 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Measles Outbreak ---- Netherlands, April 1999--January 2000On June 21, 1999, a cluster of five cases of measles was reported among the 390 students attending a religion-affiliated elementary school in the Netherlands. Persons belonging to this religious denomination routinely do not accept vaccination. Municipal health services (MHSs) investigated and found 160 suspected measles cases among children attending the school. By February 4, 2000, 2961 measles cases, includ ing three measles-related deaths, had been reported by 35 MHSs to the national registry. This report summarizes the investigation of the measles outbreak in the Netherlands, which indicated that measles can be a severe disease among unvaccinated populations in the Netherlands. Measles is a notifiable disease in the Netherlands, and cases that occurred during this outbreak were reported by physicians to the local MHS as part of routine surveillance. The vaccination status of ill persons was reviewed based on written records kept by reporting physicians and sent to the vaccination registry. In April 1999, the first cluster of measles cases occurred, followed by the reported elementary school outbreak in June. No cases of measles with onset in May were reported, and transmission was low during June and July (Figure 1). When schools reopened in August, the number of cases increased. The outbreak peaked during October--November, then decreased rapidly. As of February 4, the last reported cases had onset during the week of January 16. Since then, the number of reported cases has decreased substantially, suggesting that the outbreak is ending. From April 15, 1999, to February 4, 2000, 2961 cases of measles were reported in 35 (67%) of the country's 52 MHSs; 2317 (78%) were reported by 10 MHSs. All reporting municipalities have large communities affiliated with the religious group. Of the 105 case-patients tested for measles immunoglobulin type M, 100 (95%) had serologically confirmed measles. Complications among acute measles case-patients were assessed by telephone follow-up with reporting physicians; 510 (17%) cases had one or more complications and/or hospitalizations (Table 1). Three patients died as the result of measles complications: one child aged 2 years had an underlying cardiac disorder and subsequent cardiac failure, one child aged 3 years developed myocarditis, and one adolescent aged 17 years developed kidney failure and acute respiratory distress syndrome. Sixty-eight (2.2%) persons were reported hospitalized: 37 (1.2%) for pneumonia, seven (0.2%) for dehydration, five (0.2%) for encephalitis, four (0.1%) for high fever, three (0.1%) for shortness of breath, two (0.1%) for severe otitis media, two (0.1%) for croup, and six (0.2%) for other reasons. Two persons developed measles while hospitalized for other reasons. Of the 2882 patients whose ages were known, the median age was 6 years (range: 0--52 years): 95 (3%) were aged <1 year; 949 (33%), aged 1--4 years; 1282 (44%), aged 5--9 years; 382 (13%), aged 10--14 years; 87 (3%), aged 15--19 years; and 87 (3%), aged >20 years. Information on vaccination status was available for 2907 persons; 2770 (95%) were unvaccinated and 137 (5%) were vaccinated children. Of the 137, 117 (85%) were aged <9 years and all had received one dose of measles, mumps, and rubella vaccine (MMR); in 20 (15%) children the number of doses was unknown. Based on data from the national registry, 2749 persons whose ages were known were unvaccinated: 2317 (84%) persons eligible for vaccination were not vaccinated for religious reasons and 173 (6%) for other reasons (e.g., lack of concern about measles or concern about adverse events); 187 (7%) were not eligible for vaccination: 160 (85%) were aged <14 months (the recommended age for administration of the first dose of measles vaccine), 20 (11%) were born before 1976 (the year measles vaccination was introduced), and seven (4%) had a contraindication for measles vaccination. For the remaining 72 (3%) unvaccinated persons, the reason for not being vaccinated was unknown. In response to the outbreak in the Netherlands, on July 1, control activities were implemented, including 1) tracing contacts of cases, 2) offering vaccine or immunoglobu lin to susceptible contacts, 3) alerting all secondary-care and tertiary-care hospitals about the measles outbreak, 4) requesting general physicians to report all suspected cases, 5) conducting catch-up vaccination sessions at MHSs and mother and child clinics, 6) increasing media attention about undervaccination, and 7) urging parents to complete vaccination of children. Reported by: JE van Steenbergen, National Coordination Center for Communicable Disease Outbreak Management; S van den Hof, National Institute for Public Health and the Environment; MW Langendam, Municipal Health Svc, Amsterdam; JHTC van de Kerkhof, Municipal Health Svc, Zuid-Holland Zuid; WLM Ruijs, Municipal Health Svc, Rivierenland, Netherlands. Communicable Diseases and Immunization Unit, European Regional Office, World Health Organization (WHO), Copenhagen, Denmark; Vaccines and Biologicals Dept, WHO, Geneva, Switzerland. Respiratory and Enteric Viruses Br, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases; Vaccine Preventable Disease Eradication Div, National Immunization Program, CDC. Editorial Note: The three measles-related deaths and 68 hospitalizations that occurred among 2961 cases in the Netherlands indicate that measles can be severe and may result in death even in industrialized countries. Rates of complications reported in this outbreak are comparable with those in the United States and other industrialized countries (1). Measles notification and vaccination began in 1976 in the Netherlands, where measles epidemics have occurred every 5--7 years: 1976, 1983, 1988, 1992--1993, and 1999--2000. Since 1987, two doses of MMR have been recommended at age 14 months and 9 years. Measles vaccination is not mandatory for entry into school in the Netherlands. During 1997--1999, nationwide coverage of children for both doses was reported between 95% and 96% (2). However, coverage was not distributed uniformly throughout the country. In 1999, coverage ranged from 53% to 90% in municipalities that had a high percentage of residents who were members of a particular group that refrains from vaccination on religious grounds (2). This community in the Netherlands, estimated at 300,000 persons (2% of the overall population) lives as a close social network in a circumscribed geographic area mostly in the provinces of Gelderland, Utrecht, Zuid-Holland, and Zeeland. Approximately half of the 4%--5% of unvaccinated persons in the Netherlands are members of this group. Although the Netherlands has high overall MMR coverage, 36 (7%) of 539 municipalities have one-dose coverage of <90%. Although measles is more severe in malnourished or immunosuppressed persons, severe disease or death may result in persons with no underlying illness. Measles vaccine is a highly effective method for preventing this disease, and lack of vaccination resulted in this outbreak. Similar to the outbreak of poliomyelitis among religious communities in 1992 (3,4), measles spread from the Netherlands to Canada through visiting relatives. The resulting outbreak in Canada was limited to 17 cases within the religious community possibly because stringent control measures were taken (5). Until measles is eradicated worldwide, epidemics will continue to occur periodically in the Netherlands. The World Health Organization (WHO) has established goals to eliminate measles as an indigenous disease from the Region of the Americas by the end of 2000, the European Region by 2007, and the Eastern Mediterranean Region by 2010. To reach these goals, the WHO regional office for Europe has conducted workshops aimed at assisting participating countries to develop an elimination strategy based on the percentage of persons susceptible to measles in their population. In addition to these activities, increased commitment at the regional and national levels is needed to eliminate measles in the European Region (6). References
Table 1 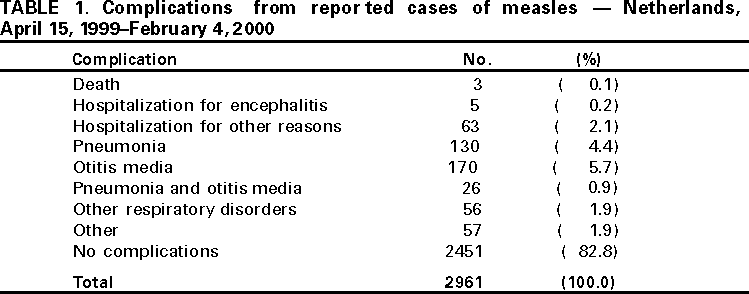 Return to top. Figure 1 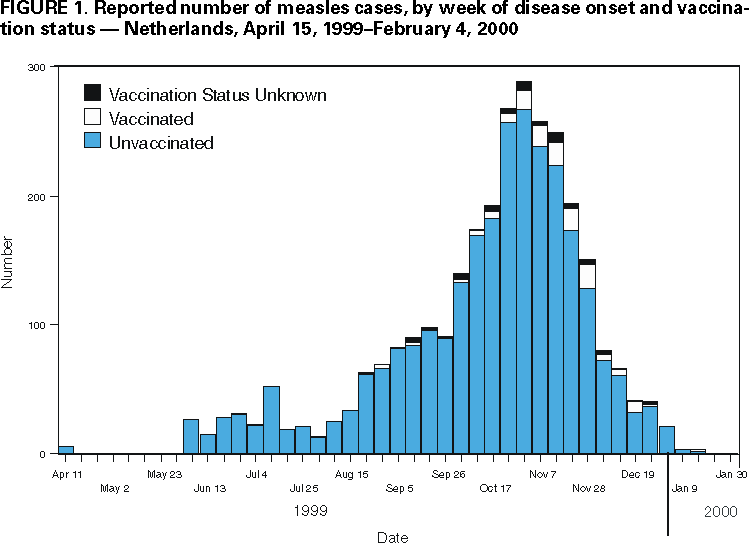 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 4/13/2000 |
|||||||||
This page last reviewed 5/2/01
|