 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Human Ingestion of Bacillus Anthracis-Contaminated Meat --- Minnesota, August 2000On August 25, 2000, the Minnesota Department of Health (MDH) was notified by the Minnesota Board of Animal Health (MBAH) of Bacillus anthracis isolated from a steer on a farm in Roseau County, Minnesota. The infected steer was one of five dead cattle found in a pasture on August 20. On the basis of phage typing of isolates cultured from tissues and blood samples by the North Dakota State University Veterinary Diagnostic Laboratory, B. anthracis was confirmed. This report describes the management of and public health response to human exposure to meat contaminated with anthrax. On July 24, the farmer who owned the infected steer also had killed, gutted, and skinned a cow that was unable to rise. A local veterinarian approved the slaughter of the cow for consumption by the farmer's family. Immediately after slaughter, the farmer took the carcass (carcass X) to a custom meat-processing plant; on July 31 and August 1, carcass X was processed. Two family members ate hamburgers made from carcass X on August 15 and steaks on August 19; three other family members ate hamburgers on August 20. A sixth member prepared the meals and also may have eaten contaminated meat. All meat was reported to have been well cooked. To investigate the possibility that they had eaten contaminated meat, the family members were interviewed by MDH on August 25. Two reported gastrointestinal illness; one reported 1 day of diarrhea approximately 48 hours after eating meat from carcass X, and the second reported 3 days of abdominal pain, diarrhea, and a temperature of 102.3 F (39.1 C) beginning 24--36 hours after consumption. Both recovered without treatment. The family was advised by MDH not to eat any more of the meat, to contact a physician, and to begin antibiotic prophylaxis with ciprofloxacin (500 mg, orally, twice daily). On August 29, samples of carcass X tested by the MDH Public Health Laboratory (MDH PHL) were found to contain gram-positive bacilli on microscopic examination. B. anthracis contamination was confirmed at MDH PHL and the U.S. Army Medical Research Institute for Infectious Diseases through culture on blood agar, presence of a capsule, lack of motility, gamma-phage test, and fluorescent antibody to cell wall polysaccharide and capsular antigens. On the basis of this exposure to meat highly contaminated with B. anthracis, the family was advised to continue chemoprophylaxis, and vaccination with anthrax vaccine was initiated (Anthrax Vaccine Adsorbed*, Bioport Corporation, Lansing, Michigan). The Minnesota Department of Agriculture (MDA) contacted the custom meat processing plant on August 28 and placed a hold on all meat processed after carcass X. On August 29, MDA inspected the plant; sanitation practices were satisfactory. Seven carcasses had been processed after carcass X. Owners of meat from the carcasses were advised not to eat any of the meat and were asked to return meat to a central location for incineration; all the meat products were accounted for and none had left Minnesota. Samples from the other carcasses and environmental swabs collected after plant cleaning tested negative for B. anthracis. Reported by: H Kassenborg, DVM, R Danila, PhD, P Snippes, MT(ASCP), M Wiisanen, M Sullivan, MPH, KE Smith, DVM, N Crouch, PhD, C Medus, MPH, R Weber, MS, J Korlath, MPH, T Ristinen, R Lynfield, MD, HF Hull, MD, Minnesota Dept of Health. J Pahlen, Roseau County Home Health Care, Roseau; T Boldingh, DVM, Minnesota Board of Animal Health, K Elfering, G Hoffman, Minnesota Dept of Agriculture, St. Paul. T Lewis, A Friedlander, MD, H Heine, PhD, R Culpepper, MD, E Henchal, PhD, G Ludwig, PhD, C Rossi, MS, J Teska, PhD, J Ezzell, PhD, E Eitzen, MD, US Army Medical Research Institute for Infectious Diseases. Food Safety and Inspection Svc, Animal and Plant Health Inspection Svc, US Dept of Agriculture. Epidemiology Program Office, Meningitis and Special Pathogens Br, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; and an EIS Officer, CDC. Editorial Note:Anthrax is a zoonotic disease caused by the spore-forming bacterium B. anthracis. Human disease usually occurs through cutaneous exposure to infected animal tissue or products. Rarely, inhalation or ingestion of B. anthracis spores also leads to anthrax. In the United States during the early part of the 20th century, approximately 130 human cases occurred annually (1); two cutaneous infections have been reported since 1992. Before this exposure, no animal anthrax cases had been reported in northern Minnesota since recordkeeping began in 1909. However, in adjacent areas of North Dakota during 2000, 120--150 cattle have died of anthrax (L. Schuler, North Dakota state veterinarian, personal communication, 2000), and 11 farms have reported anthrax-related cattle deaths in nearby Manitoba, Canada (Figure 1) (J.G. Spearman, Manitoba Department of Agriculture, personal communication, 2000). Gastrointestinal anthrax in humans occurs 1--7 days after eating raw or undercooked meat from infected animals (2), and two forms of gastrointestinal disease have been reported (3). Disease affecting the distal gastrointestinal tract results in nausea, anorexia, and fever followed by abdominal pain and bloody stool. The case fatality rate among reported cases ranges from 25%--60% (2). Gastrointestinal anthrax never has been documented in the United States because livestock are vaccinated for anthrax in areas where the disease is endemic; animals routinely are inspected by federal and state meat inspectors before, during, and after slaughter; and raw meat is eaten infrequently. Anthrax has not been documented among the persons exposed to B. anthracis-contaminated meat described in this report; however, a serologic test to determine presence of infection is pending. Limited experience with gastrointestinal anthrax complicates recommendations for use of postexposure prophylaxis. An extended duration of therapy is recommended for inhalational exposure because of the persistence of spores resistant to the action of antimicrobial agents (4,5). Upon cessation of chemoprophylaxis, such spores can cause disease several weeks after exposure. No evidence supports the existence of persistent spores associated with gastrointestinal forms of the disease; however, the meat consumed by the family in this report was highly contaminated with B. anthracis. Although possible interventions range from close observation to antibiotics alone to antibiotics with vaccination, because the family was at high risk for anthrax infection, management consisted of an extended course of ciprofloxacin combined with administration of anthrax vaccine. Federal-inspected and state-inspected animal processing facilities are required to perform intensive cleaning after contact with an anthrax-infected carcasses† ; veterinary inspection is not provided at custom meat processors. Slaughter house workers who may be exposed to an anthrax-contaminated carcass should receive medical evaluation for symptoms and for possible treatment. Management of anthrax in livestock should include 1) quarantine of the herd; 2) removal of the herd from the contaminated pasture, if possible; 3) vaccination of healthy livestock; 4) treatment of symptomatic livestock; and 5) disposal of infected carcasses, preferably by burning. Bedding and other material found around the carcass (e.g., soil) should be incinerated with the carcass and buried (6). Veterinarians notified of sudden death in an animal or of an animal unable to rise should consider anthrax as a diagnosis, especially in areas where anthrax is endemic (6). However the potential risk for animal anthrax exists in all areas of the United States. Vaccination of livestock in areas where anthrax is endemic is the most effective method of prevention in animals and humans. Cases of anthrax in animals and cases of suspected human exposure should be reported immediately to the state health department, federal animal heath officials, and to CDC's National Center for Infectious Diseases, Meningitis and Special Pathogens Branch, telephone (404) 639-3158. References
* Use of trade names and commercial sources is for identification only and does not constitute endorsement by CDC or the U.S. Department of Health and Human Services. † 9 CFR Part 310.9 (2000). Figure 1 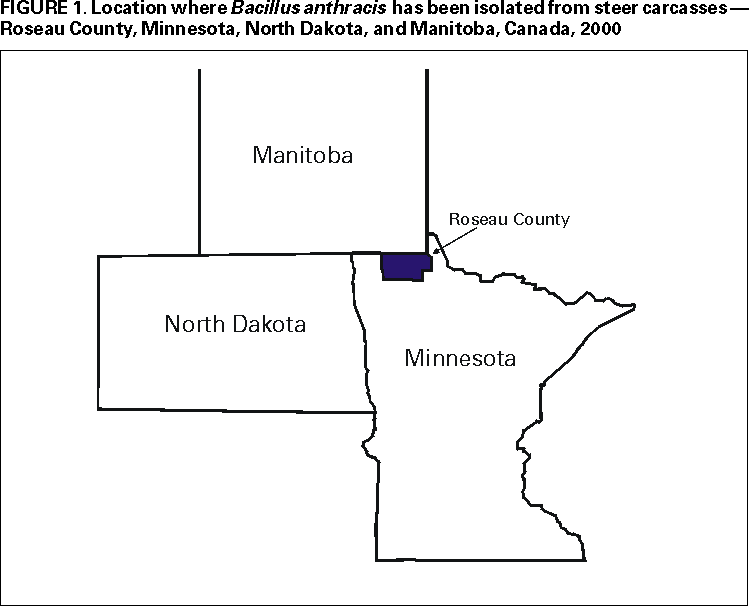 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 9/14/2000 |
|||||||||
This page last reviewed 5/2/01
|