 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Soft Tissue Infections Among Injection Drug Users --- San Francisco, California, 1996--2000Soft tissue infections (STIs), including abscesses and cellulitis, are a common complication of injection drug use. In 1997, 54 (32%) of 169 injection drug users (IDUs) in one San Francisco neighborhood had a drug-injection--related abscess or cellulitis (1). To characterize STIs among IDUs, data from San Francisco General Hospital (SFGH) discharge and billing records were analyzed. This report summarizes the results of that analysis and presents the case report of one IDU with an STI. The findings indicate that STIs are among the most common diagnoses among patients admitted to SFGH. Preventing STIs among IDUs in San Francisco will require coordinated action involving health-care providers, public health agencies, substance abuse treatment, community outreach, syringe exchange programs, IDUs, and community-based organizations. SFGH inpatient and emergency department (ED) discharge and billing records for fiscal years (FYs) 1996--97 through 1999--2000 were searched for patients aged 15--74 years with primary diagnoses of abscess and/or cellulitis of the trunk, buttocks, or extremities (International Classification of Diseases, Ninth Revision [ICD-9]) codes 682.2--682.7 and 682.9). Records with primary diagnoses of ICD-9 codes corresponding to infections of the fingers, toes, face, neck, or head were excluded because infections in these areas are less likely to be related to drug injection. Data were abstracted about demographics, number of ED discharges and inpatient admissions, average length of inpatient stay, and charges for services. To estimate the proportion of STIs that were related to injection drug use, 30 medical record numbers were selected randomly from the STI discharge lists for the ED and hospital for each FY from 1996--97 through 1999--2000. A total of 240 records were selected for drug-use history review; 20 records were excluded because of multiple visits and/or admissions. Case ReportA 42-year-old woman with a 17-year history of injecting heroin presented to the SFGH ED with a low-grade fever and tenderness and swelling in the left deltoid region. Because her veins were scarred heavily by intravenous injection of heroin, she had been injecting intramuscularly for 10 years. She denied sharing injection equipment but admitted reusing her own syringes without cleaning them. Despite increasing pain and swelling in her left deltoid, she continued to inject into that area for the 2 weeks before admission. She was hospitalized for intravenous antibiotics and incision and drainage of the abscess. Hospital Record ReviewFrom FY 1996--97 through FY 1999--2000, the number of ED discharges for STIs increased 103%, from 1292 to 2619. The number of admissions to SFGH decreased slightly (11%), and the number of hospital admissions and ED discharges increased 41%, from 2787 to 3922 (Figure 1). STIs at different anatomic sites were four of the top 13 inpatient discharge diagnoses at SFGH in FY 1999--2000; STIs at all sites was the leading cause of admission for medical or surgical treatment. Skin incision and drainage was the most common primary procedure on all inpatient records. During FY 1999--2000, 945 persons were admitted with a diagnosis of STI (average hospital stay: 3.2 days); 23% had two or more admissions, resulting in 1326 admissions. In FY 1999--2000, 7% of all SFGH admissions were for STIs. Of the 945 patients, 69% were male; median age was 42 years (range: 15--74 years); 64% were uninsured and 20% were receiving Medicaid. Annual inpatient charges for treatment of STIs averaged $9.9 million per FY from 1996 to 2000. Because most patients admitted to SFGH were uninsured, San Francisco County was responsible for inpatient charges of approximately $5.1 million. Of the 220 records selected for review, 188 were located. Of these, 132 (70%) documented injection drug use during the preceding 12 months (86% involved heroin). Two (1%) had histories of injection drug use more than 1 year before the onset of STI. Fifty-four (29%) had no history of drug injection; of these, 34 (18%) had a cause for the STI noted in the record, and 20 (11%) had no documented cause. In July 1999, concern over the high rate of STIs among IDUs led to the formation of a multiagency STI task force that included representatives of SFGH administration, researchers, community clinicians, and the San Francisco Department of Public Health. The task force recommended the creation of a hospital-based STI clinic, community outreach to IDUs, expansion of substance treatment services, and standardization of community medical and surgical STI treatment with an emphasis on expanding community-based treatment and prevention. Reported by: D Ciccarone, MD, Dept of Family and Community Medicine, Univ of California, San Francisco; JD Bamberger, MD, San Francisco Dept of Public Health, San Francisco; AH Kral, PhD, BR Edlin, MD, Urban Health Study, Univ of California, San Francisco; CJ Hobart, Univ of California, San Francisco; A Moon, San Francisco General Hospital, San Francisco; EL Murphy, MD, Dept of Laboratory Medicine, Univ of California, San Francisco; P Bourgois, PhD, Dept of Medical Anthropology, History and Social Medicine, Univ of California, San Francisco; HW Harris, MD, DM Young, MD, Dept of Surgery, Univ of California, San Francisco. Editorial Note:The findings in this report indicate that many STIs in San Francisco are related to injection drug use and are a major cause of hospitalization. Some STIs among IDUs are complicated by tetanus (2), botulism (3), and myonecrosis (D. Bangsberg, Epidemiology and Prevention Interventions Center, SFGH, personal communication, 2000). Possible contributing factors to the high rate of STIs among San Francisco IDUs include poor injection site hygiene, syringe reuse, intramuscular or subcutaneous routes of injection, and contaminated drugs. IDUs often contaminate needles by touching them to surfaces, mouths, or hands (4). Reuse of syringes may increase the chance of bacterial infections (5). San Francisco IDUs with STIs report frequent reuse of syringes that only they have used (4). State laws requiring a prescription to purchase syringes and making possession of syringes by IDUs a crime may contribute to the reuse of syringes (6). Subcutaneous and intramuscular injection of heroin (either intentional or inadvertent) is associated with STI (1). Use of alcohol to clean the skin before injection may protect against STI (7). In San Francisco, the local health department pays most of the costs of caring for persons with STIs. In 1997, Federal Social Security Insurance (SSI) disability eligibility was amended so that drug and alcohol addictions were no longer qualifying disabilities (8). Because California's Medicaid program is linked to SSI, the restriction of federal disability eligibility has reduced the ability of local municipalities to obtain state and federal financial support for the medical costs of persons living with substance addiction. In response to the high use of emergency and inpatient services, SFGH opened a surgical outpatient STI clinic in July 2000. As of February 2001, the clinic averaged 273 patient visits and 170 procedures per month. For FY 2000--2001, the numbers of admissions and ED visits for treatment of STIs are projected to decline significantly compared with FY 1999--2000. The findings in this report are subject to at least four limitations. First, the hospital and ED discharge records may be incomplete or inaccurate. Second, using only primary diagnoses underestimated the number of STIs. Third, because only a small percentage of medical records were reviewed, the proportion of STIs attributed to injection drug use is uncertain. Finally, hospital charges were estimated and are related but not equal to the cost to the hospital. Primary prevention strategies to reduce STIs among IDUs include preventing initiation of injection drug use and increasing entry and retention of IDUs in substance abuse treatment (particularly methadone maintenance). For IDUs who continue to inject drugs, increasing access to sterile injection equipment and alcohol swabs and promoting hygiene (including hand washing, cleaning the injection site before injection, using a sterile syringe for every injection, and avoiding needle contamination) are important prevention goals. Secondary prevention strategies include promoting earlier medical and surgical treatment of STIs. Microbiologic testing of street samples of black tar heroin also may help identify the causes of injection-related STI. Ongoing research into the behavioral and biologic risk factors for STI may identify additional prevention interventions (9). References
Figure 1 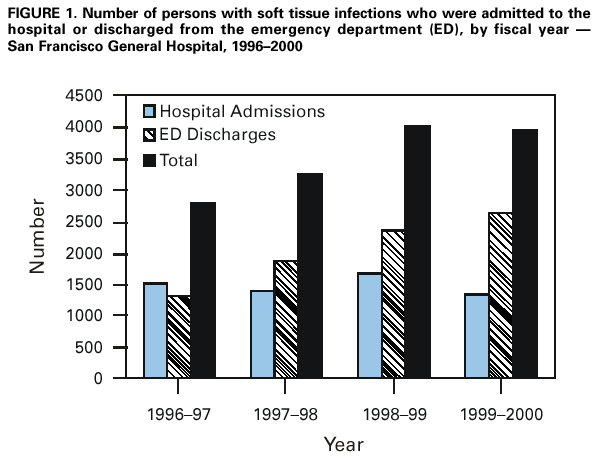 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 5/17/2001 |
|||||||||
This page last reviewed 5/17/2001
|