113 of listeriosis, 45 of Vibrio infections, and 14 of cyclosporiasis. Among the 4095 Salmonella isolates serotyped, 982 (24%) were serotype Typhimurium, 403 (10%) were serotype Enteritidis (SE), 362 (9%) were serotype Newport, 284 (7%) were serotype Heidelberg, and 231 (6%) were serotype Muenchen; 405 (10%) of Salmonella isolates were untyped. Among the 949 Shigella isolates with a known species, 626 (66%) were S. sonnei and 295 (31%) were S. flexneri. For all reporting sites in 1999, incidence per 100,000 population was highest for salmonellosis (17.7), campylobacteriosis (14.8), and shigellosis (4.0). Substantial variation in incidence was observed among the sites for some pathogens (Figure 1). In 1999, the incidence of campylobacteriosis ranged from 6.6 in Maryland to 32.5 in California. Overall, salmonellosis incidence was similar (from 12.7 to 17.5) among all sites, except in Georgia where the incidence was 25.5. Rates for infections with specific Salmonella serotypes varied: infection with S. Typhimurium ranged from 2.0 in New York to 4.6 in Georgia, SE from 0.7 in New York to 4.0 in Maryland, and S. Newport from 0.2 in New York to 3.2 in Georgia. Incidence of shigellosis ranged from 1.7 in New York to 9.7 in California, E. coli O157 infections ranged from 0.6 in Georgia to 5.8 in New York, and yersiniosis varied from 0.3 in Connecticut and New York to 0.8 in Georgia and California. The incidence of cryptosporidiosis ranged from 0.3 in Maryland to 2.3 in Georgia. 1996--1999 Rate Comparison at Original FoodNet SitesFrom 1996 to 1999, the incidence of three laboratoryconfirmed infections under surveillance declined substantially in the five original FoodNet sites (Table 1). Over this period, the incidence of Campylobacter declined 26%, including 19% from 1998 to 1999; all states reported declines in Campylobacter rates. The incidence of shigellosis decreased 44% from 1996 to 1999; S. sonnei decreased 52% (from 6.4 to 3.1), and S. flexneri declined 25% (from 2.0 to 1.5). Rates of E. coli O157 infection decreased 22%. The overall incidence of salmonellosis decreased 15% from 1996 to 1998; however, the incidence increased 20% from 1998 to 1999. Compared with 1998 rates, 1999 rates for salmonellosis increased in Connecticut, Georgia, Minnesota, and Oregon, and declined in California. Rates for S. Typhimurium, the most common serotype, were constant from 1996 to 1999 (3.9 and 3.6, respectively). SE rates declined 48% from 1996 to 1999 with a 7% decline from 1998 to 1999. From 1998 to 1999, Salmonella infections with serotypes Muenchen, Newport, and Heidelberg increased 348%, 79%, and 44% respectively. The incidence of listeriosis, Vibrio infections, and yersiniosis were unchanged during the 4year period. Comparing the data on parasitic diseases from 1997 to 1999 (using only the sites reporting in all 3 years), rates of Cyclospora infections decreased 70% (from 0.3 to <0.1); rates of Cryptosporidium infection were constant from 1997 to 1999 (from 3.0 to 2.9). Reported by: S Shallow, MPH, M Samuel, DrPH, A McNees, MPH, G Rothrock, MPH, California Emerging Infections Program, D Vugia, MD, Acting State Epidemiologist, California Dept of Health Svcs. T Fiorentino, MPH, R Marcus, MPH, G Kazi, MPH, School of Medicine, Yale Univ, New Haven; P Mshar, M Cartter, MD, J Hadler, MD, State Epidemiologist, Connecticut State Dept of Public Health. M Farley, MD, S Desai, MPH, S Segler, MPH, Emory Univ School of Medicine, Atlanta; S Lance-Parker, DVM, P Blake, MD, Acting State Epidemiologist, Div of Public Health, Georgia Dept of Human Resources. M Pass, Johns Hopkins Univ School of Hygiene and Public Health, Baltimore; T Karchmer, MD, C Gregg, C Steiner, Univ of Maryland School of Medicine, Baltimore; M Carter, K Henning, J Razeq, A Glenn, Maryland Dept of Health and Mental Hygiene. K Smith, DVM, J Bender, DVM, J Besser, MS, D Soderlund, MS, K Moore, Minnesota Dept of Public Health. S Zansky, PhD, D Morse, MD, P Smith, State Epidemiologist, New York State Dept of Health. M Cassidy, T McGivern, E Lorber, B Shiferaw, MD, P Cieslak, MD, D Fleming, MD, State Epidemiologist, Health Div, Oregon Dept of Human Svcs. Office of Public Health and Science, Food Safety and Inspection Svc, Center for Food Safety and Applied Nutrition, Food and Drug Administration. Foodborne and Diarrheal Diseases Br, Div of Bacterial and Mycotic Diseases; Epidemiology Br, Div of Parasitic Diseases; and Office of the Director, National Center for Infectious Diseases; and an EIS Officer, CDC. Editorial Note:FoodNet data for 1999 indicate a decline in several major bacterial and parasitic causes of foodborne illnesses. Camplyobacter infections, the leading bacterial foodborne illnesses during 1996--1998, decreased in 1999 in all original FoodNet sites. SE, Shigella, and E. coli O157 cases also declined substantially. Decreases in the incidence of foodborne illnesses occurred concurrently with disease prevention efforts, including implementation of changes in meat and poultry processing plants, new requirements for food service establishments, and increased attention to good agricultural practices for produce and eggs on farms (6). From 1998 to 1999, although S. Typhimurium rates were steady and SE rates declined, salmonellosis rates increased in all original FoodNet sites except California. The reasons for the increased incidence of Salmonella infections are unclear. Salmonella can be acquired from foods of animal origin and foods contaminated with animal feces (7); however, in 1999, several large salmonellosis outbreaks were traced to produce vehicles, including unpasteurized orange juice (S. Muenchen) (8), mangos (S. Newport), and raw sprouts (S. Mbandaka). Controlling Salmonella requires prevention efforts among all food commodities. The decline in Shigella was largely restricted to S. sonnei, and followed an outbreak in 1998 traced to imported parsley (9), which increased attention to produce-associated shigellosis. The findings in this report are subject to several limitations. First, although FoodNet surveillance encompassed 9% of the U.S. population in 1999, these areas were not a nationally representative sample. Second, FoodNet data are limited to laboratory-confirmed illnesses; however, most foodborne illnesses are neither laboratory confirmed nor reported to state health departments. Third, some laboratory-confirmed illnesses reported to FoodNet can be acquired through nonfoodborne routes, such as water, person-to-person contact, and direct animal exposure; therefore, rates do not represent foodborne sources only. Further surveillance is necessary to determine whether changes represent year-to-year variation or definitive trends. In 2000, selected counties in Tennessee and Contra Costa County, California, will be added to the FoodNet area, bringing the FoodNet surveillance population to approximately 29 million persons---11% of the U.S. population (1998 estimates). The 1999 final FoodNet report will include incidence figures and other information, such as illness severity, and will be available later in 2000 at the FoodNet site on the World-Wide Web, http://www.cdc.gov/ncidod/dbmd/foodnet . Because the population within FoodNet sites probably has increased since 1998 (the increase from 1997 to 1998 was 1%), the final 1999 rates might be slightly lower than the preliminary rates. Additional analysis of FoodNet surveillance data, foodborne outbreak data (10), and surveys of clinical laboratories, health-care providers, and consumers will facilitate interpretation of FoodNet data and help track temporal trends in foodborne illnesses. References
Table 1 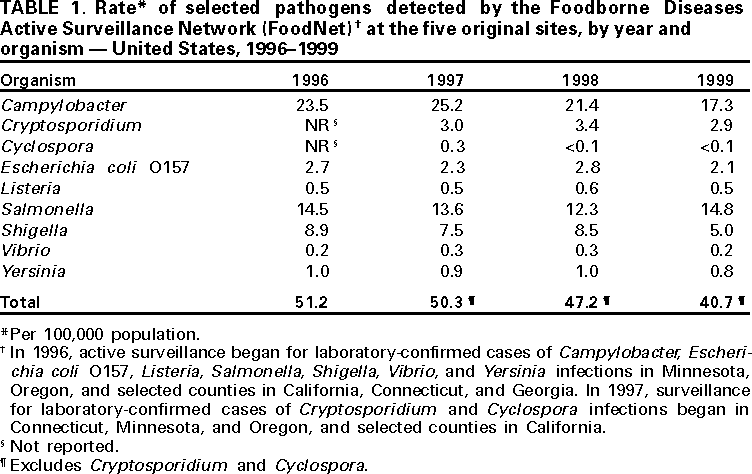 Return to top. Figure 1 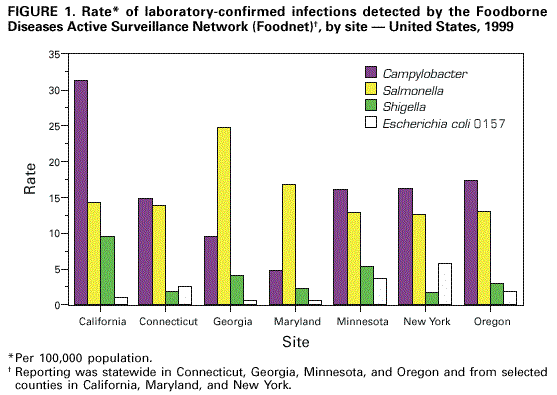 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 3/16/2000 |
|||||||||
This page last reviewed 5/2/01
|