 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. End-Stage Renal Disease Attributed to Diabetes Among American Indians/Alaska Natives With Diabetes --- United States, 1990--1996Diabetes is the leading cause of end-stage renal disease (ESRD) (i.e., kidney failure requiring dialysis or kidney transplantation), and ESRD treatment has increased among American Indians/Alaska Natives (AI/ANs) (1,2). To assess trends in the incidence of ESRD attributable to diabetes mellitus (ESRD-DM) treatment among AI/ANs with diabetes, CDC and the Indian Health Service (IHS) analyzed data from the U.S. Renal Data System (USRDS). This report summarizes the findings of the analysis, which indicate that the incidence of ESRD-DM treatment is increasing among AI/ANs with diabetes, particularly young AI/ANs. USRDS is a surveillance system for ESRD supported by the Health Care Financing Administration (HCFA), the federal agency that administers the Medicare program which reimburses >90% of the ESRD treatment in the United States (1). USRDS collects, analyzes, and distributes information about the incidence, prevalence, treatment, and costs of ESRD (1), including demographic (e.g., age, sex, and race) and ESRD-related information (e.g., first date of treatment and primary cause of renal failure), ESRD-DM* (i.e., listed in USRDS as the primary cause of renal failure), and first treatment (e.g., kidney dialysis, peritoneal dialysis, or kidney transplantation) in each year during 1990--1996. The incidence of ESRD-DM treatment was calculated using annual age-specific and sex-specific diabetes prevalence estimates from the IHS outpatient database (3) and annual estimates of the AI/AN population from the U.S. Bureau of the Census. Incidence of ESRD-DM treatment was age-adjusted by the direct method based on the 1980 U.S. population with diabetes (4). In 1990, 394 AIs/ANs with diabetes began treatment for ESRD-DM; in 1996, 719 began treatment (Table 1). During 1990--1996, of 3884 AI/ANs with diabetes who began treatment for ESRD-DM, 2221 (57%) were women. During this period, the age-adjusted incidence of ESRD-DM treatment increased 24%, from 472 to 584 per 100,000 persons with diabetes (Table 1). The relative increase in the age-adjusted incidence was 32% among women and 14% among men. In 1996, the age-adjusted incidence of ESRD-DM treatment among AI/ANs with diabetes was 584 per 100,000 persons with diabetes compared with 378 among the entire U.S. population with diabetes (4). Incidence of ESRD-DM treatment among AI/ANs with diabetes increased with age (Figure 1). In 1996, incidence ranged from 278 per 100,000 persons with diabetes among AI/ANs aged <45 years to 723 among those aged >65 years. During 1990--1996, incidence increased 58% among AI/ANs aged <45 years, 9% among those aged 45--64 years, and 34% among those aged >65 years. Reported by: National Diabetes Program Headquarters, Indian Health Svc. Epidemiology and Statistics Br, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:ESRD-DM is a disabling and costly condition that disproportionately affects AI/ANs and is associated with high mortality (1). The data analyzed in this report suggest that the incidence of ESRD-DM treatment among the AI/AN population with diabetes is increasing. The increase in treatment, especially among those aged <45 years, contributes further to the large and growing public health problem of diabetes among AI/ANs (3,5). Reasons for the increased incidence of ESRD-DM treatment need further research; however, possible factors include higher incidence of ESRD-DM, changes in treatment and care practices, greater recognition of the etiologic role of diabetes in ESRD, better access to or acceptance of treatment, or a combination of these factors. Risk factors for developing ESRD-DM include familial and genetic factors, duration of diabetes, hypertension, and hyperglycemia (2). The findings in this report are subject to at least four limitations. First, the data are for persons receiving ESRD treatment as reported to HCFA and do not include patients who die of ESRD before receiving treatment and those who are not reported to HCFA. Second, racial/ethnic misclassification of AI/ANs in USRDS data may result in an under-estimation of incidence (6). Third, underreporting of AI/ANs in U.S. census counts may result in an overestimation of incidence. Finally, IHS data may not account for the total AI/AN population and may result in overestimation or underestimation of the number of AI/ANs with diabetes and, therefore, the incidence of ESRD-DM. Although these biases may have affected the magnitude of incidence estimates, trends in incidence would not be affected if the biases remained constant over time. The increased incidence of ESRD-DM treatment poses a public health challenge for AI/AN communities. Moreover, during 1990--1996, the age-adjusted prevalence of diabetes among AI/ANs increased by 24% compared with 14% among the U.S. general population (3). Interventions are needed to prevent both diabetes and diabetes-related renal disease among AI/ANs. Regular exercise, improved nutrition, and reduced body weight may prevent or delay the onset of diabetes (7). Among persons with diabetes, aggressive blood sugar and hypertension control and the use of angiotensin-converting enzyme inhibitors may prevent or delay the development of ESRD-DM (8--10). In 1998, IHS granted $30 million to tribal governments to help develop and implement interventions to prevent diabetes and its complications. In 1999, CDC, IHS, and other organizations established the National Diabetes Prevention Center in Gallup, New Mexico, to provide guidance and technical support to AI/AN communities throughout the United States and to develop, evaluate, and disseminate culturally appropriate interventions. CDC and the National Institutes of Health cosponsor the National Diabetes Education Program (NDEP) to promote early diagnosis and improve the treatment and outcomes of persons with diabetes. In 1999, in collaboration with IHS and other partners, NDEP launched a diabetes awareness campaign focused on the importance of controlling diabetes. Additional information about NDEP is available from the World-Wide Web, http://ndep.nih.gov/; http://www.cdc.gov/diabetes; or by telephone (800) 438-5383. CDC assists the National IHS Diabetes Program by providing technical assistance on the surveillance of diabetes and its complications among AIs/ANs. The continued surveillance of diabetes and its complications will be an important tool for monitoring the effectiveness of on-going and future prevention strategies. References
* Diabetes as the primary disease causing renal failure is determined by ESRD treatment providers and reported on the Medical Evidence Form of HCFA using a detailed code from a list of diseases. Table 1 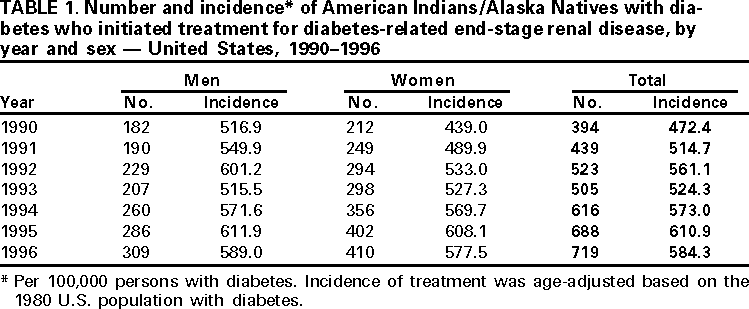 Return to top. Figure 1 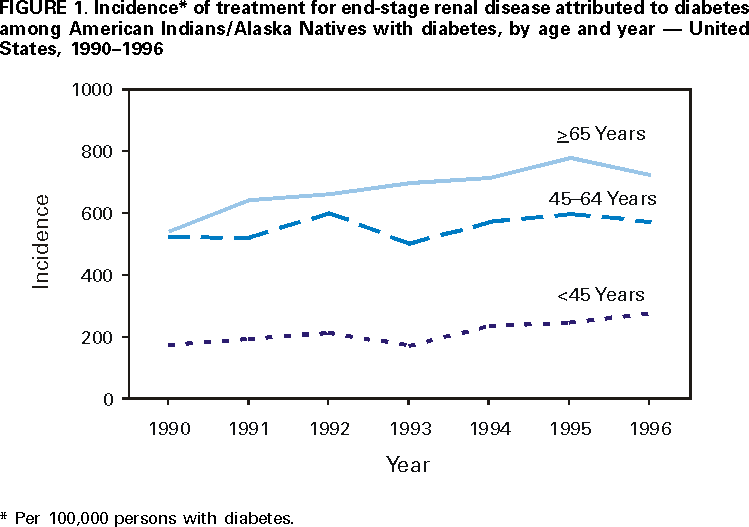 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/26/2000 |
|||||||||
This page last reviewed 5/2/01
|