 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Update: Clostridium novyi and Unexplained Illness Among Injecting-Drug Users --- Scotland, Ireland, and England, April--June 2000Since April 19, 2000, health authorities in Scotland, Ireland, England, and the United States have been investigating an outbreak of unexplained illness and death among injecting-drug users (IDUs) in the United Kingdom and Ireland (1--3). Initial testing of specimens from 76 IDUs identified Clostridium species in 18 (24%) patients; nine were Clostridium novyi. This report updates the investigation of this outbreak, which indicates that Clostridium species may be associated with these illnesses. During April 1--June 19, investigators identified 88 IDUs in Scotland (n=48), Ireland (n=19), and England (n=21) with injection-site soft tissue inflammation resulting in hospitalization or death; 40 (45%) have died. Thirty-five (40%) patients had illnesses that met the syndrome-based case-definition (1), including sustained hypotension and markedly elevated white blood cell count (WBC), or postmortem evidence of a diffuse toxic or infectious process, with initial hospitalization during April 11--June 6 (Figure 1). The median age of the 35 case-patients was 32 years (range: 20--51 years); 18 (51%) were men, and 34 (97%) died. Median peripheral WBC was 63,600 cells/mm3 (range: 8,200--153,000 cells/mm3). In Ireland, cases remained limited to Dublin, and in Scotland cases have been reported from both the Glasgow and Aberdeen areas. In England, most cases have been identified in and around Manchester, but several cases have been reported from other parts of the country. Among the 35 patients with illnesses meeting the case definition, nine (26%) have laboratory evidence of clostridial infections based on culture isolation or 16S ribosomal DNA polymerase chain reaction and sequencing performed on blood or tissue, including three C. novyi, three C. perfringens, one with both C. novyi and C. perfringens, and two clostridial species awaiting further typing. Of the remaining 41 patients with illnesses who failed to meet the case definition but who may be linked to this outbreak, and for whom data are available, nine (22%) have evidence of clostridial infections, including five C. novyi and four with species pending. Although the role of other pathogens requires further delineation, only four (11%) patients with illnesses meeting the case definition have evidence of other etiologic agents (Staphylococcus aureus, group A Streptococcus, and group C Streptococcus), compared with 12 (29%) of 41 patients with unexplained soft tissue infections but lacking severe systemic toxicity. Reported by: S Ahmed, MD, L Gruer, MD, C McGuigan, MD, G Penrice, MD, K Roberts, MPhil, Dept of Public Health, Greater Glasgow Health Board; J Hood, MD, Dept of Microbiology, Glasgow Royal Infirmary; P Redding, MD, Dept of Microbiology, Victoria Infirmary Glasgow; G Edwards, MD, Stobhill General Hospital; M Black, MD, J McFarlane, MD, Dept of Forensic Pathology, Univ of Glasgow; D Cromie, MD, Dept of Public Health, Lanarkshire Health Board; H Howie, MD, Dept of Public Health, Grampian Health Board; A Leonard, MD, Dept of Microbiology, Monklands Hospital; D Goldberg, MD, A Taylor, PhD, S Hutchinson, MSc, K Roy, PhD, S Wadd, PhD, R Andraghetti, MD (EPIET), Scottish Center for Infection and Environmental Health, Glasgow, Scotland. J Barry, MD, G Sayers, MD, M Cronin, MD, T O'Connell, MD, M Ward, MD, P O'Sullivan, MD, B O'Herlihy, MD, Eastern Regional Health Authority, Dept of Public Health; E Keenan, MD, J O'Connor, MD, L Mullen, MSc, B Sweeney, MD, Eastern Regional Health Authority Area Health Boards' Drug Svcs; D O'Flanagan, MD, D Igoe, MD, National Disease Surveillance Center; C Bergin, MD, S O'Briain, MD, C Keane, MD, E Mulvihill, MD, P Plunkett, MD, G McMahon, MD, T Boyle, MD, S Clarke, MD, St. James's Hospital; E Leen, MD, James Connolly Memorial Hospital; M Cassidy, MD, State Pathology Svc, Dublin, Ireland. T Djuretic, MD, N Gill, MD, V Hope, PhD, J Jones, MD, G Nichols, PhD, A Weild, MPhil, Public Health Laboratory Svc (PHLS) Communicable Disease Surveillance Centre; R George, MD, PHLS Respiratory and Systemic Infection Laboratory; P Borriello, PhD, PHLS Central Public Health Laboratory, London, England; J Brazier, PhD, J Salmon, MD, PHLS Anaerobe Reference Unit, Cardiff, Wales; N Lightfoot, MD, PHLS North, Newcastle; A Roberts, PhD, Centre for Applied Microbiology and Research, Porton Down, England. Infectious Diseases Pathology Activity, Div of Viral and Rickettsial Diseases; Bioterrorism Preparedness and Response Program; Meningitis and Special Pathogens Br, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; and EIS officers, CDC. Editorial Note:Although clostridial species have been implicated previously in clusters of wound infections among IDUs (4,5), the number of cases and severity of illness associated with this outbreak appear to be unique. C. perfringens can produce fulminant shock through direct toxogenic effects on myocardial contractility, but this organism usually causes extensive tissue destruction and gas production, features that are not prominent in the current cases (6). C. sordellii can also cause a distinctive, toxin-mediated illness characterized by tissue edema, myonecrosis, leukemoid reaction and sudden onset of shock (7). However, perhaps because of its fastidious and strict anaerobic growth requirements (6), C. novyi has been less commonly implicated in such a clinical syndrome. The significance of isolating clostridial species from the tissue of the patients described in this report remains unclear, but the presence of these organisms suggests soil or fecal contamination of the drugs or other materials used by these IDUs and may provide the causative explanation for their illnesses. Clinical, epidemiologic, and laboratory investigations continue to characterize these illnesses, confirm the role of C. novyi as one of the potential etiologic agents, identify risk factors for disease, and implement measures to prevent further cases. Surveillance activities to identify additional cases in the United Kingdom and Ireland are ongoing, and efforts to find cases in the rest of Europe or the United States have been expanded. Health-care providers and public health personnel are encouraged to report persons with illnesses meeting the case definition to their designated public health authorities. References
Figure 1 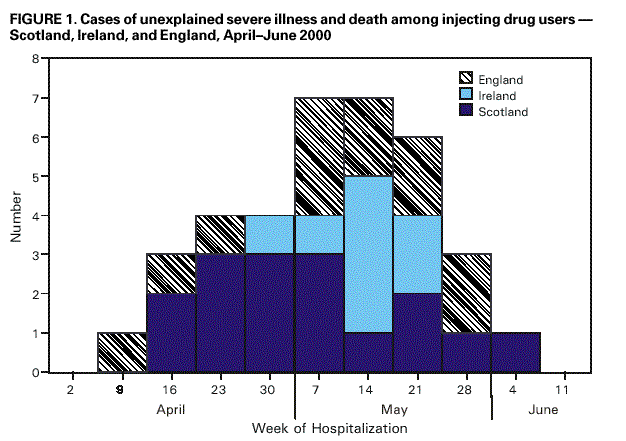 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 6/22/2000 |
|||||||||
This page last reviewed 5/2/01
|