 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreaks of Norwalk-like Viral Gastroenteritis --- Alaska and Wisconsin, 1999Norwalk-like viruses (NLVs) are the most common cause of epidemic gastroenteritis in the United States, resulting in illness in approximately 23 million persons each year (1,2). Persons of all ages are affected because previous infection confers only short-term immunity (3 ). Most NLV gastroenteritis outbreaks involve foodborne or person-to-person transmission. This report presents investigations of a foodborne NLV outbreak in Alaska and person-to-person transmission in Wisconsin. AlaskaOn November 10, 1999, a company in Anchorage notified the Alaska Division of Public Health that an estimated 20% of its 500 employees had called in sick. Ill workers reported signs and symptoms of acute gastroenteritis (AGE)---primarily nausea, diarrhea, and vomiting---following a restaurant-catered company luncheon on November 8. On November 11, questionnaires were e-mailed to 500 company employees; 456 (91%) were returned. A case was defined as nausea, vomiting, or diarrhea occurring in a company employee 1--96 hours after eating the restaurant food. Because the same batches of food served at the luncheon were available at the restaurant during the 4 days following the luncheon, 56 restaurant patrons were identified from credit card receipts to determine whether any were ill. Sanitarians investigated the restaurant facilities and interviewed foodhandlers. Stool samples were collected from ill luncheon attendees, foodhandlers, and ill restaurant patrons. Of 343 company employees who completed a questionnaire and ate luncheon food, 191 (56%) had an illness meeting the case definition. Among ill luncheon attendees, symptoms included nausea (87%), diarrhea (80%), abdominal pain (75%), chills (73%), vomiting (70%), and headache (65%). Illness onsets occurred a median of 33 hours after eating the lunch (range: 6--96 hours) (Figure 1), and the median duration of illness was 24 hours (range: 5--120 hours). Of 236 luncheon attendees who ate potato salad, 183 (78%) became ill. In addition, eight (89%) of nine restaurant patrons who responded ate potato salad and became ill. Among luncheon attendees, eating potato salad was associated strongly with illness (odds ratio=42.7; 95% confidence interval=18.6--101.7). The potato salad was prepared 2 days before the luncheon by two foodhandlers, one of whom was ill. The ill foodhandler used bare hands to mix the ingredients in a 12-gallon plastic container. Stool samples from 11 ill luncheon attendees, three foodhandlers, and two ill restaurant patrons were tested. No bacterial pathogens were isolated. Thirteen specimens tested at CDC by reverse transcriptase-polymerase chain reaction (RT-PCR) were positive for NLV: 10 from ill luncheon attendees, one from the ill foodhandler, and two from restaurant patrons. RT-PCR products from one luncheon attendee, one restaurant patron, and the implicated foodhandler had identical nucleotide sequences. WisconsinDuring November 30--December 1, 1999, seven students living on the same floor of a university residence hall with shared bathroom facilities developed signs and symptoms of AGE, including nausea, vomiting, and diarrhea. They were taken to local emergency departments. In conjunction with the Madison Department of Public Health and the Wisconsin Division of Public Health, the University Health Service initiated an investigation on December 1. All residents of the involved floor were administered a symptom, event, and food history questionnaire. A case of AGE was defined as vomiting or three or more loose stools within a 24-hour period in a hall resident during November 27--December 3. Specimen kits were distributed to all hall residents for stool sample collection. Of the 36 hall residents, all returned from Thanksgiving break during November 27--29. Nineteen (53%) of the residents had illnesses meeting the case definition. Signs and symptoms of illness among the case patients included fatigue (100%), vomiting (95%), chills (95%), body aches (84%), diarrhea (74%), abdominal cramps (63%), muscle aches (58%), headache (58%), and subjective fever (44%). The cases clustered in time into four groups (Figure 2). The probable index case-patient had multiple episodes of diarrhea and vomiting between 7 p.m. on November 28 and 6:30 a.m. on November 29. Twelve case-patients had illness onsets between noon on November 30 and noon on December 1 (secondary), five had illness onsets between noon on December 1 and noon December 2 (tertiary), and one had illness onset early in the morning of December 3. The mean illness duration was approximately 24 hours (range: 3.5--33 hours). None of the seven patients treated in emergency departments was hospitalized. No particular event, meal, food, or beverage was associated with illness. Only one person with a secondary case reported exposure to someone who was vomiting before illness onset. Three of the five persons with tertiary cases reported exposure to someone who was vomiting during the previous 36 hours. Stool specimens were obtained from eight case-patients. Seven were tested for bacterial pathogens at the Wisconsin State Laboratory of Hygiene (WSLH), and all were negative. Five of seven stool specimens tested at WSLH were positive by RT-PCR for NLV. The five positive specimens were obtained from the index case-patient, three from secondary case-patients, and one from a tertiary case-patient (Figure 2). The nucleotide sequences of RT-PCR products from four case-patients (the index case-patient and two secondary and the tertiary case-patients) were determined at CDC and were identical. Reported by: B Chandler, MD, Dept of Health and Human Svcs, Anchorage; M Beller, MD, S Jenkerson, MSN, J Middaugh, MD, State Epidemiologist, Alaska Dept of Health and Social Svcs. C Roberts, PA-C, Univ of Wisconsin Health Svcs, Madison; E Reisdorf, M Rausch, Wisconsin State Laboratory of Hygiene; R Savage, MS, Madison Dept of Public Health, Madison; J Davis, MD, State Epidemiologist, Wisconsin Div of Public Health. Viral Gastroenteritis Section, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases; and EIS officers, CDC. Editorial Note:These two outbreaks illustrate two principal modes of epidemic NLV transmission: consuming contaminated food and person-to-person transmission. In a study of 51 NLV outbreaks, modes of transmission included foodborne (excluding oysters) (37%), person-to-person (20%), consuming contaminated oysters (10%), waterborne (6%), and indeterminate (27%) (1). Person-to-person transmission, including direct contact, aerosol, and fomite exposure, generally has been reported in outbreaks involving elder-care settings, hospitals, or cruise ships (1,4). The low infectious dose of NLVs permits efficient transmission. The Alaska outbreak was associated with eating contaminated potato salad. In this outbreak, an ill foodhandler contaminated enough potato salad to cause illness in at least 200 persons. Evidence from the Wisconsin outbreak, particularly the grouping of cases, suggests that NLV was transmitted person-to-person. Because of the close living quarters and shared bathroom facilities, direct and fomite transmission most likely occurred. Less likely is that secondary case illnesses resulted from aerosol transmission of NLV; only one ill person reported exposure to someone who was vomiting. However, aerosol transmission may have contributed to subsequent NLV spread because three persons with tertiary cases reported exposure to secondary case-patients who were vomiting. Basic sanitary measures, such as diligent handwashing, can prevent foodborne transmission. In addition, ill workers should be excluded from food handling, and food preparers should minimize direct contact with ready-to-eat foods. Because improper food handling can result in large numbers of persons becoming ill, maintaining food-safety programs is an essential function of public health departments. Constant education of food handling staff and on-site inspections of food preparation facilities, including observation of food handling practices, are basic activities of effective food-safety programs. Populations in shared living arrangements, such as residence halls, are at greater risk for viral gastroenteritis acquired by person-to-person transmission. Residents in such facilities should use good hygienic practices, especially handwashing. Bathrooms should be kept visibly clean (5), and potentially contaminated areas should be cleaned as soon as possible after someone has been ill. References
Figure 1 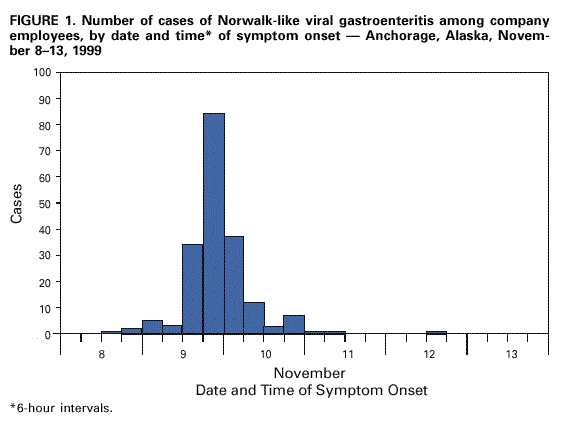 Return to top. Figure 2 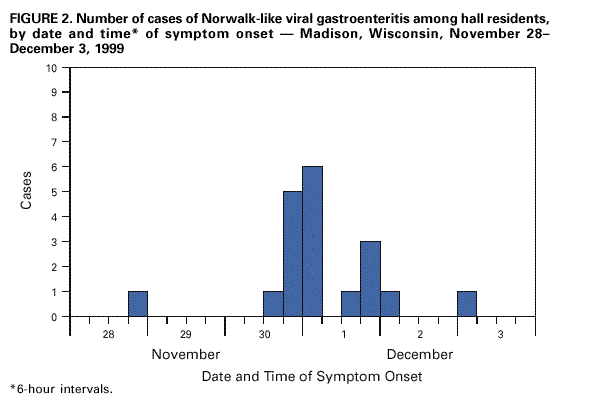 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 3/16/2000 |
|||||||||
This page last reviewed 5/2/01
|