 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Levels of Diabetes-Related Preventive-Care Practices --- United States, 1997--1999Persons with diabetes are at increased risk for serious complications (e.g., blindness, kidney failure, nontraumatic lower-extremity amputations, and cardiovascular disease) (1). Preventive-care practices, such as annual dilated eye and foot examinations, self-monitoring of blood glucose, and glycemic control, are effective in reducing both the incidence and progression of diabetes-specific complications (2--6). Despite the benefits of preventive-care practices, many persons with diabetes in the United States do not receive these services (7). The national health objectives for 2010 include increasing the proportion of persons with diabetes who 1) have an annual dilated eye examination to 75%, 2) have an annual foot examination to 75%, 3) perform self-monitoring of their blood glucose (SMBG) at least once daily to 60%, and 4) have a glycosylated hemoglobin (HbA1C) measurement at least once a year to 50%. To measure levels of preventive-care practices, CDC analyzed data from the 1997--1999 Behavioral Risk Factor Surveillance System (BRFSS). This report summarizes the results of that analysis, which indicate that levels of preventive-care practices among persons with diabetes are lower than the national health objectives for 2010 (Figure 1). BRFSS is an ongoing, state-based, random-digit--dialed telephone survey of the noninstitutionalized U.S. population aged >18 years. BRFSS is conducted in 50 states, the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands. This analysis was restricted to respondents who answered "yes" to the question, "Has a doctor ever told you that you have diabetes?" Women who were told they had diabetes only during pregnancy were excluded from this analysis. Persons with self-reported diabetes were asked, "When was the last time you had an eye exam in which the pupils were dilated?", "About how many times in the last year has a health professional checked your feet for any sores or irritations?", "About how often do you check your blood for glucose or sugar?", and "About how many times in the last year has a doctor, nurse, or other health professional checked you for glycosylated hemoglobin or hemoglobin `A one C'?" Only persons who reported having seen a health professional for their diabetes during the preceding year were asked if they had their feet examined, and only patients who had seen a health professional for their diabetes during the preceding year and heard of the term "glycosylated hemoglobin" or "hemoglobin A one C" were asked if they had received a HbA1C measurement. Persons who were not asked the questions were considered not to have received the services. Data were analyzed to determine the level of use of each preventive-care practice, by state, in the 40 states that had at least 2 years of data during 1997--1999. In addition, sociodemographic characteristics associated with use of each preventive-care practice were examined. Data were weighted to reflect the age, sex, and racial distribution of the adult, noninstitutionalized population of each state, and all estimates were age-adjusted to the 2000 U.S. adult population. Data were analyzed using SAS software, with SUDAAN to calculate point estimates and 95% confidence intervals. Among adults with diabetes in the 40 states, substantial gaps exist between current levels of preventive-care practices and the 2010 targets (Figure 1). Sociodemographic characteristics associated with each preventive-care practice varied by practice (Table 1). Men were more likely than women to have their feet examined. Persons aged >45 years were more likely to report having a dilated eye examination, persons aged >75 years were less likely to perform SMBG, and persons aged <45 years were more likely to have their HbA1C measured. Non-Hispanic whites were more likely to perform SMBG than were persons from other racial/ethnic groups. Persons with at least a high school education and with health insurance were more likely to receive each of the four preventive-care practices. Levels of preventive-care practices varied by state for each practice (Table 2). The proportion of persons who received an annual dilated eye examination ranged from 47.0 to 81.0, who received an annual foot examination ranged from 42.4 to 69.4, who self-monitored their blood glucose ranged from 29.7 to 65.5, and who received a HbA1C measurement ranged from 16.9 to 42.4. Three states (Alaska, Maine, and Massachu setts) met the dilated eye examination target, and one state (Montana) met the self-monitoring of blood glucose target; no state met the annual foot examination or HbA1C measurement target. Reported by the following BRFSS coordinators: S Reese, MPH, Alabama, MBA; P Owen, Alaska; B Bender, MBA, Arizona; G Potts, MBA, Arkansas; B Davis, PhD, California; M Leff, MSPH, Colorado; M Adams, MPH, Connecticut; F Breukelman, Delaware; I Bullo, District of Columbia; S Hoecherl, Florida; L Martin, MS, Georgia; F Reyes-Salvail, MS, Hawaii; J Aydelotte, MA, Idaho; B Steiner, MS, Illinois; L Stemnock, Indiana; J Igbokwe, PhD, Iowa; C Hunt, MPH, Kansas; T Sparks, Kentucky; B Bates, MSPH, Louisiana; D Maines, Maine; A Weinstein, MA, Maryland; D Brooks, MPH, Massachusetts; H McGee, MPH, Michigan; N Salem, PhD, Minnesota; D Johnson, MS, Mississippi; J Jackson-Thompson, PhD, Missouri; P Feigley, PhD, Montana; L Andelt, PhD, Nebraska; E DeJan, MPH, Nevada; L Powers, MA, New Hampshire; G Boeselager, MS, New Jersey; W Honey, MPH, New Mexico; C Baker, New York; Z Gizlice, PhD, North Carolina; L Shireley, MPH, North Dakota; P Pullen, Ohio; K Baker, MPH, Oklahoma; K Pickle, MS, Oregon; L Mann, Pennsylvania; Y Cintron, MPH, Puerto Rico; J Hesser, PhD, Rhode Island; M Wu, MD, South Carolina; M Gildemaster, South Dakota; D Ridings, Tennessee; K Condon, Texas; K Marti, Utah; C Roe, MS, Vermont; K Carswell, MPH, Virginia; K Wynkoop-Simmons, PhD, Washington; F King, West Virginia; K Pearson, Wisconsin; M Futa, MA, Wyoming. Epidemiology and Statistics Br, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report indicate low levels of preventive-care practices and a wide gap between current state levels and the 2010 targets. States with the lowest levels were approximately 30 percentage points from reaching the target. Increasing the proportion of persons with diabetes who receive each preventive-care practice could minimize diabetes-related complications and would reduce the morbidity, mortality, and costs associated with diabetes (1). Collaborative efforts among health-care systems, health-care providers, public health officials, members of community-based organizations, and patients are needed to identify effective mechanisms for delivering improved quality care to persons with diabetes. The only characteristics that were consistent across each preventive-care practice were education level and health insurance status. These findings suggest that socio-economic status and access to health care have an effect on the receipt of diabetes-related preventive-care practices. Further examination is needed to determine the role of sex, age, and race on receipt of preventive care. The variation by state in receipt of preventive care may, in part, result from differences in demographic distribution, physician practice patterns, health-care system characteristics, and patient attitudes. The findings in this analysis are subject to at least two limitations. First, persons who live in nursing homes and in households without telephones are not included in this survey; therefore, these results cannot be generalized to these segments of the population. Second, because the data were self reported, they are subject to recall bias and may be underreported or overreported. CDC, in collaboration with 59 state and territorial diabetes control programs, provides leadership for a coordinated, multifaceted approach to increasing awareness and education about diabetes, improving the quality of diabetes care, promoting early detection of diabetic complications, and monitoring trends in the quality of care received by persons with diabetes. CDC and the National Institutes of Health will cosponsor the National Diabetes Education Program, which develops educational tools and community-based interventions and establishes public and private partnerships to address the needs of persons with diabetes and raise general awareness about the disease. CDC also supports Diabetes Today, a program that provides health professionals and community leaders with the skills needed to mobilize communities and improve diabetes care. CDC also is working with managed-care partners to determine how to improve care for persons with diabetes. Project TRIAD (Translating Research into Action for Diabetes) is a multicenter study that includes several managed-care organizations. Information on these prevention programs is available on the World-Wide Web at http://www.cdc.gov/diabetes/projects/index.htm. References
Table 1 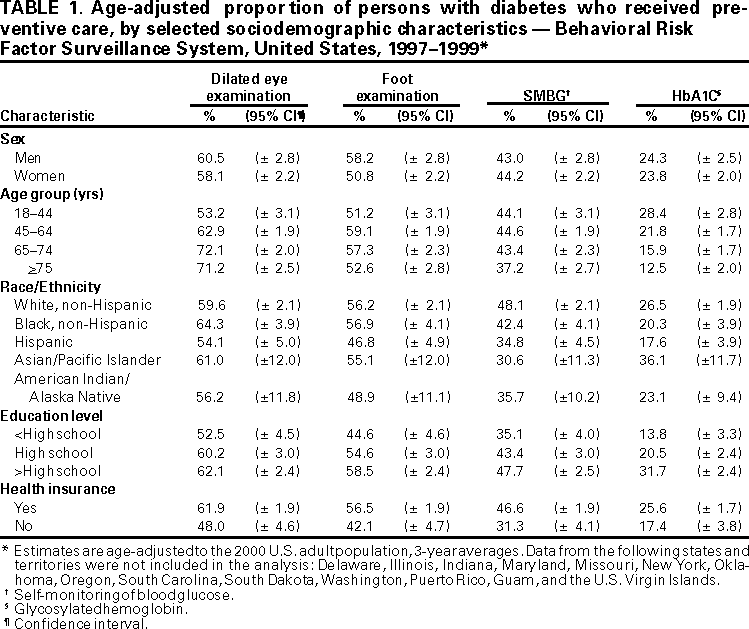 Return to top. Figure 1 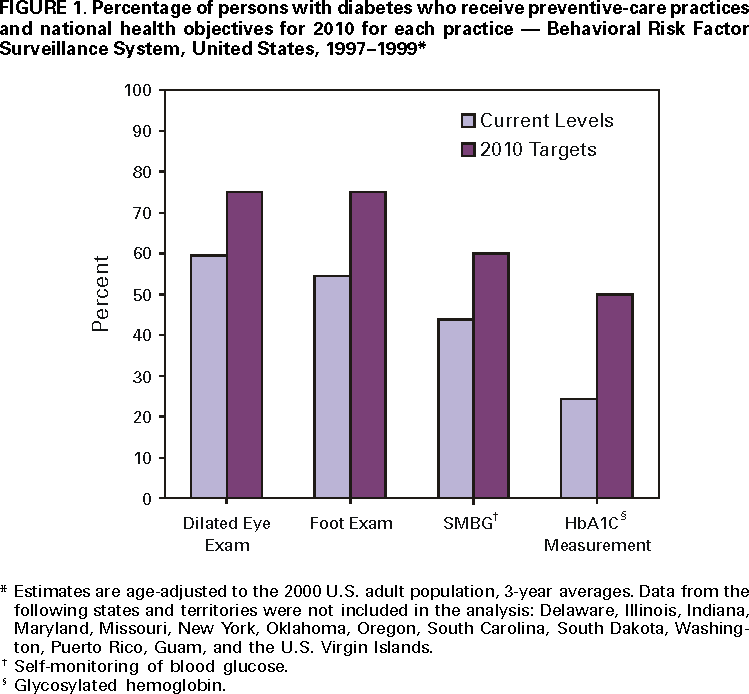 Return to top. Table 2 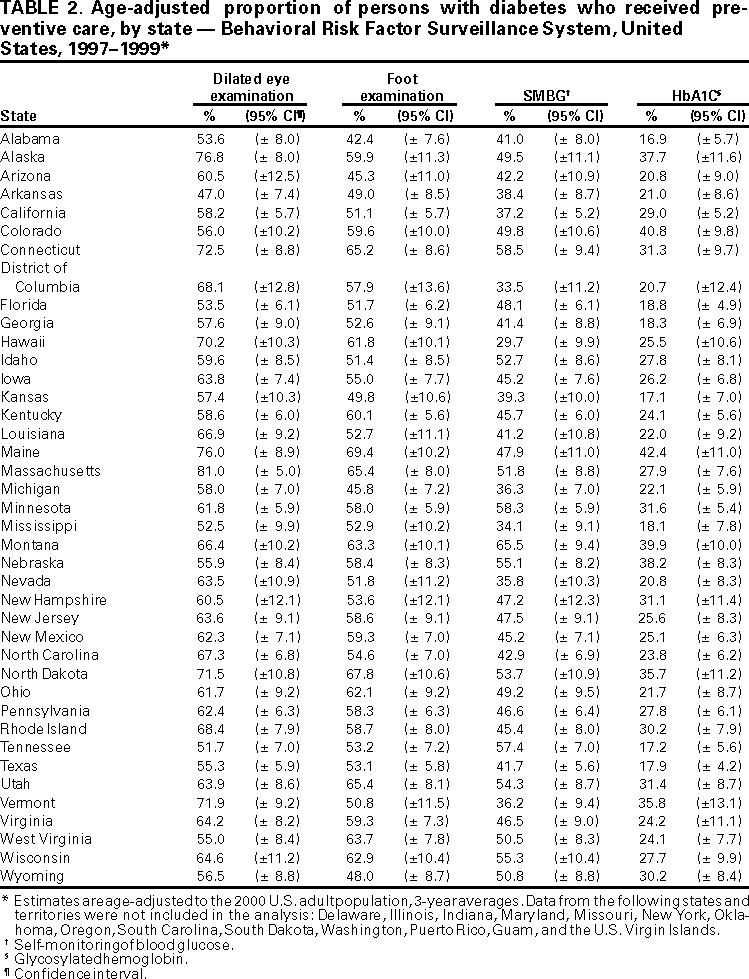 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/26/2000 |
|||||||||
This page last reviewed 5/2/01
|