 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. State-Specific Cholesterol Screening Trends --- United States, 1991--1999High blood cholesterol (HBC) increases the risk for heart disease, the leading cause of death in the United States. To reduce the prevalence of HBC in the United States, the National Heart, Lung, and Blood Institute initiated the National Cholesterol Education Program (1) in 1985 and recommended that all adults aged >20 years have their cholesterol levels checked at least once every 5 years. One of the national health objectives for 2000 was to increase to 75% the proportion of adults aged >20 years screened for HBC during the preceding 5 years (objective 15.14) (2). This objective was revised for 2010 to recommend that 80% of adults in this age group be screened during the preceding 5 years (3). To monitor progress during the 1990s and to determine whether the 2000 objective was attained, data from CDC's Behavioral Risk Factor Surveillance System (BRFSS) were used to examine the state-specific trends in cholesterol screening from 1991 through 1999. This report summarizes the results of this analysis and provides a projected estimate of the 2010 screening rates for HBC in each state. The findings indicate that few states attained the 2000 objective and that more emphasis on cholesterol screening will be needed to attain the 2010 objective. BRFSS is a random-digit--dialed telephone survey of the noninstitutionalized U.S. population aged >18 years. For this study, BRFSS data from 1991, 1993, 1995, 1997, and 1999 were analyzed for 563,742 persons aged >20 years from 50 states and the District of Columbia (DC). Survey participants were asked whether they had ever had their blood cholesterol checked and, if so, when they had last had it checked. Persons who reported that they had been screened during the preceding 5 years were classified as having been screened for HBC. Data were weighted to account for the age, race, and sex distribution in each state. SUDAAN 7.0 was used to account for the complex sampling design and to achieve accurate variance estimates. A state-specific method and an aggregate method were used to project the prevalence of cholesterol screening during 2010. The state-specific method was limited to DC and the 47 states that participated in BRFSS from 1991 through 1999; for each state, the 9-year change in the percentage of adults screened for HBC during 1991--1999 was added to that state's 1999 value to project the 2010 screening rate. The aggregate method added the median 9-year change in cholesterol screening among all states combined from 1991 through 1999 to the state-specific 1999 cholesterol screening value for each of the 50 states and DC. In the 47 states and DC that participated in BRFSS from 1991 through 1999, the proportion of adults screened for HBC increased from 67.3% in 1991 to 70.8% in 1999 (Table 1). The estimated state-specific cholesterol screening rate increased for DC and 40 states, ranging from a 0.4% increase in Idaho to an 11.6% increase in Arizona (median: 3.6%). For seven states, the screening rate declined during 1991--1999. DC (80%) and nine states (Arizona [76%], Connecticut [76%], Delaware [75%], Florida [76%], Maryland [77%], Massachusetts [77%], New Jersey [76%], North Carolina [75%], and Rhode Island [76%]) attained the 2000 objective in 1999. On the basis of state-specific increases, the projected 2010 screening rates ranged from 51.5% (Minnesota) to 91.7% (DC), and projected screening rates for seven states and DC were greater than the 2010 objective of 80%. On the basis of a median increase of 3.6%, the projected screening rates ranged from 64.0% (Minnesota) to 84.0% (DC), and projected screening rates for five states and DC are greater than the 2010 objective (Figure 1). Reported by the following BRFSS coordinators: S Reese, MPH, Alabama; P Owen, Alaska; B Bender, MBA, Arizona; G Potts, MBA, Arkansas; B Davis, PhD, California; M Leff, MSPH, Colorado; M Adams, MPH, Connecticut; F Breukelman, Delaware; I Bullo, District of Columbia; S Hoecherl, Florida; L Martin, MS, Georgia; F Reyes-Salvail, MS, Hawaii; J Aydelotte, MA, Idaho; B Steiner, MS, Illinois; L Stemnock, Indiana; J Davila, Iowa; C Hunt, Kansas; T Sparks, Kentucky; B Bates, MSPH, Louisiana; D Maines, Maine; A Weinstein, MA, Maryland; D Brooks, MPH, Massachusetts; H McGee, MPH, Michigan; N Salem, PhD, Minnesota; D Johnson, MS, Mississippi; J Jackson-Thompson, PhD, Missouri; P Feigley, PhD, Montana; L Andelt, PhD, Nebraska; E DeJan, MPH, Nevada; L Powers, MA, New Hampshire; G Boeselager, MS, New Jersey; W Honey, MPH, New Mexico; C Baker, New York; Z Gizlice, PhD, North Carolina; L Shireley, MPH, North Dakota; P Pullen, Ohio; K Baker, MPH, Oklahoma; K Pickle, MPH, Oregon; L Mann, Pennsylvania; J Hesser, PhD, Rhode Island; M Wu, MD, South Carolina; M Gildemaster, South Dakota; D Ridings, Tennessee; K Condon, MS, Texas; K Marti, Utah; C Roe, MS, Vermont; K Carswell, MPH, Virginia; K Wynkoop Simmons, PhD, Washington; F King, West Virginia; K Pearson, Wisconsin; M Futa, MA, Wyoming. Cardiovascular Health Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report indicate that the overall percentage of U.S. adults who received cholesterol screening during the 5 years preceding the survey increased during the 1990s. However, these increases were moderate, and most states did not attain the 2000 health objective. Data from the 1988--1991 BRFSS projected that 31 of 47 states (Kansas, Nevada, and Wyoming were excluded) and DC would have cholesterol screening rates greater than the 2000 objective (4). However, this report indicates that nine of 50 states and DC attained a cholesterol screening rate of >75% in 1999. In addition, 14 states had at least a 10% difference between the 2010 objective of 80% and the 2010 projected screening rates using the state-specific method. This finding suggests that these states will need to substantially increase cholesterol screening rates to attain the 2010 objective. The trend of decreasing cholesterol screening rates in seven states is of particular concern. In the 1988--1991 BRFSS analysis (4), all states had increases in cholesterol screening rates. Changes in the sampling frame or weighting protocol within a state during the 9 years may have contributed to the decline. However, response rates did not appear to explain the decreases, and changes in the questionnaire would be expected to affect all states rather than a select few. Other factors that may be associated with declining cholesterol screening rates within a community include lower perception of the risk for heart disease and the protective effect of reducing cholesterol levels, lack of availability of quality health care, and fewer socioeconomic resources (5). The nine states that achieved the 2000 objective in 1999 and Arizona, Massachusetts, and North Carolina participate in CDC's WISEWOMAN (Well-Integrated Screening and Evaluation for Women Across the Nation) demonstration program, which provides cholesterol screening and other services to some participants in the National Breast and Cervical Cancer Early Detection program (6). In addition, several local health departments in Connecticut conducted cholesterol screening during the 1990s under block grant funding, and four Healthy Heart program initiatives were funded in New Jersey during 1990--1996 (M. Adams, Connecticut, G. Boeselager, New Jersey, BRFSS coordinators, personal communication, 2000). The findings in this report are subject to at least two limitations. First, because BRFSS is telephone-based, persons of low socioeconomic status are less likely to have a telephone and may not have been included. Second, data are self-reported. As a result, some participants may not have been aware they were screened for elevated cholesterol. HBC is a major modifiable risk factor for heart disease. A 10% decrease in cholesterol levels may result in an estimated 30% reduction in the incidence of coronary heart disease (7). Cholesterol screening is an important step in reducing the prevalence of elevated cholesterol levels and serves several purposes including 1) assessing persons with heart disease risk; 2) identifying persons who may achieve lower cholesterol levels through dietary modification, physical activity, weight control, or drug treatment; and 3) heightening public awareness and reinforcing educational messages (8). Substantial progress has been made in lowering cholesterol levels since the mid-1980s (1); however, the findings of this report suggest that increased emphasis on cholesterol screening is necessary if states are to achieve the 2010 objective. References
Table 1   Return to top. Figure 1 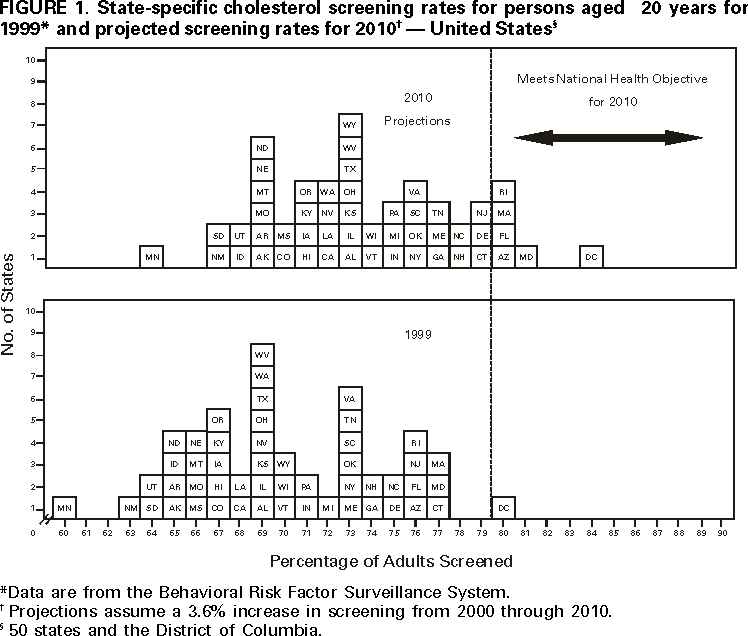 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 8/24/2000 |
|||||||||
This page last reviewed 5/2/01
|