 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. The Global HIV and AIDS Epidemic, 2001Human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS) are pandemic and pose one of the greatest challenges to global public health. As a bloodborne and sexually transmitted infection, HIV has variable patterns of transmission and impact among world regions and has disproportionately affected disadvantaged or marginalized persons such as commercial sex workers, injection drug users, men who have sex with men (MSM), and persons living in poverty. HIV infection has caused approximately 20 million deaths; an estimated 36 million persons are infected (Figure 1). On the basis of data from the Joint United Nations Program on AIDS (UNAIDS) and other sources, this report summarizes epidemiologic trends, highlights several HIV and AIDS prevention milestones, and describes some prevention activities for the coming decade (1--4). Sub-Saharan Africa (SSA)SSA* is the region of the world most severely affected by HIV and AIDS. Uganda, Kenya, and Tanzania were among the countries where the HIV epidemic was first recognized during the early 1980s. In 2000, an estimated 25.3 million persons in SSA were infected with HIV, and the average national prevalence of HIV infection among persons aged 15--49 years was 8.8%. Approximately four million new infections occurred during 2000. Approximately 10% of persons aged 15--49 years are infected in 16 countries, including seven in southern and eastern Africa, where approximately 20% are infected. In Botswana, the country with the highest prevalence, 36% of the adult population is infected with HIV (Figure 2). Despite these trends, intensive and aggressive prevention programs for behavior change, condom promotion, voluntary HIV counseling and testing, and blood transfusion safety have lowered prevalence or slowed HIV transmission in several SSA countries. For example, in Uganda during 1990--2000, overall adult HIV prevalence declined from 14% to 8%. In Masaka, Uganda, HIV prevalence among females aged 20--24 years decreased from 20.9% during 1989--1990 to 13.8% during 1996--1997 (5). Also, in Lusaka, Zambia, which had an early and severe epidemic, HIV prevalence declined among females aged 15--19 years attending prenatal clinics from 27% in 1993 to 17% in 1998. In West Africa, Senegal has maintained a prevalence of approximately 2%; prevention efforts have included regulating commercial sex, intensive condom promotion, treatment of sexually transmitted diseases (STDs), and community mobilization. AsiaThe epidemic continues to spread in the world's most populous areas, where the infrastructure for an effective response is underdeveloped. In China, HIV prevalence was as high as 82% among injection drug users and 6% in commercial sex workers during 1998--1999. A sustained increase also occurred in all reported STDs among males and females during 1989--1998. In India, the estimated HIV infection rate among persons aged 15--49 years is 0.7%. As of mid-1998, an estimated 3.5 million persons were infected with HIV. An exception to countries with increasing prevalence is Thailand, where the epidemic began in the mid-1980s among injection drug users and commercial sex workers and their clients and spread rapidly to the wider population through heterosexual transmission. In response, health officials developed HIV and AIDS surveillance systems and mounted a sustained and effective response, including the "100% condom use" campaign for commercial sex. The resulting decline in STD and HIV transmission was reflected in a decrease in STD rates and HIV prevalence in military recruits and women attending prenatal clinics. Eastern Europe and Central AsiaEastern Europe has had recent and rapid growth of HIV infection among injection drug users. By January 1999, approximately 10,000 HIV cases had been reported in the Russian Federation. By December 2000, the cumulative total increased to 70,000, and HIV infection among injection drug users was reported from 82 of the 89 regions in the Russian Federation. Ukraine was the country most affected in Eastern Europe and Central Asia, where newly reported infections increased from 47 cases per year during 1992--1994 to approximately 15,000 cases in 1997. Ukraine accounted for 90% of all AIDS cases reported in the region in 1998 and 1999. HIV probably will spread further in the region as a result of the large number of injection drug users, increasing rates of STDs, the growing commercial sex industry, and socioeconomic transitions. United States and Western EuropeIn Western Europe and the United States, deaths attributed to HIV have declined substantially since the introduction of highly active antiretroviral therapies. However, reported increases in STDs among MSM and other indicators of increased risk-taking behavior may be leading to an increase in HIV transmission. Latin America and the CaribbeanIn Latin America and the Caribbean, the leading modes of transmission include sex between men, sex between men and women, and injection drug use. By December 2000, an estimated 1.4 million adults and children were infected with HIV/AIDS in the region compared with 1.3 million in 1999. Barbados, Belize, Dominican Republic, Guyana, Haiti, and Suriname have an HIV prevalence of approximately 1%. The Caribbean, with an adult prevalence of 2.1%, is the second most affected world region. In Brazil, reported HIV-related deaths have declined from approximately 25 per 100,000 in 1995 to approximately 15 per 100,000 in 1999, in large part because of the government policy of providing universal, free access to antiretroviral therapies (6). Reported by: Global AIDS Program, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:HIV and AIDS is the leading cause of death in Africa and the fourth leading cause of death worldwide. In the countries most affected in Africa, life expectancy has declined by 10 years and infant death rates have doubled. In countries with the highest prevalence, such as Botswana, South Africa, and Zimbabwe, the full impact of the epidemic has not been felt because those infected recently have not developed symptoms. Equally important is the effect of HIV deaths on families, social systems, and national growth and development. Young adults who contribute substantially to countries' gross domestic product are most commonly affected. In families, loss of one or both parents to HIV can lead to loss of income, cessation of children's education, increased child labor, and disruption of family and social support systems. For example, in Zambia, a shortage of school teachers has occurred because more teachers are dying of AIDS than can be trained to replace them. Considerable heterogeneity of rates exist in HIV-infected countries throughout the world, and the differences have been attributed to risk factors associated with the spread of HIV and AIDS. They include migration, economic instability, drug use, STDs, low levels of literacy, and poverty. These are formidable challenges to implementing effective prevention programs (4). Although the earliest epidemiologic studies described the modes of transmission of HIV and AIDS and provided insights into the types of interventions needed to prevent transmission, this understanding has been difficult to translate into effective interventions worldwide. The HIV epidemic has challenged public health agencies to develop new and often controversial prevention programs that contradict established practices and social norms. Despite these challenges, even countries with modest resources have demonstrated that the epidemic can be stabilized or reversed. In these countries, successful programs have included strong, high-level political leadership for HIV prevention, a national program plan, adequate funding, and strong community involvement. Effective and feasible interventions for HIV prevention and control are available. Quality testing and guidelines for blood use can promote a safer blood supply. Widespread condom promotion can reduce HIV seroprevalance in high-risk populations, and education programs for young persons can result in decreased risk-taking behavior. Increasing access to drug treatment and providing education about and increasing access to clean syringes can reduce infection risk in drug using populations. Prophylaxis with co-trimoxazole can prevent certain opportunistic infections and reduce the number of HIV-related deaths. Administering antiviral agents, such as niverapine or short-course zidovudine, and advice to women on breastfeeding, can substantially reduce mother-to-infant transmission (7). Improving treatment for STDs can slow HIV infection rates (8). When effective STD treatment programs continue to be compromised by weak infrastructure, important opportunities for HIV prevention are lost. Efforts are needed to strengthen STD services and to integrate these with HIV prevention and control programs. The social stigma associated with HIV infection in many cultures combined with difficulties in providing treatment or services for infected persons are major barriers to expanding voluntary counseling and testing for HIV. Persons who may benefit from knowing their serostatus often reject counseling and testing because they fear the consequences of disclosure of their HIV status. Other disincentives are the lack of resources for care and treatment and the sense that little is gained from learning that one is infected with HIV. Prevention programs must be accompanied by efforts to improve the care of HIV-infected persons. Isoniazid prophylaxis for TB (9) and other low-cost interventions should be incorporated into prevention programs (10). The most effective intervention therapy for persons infected with HIV is the use of a combination of antiretroviral agents. However, the high cost of these regimens and the infrastructure needed to monitor their use have put these medications beyond the reach of most HIV-infected persons. Although the price of these drugs has fallen, making treatment a possibility for a greater number of persons, infrastructures to support the effective use of these medications remain inadequate and need strengthening. Given the needs for both prevention and treatment, public health officials and international donors will need to determine the best mix of drug treatment and prevention programs. Globally, the HIV epidemic has intersected with other, underlying public health problems, most notably tuberculosis (TB). TB remains the principal cause of death in persons with HIV infection worldwide. National TB rates have escalated over the past decade in SSA and South-East Asia. Since the mid-1980s, in many African countries with well-organized programs, annual TB notification rates have increased fourfold, reaching peaks of more than 400 cases per 100,000 population. In some countries, up to 70% of patients with sputum smear-positive pulmonary TB are HIV-infected. To the extent possible, integration of HIV and TB prevention programs should be a priority in these countries. The increase in HIV infection and AIDS deaths has led to increases in aid from governments and national and international organizations and foundations. Since 1999, the U.S. government increased its financial support to HIV/AIDS prevention and care programs in affected countries. For fiscal year 2001, this totaled $457.5 million. Participating agencies include the U.S. Agency for International Development, the U.S. Department of Health and Human Services (including CDC, and the Health Resources and Services Administration), the Department of Defense, the Department of Labor, and the Department of Commerce. The National Institutes of Health recently launched the Comprehensive International Program for Research on AIDS (CIPRA) to assist developing countries with research agendas relevant to their populations and to enhance infrastructure. CDC established the Global AIDS Program (GAP) to implement international HIV prevention efforts in collaboration with other federal agencies. The program emphasizes sustaining intervention programs for primary prevention of HIV infection, infrastructure development and laboratory support, and home- and community-based care for persons with HIV infection. CDC is supporting these activities in 24 countries in partnership with other U.S. agencies, national ministries of health, UNAIDS, and other international agencies. References
*Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Cape Verde, Central African Republic, Chad, Congo, Cotê d'Ivoire, Democratic Republic of Congo, Djibouti, Eritrea, Ethiopia, Equatorial Guinea, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Malawi, Mali, Mauritania, Mozambique, Namibia, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, South Africa, Swaziland, Tanzania, Togo, Sao Tome-Principe, Uganda, Zambia, and Zimbabwe. Figure 1 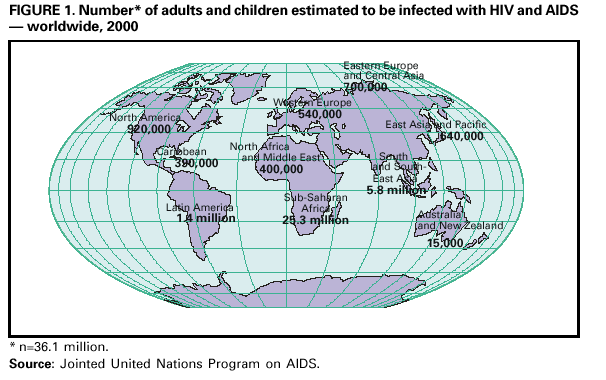 Return to top. Figure 2 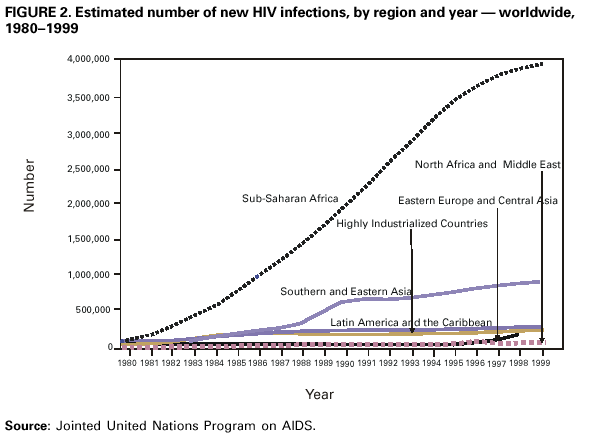 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 6/8/2001 |
|||||||||
This page last reviewed 6/8/2001
|