 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Consequences of Delayed Diagnosis of Rocky Mountain Spotted Fever in Children --- West Virginia, Michigan, Tennessee, and Oklahoma, May--July 2000Patients with Rocky Mountain spotted fever (RMSF), a tickborne infection caused by Rickettsia rickettsii, respond quickly to tetracycline-class antibiotics (e.g., doxycycline) when therapy is started within the first few days of illness; however, untreated RMSF may result in severe illness and death. Persons aged <10 years have the highest age-specific incidence of RMSF (1,2). This report summarizes the clinical course and outcome of RMSF in four children from four regions of the United States and underscores the need for clinicians throughout the United States to consider RMSF in children with rash and fever, particularly those with a history of tick bite or who present during April--September when approximately 90% of RMSF cases occur (1,2). West VirginiaOn May 12, a child aged 15 months presented to a physician with a 2-day history of maculopapular rash and fever. A tick had been removed from the patient's scalp 1 week before onset of symptoms. The patient was thought to have a viral illness. On May 16, the patient returned to the physician with continued fever and irritability; an allergy to a sulfa-containing antimicrobial prescribed on the previous visit was suspected, and treatment was switched to an oral penicillin-class antibiotic. On May 17, the patient was seen twice at a local emergency department (ED) and, by the second visit, exhibited lethargy, seizures, a generalized petechial rash, hyponatremia (131 mmol of sodium/L) (normal range: 135--145 mmol/L), and thrombocytopenia (8 x 109 platelets/L) (normal range: 150--350 x 109/L). The patient was transported to a tertiary medical center with a differential diagnosis of bacterial sepsis, meningitis, or a rickettsial disease and immediately was started on intravenous doxycycline. Shortly after admission, the patient required intubation for respiratory distress and anticonvulsant therapy for seizures. On May 19, the patient died. Paired serum samples demonstrated a four-fold increase (from 80 to 320) in reciprocal IgM antibody titers reactive with R. rickettsii when tested using an indirect immunofluorescence assay (IFA). When stained by using an immunohistochemical (IHC) technique, tissue samples obtained at autopsy demonstrated spotted fever group rickettsiae. MichiganOn June 1, a child aged 3 years presented to a physician with a 4-day history of rash and a temperature of 101.3 F (38.5 C). On clinical examination, the patient had a fine red-purple rash on the cheeks, trunk, upper extremities, and palms, thrombocytopenia (102 x 109/L), and a normal white blood cell (WBC) count (5.8 cells x 109/L). The patient's mother reported that she recently had found a tick on the patient's scalp. The patient was diagnosed with a viral exanthem. On June 2, the patient was still febrile but the rash had faded, and the patient was given an oral cephalosporin-class antibiotic. On June 5, the patient developed vomiting, decreased appetite, persistent crying, and disorientation. The patient's mother reported that she had removed a second tick that day. Clinical examination revealed generalized petechiae, hepatosplenomegaly, dry mucous membranes, and pallor. Laboratory findings included thrombocytopenia (38 x 109/L), an elevated WBC count (19 x 109/L), hyponatremia (124 mmol/L), elevated aspartate aminotransferase (AST 7.20 µkat/L) (normal range: 0.17--0.67 µkat/L), and alanine aminotrans ferase (ALT 1.63 µkat/L) (normal range: 0.17--0.92 µkat/L). The patient was admitted to a hospital, and within several hours the patient became cyanotic, developed seizures, and died. Using an IHC stain, tissue samples obtained at autopsy revealed spotted fever group rickettsiae. Using a polymerase chain reaction assay, a whole blood sample was positive for DNA of R. rickettsii. TennesseeOn June 15, a child aged 11 years presented to an ED with a 1-day history of severe headache and a temperature of 102.4 F (39.1 C). On clinical examination, an injected tympanic membrane was found, and the patient received an oral penicillin for otitis media and released. No history of tick bite was reported. On June 16, the patient developed a diffuse maculopapular rash, and on June 20, the patient was hospitalized because of persistent fever, headache, and vomiting; a viral exanthem or an allergic reaction to the antibiotic was suspected. Laboratory findings included elevated AST (0.96 µkat/L) and ALT (1.52 µkat/L). On June 24, the patient was treated intravenously with a cephalosporin and sent home; however, the patient continued to have fever and headache. On June 30, IFA results from a serum sample obtained June 21 revealed positive IgG and IgM antibody titers (64 and 64, respectively) reactive with R. rickettsii. The patient received oral doxycycline and the symptoms resolved over the next 7 days. On July 6, IFA results of a serum specimen demonstrated an eight-fold increase in the IgG antibody titer to 512, confirming the diagnosis of RMSF. OklahomaOn July 7, a child aged 6 years presented to a physician with a 1-day history of a temperature of 102.2 F (39.0 C), headache, myalgia, diarrhea, and a macular rash on the arms, legs, palms, and soles. On July 1, a tick had been removed from the back of the patient's neck. On July 10, the patient was diagnosed with a viral illness. When the symptoms worsened, the patient was given an oral cephalosporin. On July 11, the patient was hospitalized with dehydration, irritability, confusion, and thrombocytopenia (26 x 109/L). On July 12, the patient was transferred to a tertiary care medical center with disseminated intravascular coagulation. Laboratory results included an elevated WBC count (20 x 109/L) and AST (3.65 µkat/L), and thrombocytopenia (9 x 109/L). On July 13, therapy with intravenous doxycycline for possible RMSF was initiated. The patient subsequently developed gangrene, requiring limb amputation and removal of the upper stomach and distal esophagus. On August 19, the patient died. Using an enzyme immunoassay, a serum sample collected on July 12 tested positive for IgG antibodies reactive with R. rickettsii. Serum obtained on August 3 and tested using an IFA demonstrated a high positive IgG antibody titer of 1024 reactive with R. rickettsii. Reported by: L Minnich, MS, JE McJunkin, MD, Charleston Area Medical Center, Charleston; D Bixler, MD, C Slemp, MD, L Haddy, MA, State Epidemiologist, West Virginia Dept of Health and Human Resources. F Busse, MD, M Harrison, MD, Lakeland Medical Center, Lakeland; MG Stobierski, DVM, ML Boulton, MD, State Epidemiologist, Michigan Dept of Community Health. T Jones, MD, W Moore, MD, State Epidemiologist, Tennessee Dept of Public Health. P Barton, MD, St. Francis Hospital, Tulsa; K Bradley, DVM, M Crutcher, MD, State Epidemiologist, Oklahoma State Dept of Health. State Br, Div of Applied Public Health Training, Epidemiology Program Office; Infectious Disease Pathology Activity, and Viral and Rickettsial Zoonoses Br, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases; and EIS officers, CDC. Editorial Note:Despite its name, RMSF has been reported throughout the continental United States (except in Maine and Vermont) (1,2). During 1990--1998, approximately 4800 RMSF cases were reported to CDC. Approximately 20% of the cases and 15% of reported deaths were in persons aged <10 years. Because of RMSF's rapid course, half the RMSF deaths in this age group occurred within 9 days of illness onset, leaving no more than several days to establish the diagnosis and initiate specific antibiotic therapy. Before the discovery of effective antirickettsial drugs, 13% of children with RMSF died (3). Despite the availability of treatment and advances in supportive medical care, the case-fatality ratio is 2%--3% for patients aged <10 years with RMSF (Figure 1). In its early stages, RMSF may resemble other infectious and noninfectious conditions and can be difficult to diagnose even for physicians familiar with the disease (4,5). Because only 3%--18% of patients present with rash, fever, and a history of tick exposure on their first visit (4--6), physicians should consider RMSF in infants and children even when one feature is lacking. The absence of tick exposure should not dissuade the clinician from suspecting RMSF. Laboratory abnormalities such as thrombocytopenia and hyponatremia should also raise the possibility of RMSF (5). Delayed diagnosis and late initiation of specific antirickettsial therapy (e.g., on or after day 5 of the illness) is associated with substantially greater risk for a fatal outcome (1,4,5). Treatment never should be delayed pending a laboratory diagnosis. Most broad-spectrum antibiotics, including penicillins, cephalosporins, and sulfa-containing antimicrobials, are ineffective treatments for RMSF. In almost all clinical situations, including disease in children aged <8 years, the antibiotic of choice is doxycycline (7). However, this drug is used infrequently as initial therapy even for children who present with signs and symptoms of a rickettsial illness (6). The use of tetracyclines in young children has been discouraged because of the potential for tooth discoloration and should be reserved for patients in whom a rickettsial illness is strongly suspected; however, tetracycline staining of teeth is dose related and available data suggest that one course of doxycycline for presumed RMSF does not cause clinically significant staining of permanent teeth (8). The most effective ways to reduce the risk for RMSF in children are for supervising adults to 1) limit the child's exposure to ticks, especially during April--September; 2) thoroughly inspect the head, body, and clothes for ticks after time spent in wooded or grassy areas, especially along the edges of trails, roads, or yards; and 3) immediately remove attached ticks by grasping the tick with tweezers or forceps close to the skin and pulling gently with steady pressure. More information about RMSF is available on the World-Wide Web, http://www.cdc.gov/ncidod/dvrd/rmsf. References
Figure 1 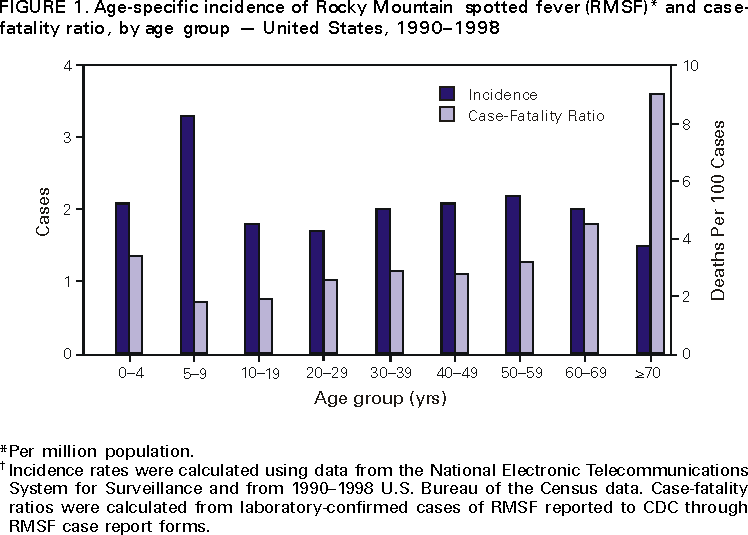 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/5/2000 |
|||||||||
This page last reviewed 5/2/01
|