 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Hospital Discharge Rates for Nontraumatic Lower Extremity Amputation by Diabetes Status --- United States, 1997Lower extremity amputation (LEA) is a costly and disabling procedure that disproportionately affects persons with diabetes (1,2). One of the national health objectives for 2000 was to reduce the LEA rate from a 1991 baseline of approximately eight per 1,000 persons with diabetes to a target of approximately five per 1,000 persons with diabetes. Review of 1996 data indicated an LEA rate of approximately 11. To estimate the national rates of hospital discharges for LEA among persons with and without diabetes and to assess the excess risk for LEA among persons with diabetes, CDC and the Agency for Healthcare Research and Quality (AHRQ) analyzed data from the 1997 Nationwide Inpatient Sample (NIS) and the 1997 National Health Interview Survey (NHIS). This report summarizes the findings of the analysis, which indicated that the age-adjusted rates of hospital discharges among persons with LEA who had diabetes were 28 times that of those without diabetes. This higher rate underscores the need to increase efforts to prevent risk factors (e.g., peripheral vascular disease, neuropathy, and infection) that result in LEA among persons with diabetes. Hospital discharges were estimated from NIS, a stratified probability sample of hospitals in 22 states. Discharges from these states represented approximately 60% of all discharges in the United States. Sample data were weighted using the American Hospital Association Annual Survey of Hospitals to approximate discharges from all U.S. acute-care community hospitals. LEA discharges were defined using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes 84.10--84.19 (traumatic LEA codes 895--897 were excluded). Diabetes-related LEA discharges were identified as discharges that included ICD-9-CM code 250 as one of the listed discharge diagnoses. LEA hospital discharge rates were calculated for populations with and without diabetes. Estimates of the number of persons with and without diabetes were obtained from the 1997 NHIS, an ongoing, nationally representative survey providing information about the health of the noninstitutionalized U.S. civilian population (3). SUDAAN was used to calculate estimates and 95% confidence intervals (CIs) of NIS and NHIS data. The 2000 U.S. standard population was used to adjust LEA rates by age. The rate ratio was calculated by dividing the LEA rate for persons with diabetes by the rate for persons without diabetes. The rate difference was defined as the difference in LEA rates between the two populations. The significance of trends by age was assessed for LEA rates, rate ratios, and rate differences, and t-tests in SUDAAN were used to determine the significance of the difference in mean age by diabetes status and the age-adjusted rate differences by sex and race. Z-tests were used to assess the difference between age-adjusted rates by diabetes status among all sex and race groups. In 1997, 131,218 hospital discharges had an LEA discharge diagnosis code; 87,720 (67%) of these were related to diabetes (Table 1). Among persons with diabetes, 66.7% of LEA hospitalizations were paid by Medicare and an additional 8.1% were paid by Medicaid. Among persons with diabetes, approximately 52% of amputations occurred at or below the foot, and among persons without diabetes, approximately 70% occurred between the ankle and the knee or higher. Patients with diabetes-related LEA hospital discharges had a mean age of 66 years (95% CI=+0.3 years), and the mean age of LEA discharges not related to diabetes was 71 years (95% CI=+0.7 years) (p<0.0001). LEA rates increased with age in both populations, but rates were higher in the population with diabetes. LEA rate ratios ranged from 149 (95% CI=116--182) to nine (95% CI=7--10) for persons aged <44 years and >75 years, respectively. Rate differences ranged from 3.4 to 13.8 per 1,000 persons in those aged <44 years to >75 years, respectively. The age-adjusted LEA rate for persons with diabetes (5.5 per 1,000 persons with diabetes) was 28 (95% CI=24--31) times that of persons without diabetes (0.2 per 1,000 persons without diabetes). Regardless of diabetes status, these rates were higher for men than women (p<0.0001) and higher for non-Hispanic blacks than Hispanics or non-Hispanic whites (p<0.05) (Figure 1). Age-adjusted LEA rates were much higher for persons with diabetes for both sexes and all racial/ethnic populations (p<0.0001). Reported by: Center for Organization and Delivery Studies, Agency for Healthcare Research and Quality, Rockville, Maryland. Epidemiology and Statistics Br, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report indicate that LEAs occur at a much higher rate among persons with diabetes and that diabetes causes approximately 67% of LEAs. Among persons with diabetes, LEA rates were highest among men, non-Hispanic blacks, and the elderly. These findings indicate that LEAs might increase as the U.S. population ages and as the prevalence of diabetes increases. Because approximately 75% of LEA hospitalizations are paid by Medicare or Medicaid, the increase in prevalence will place a large financial burden on these public health systems. Among persons with diabetes, LEAs result from the single or combined effects of peripheral vascular disease, peripheral neuropathy, and infection (1,4). Foot deformities and ulcers occurring as a consequence of neuropathy and/or peripheral vascular disease, minor trauma, and poor foot care also might contribute to LEAs (1,5). The findings in this study are subject to at least five limitations. First, because NIS data represent hospital discharges and not individual persons, patients with multiple amputations within 1 year were counted multiple times; this might have resulted in an over-estimation of hospital discharge rates. Second, because NIS data do not include LEAs that occurred in federal hospitals and outpatient settings, the analysis underestimates the total number of LEA discharges that occurred nationally. Third, because NHIS is representative of the noninstitutionalized civilian population, the total population with or without diabetes was underestimated. Fourth, race/ethnicity data are missing for approximately 20% of the hospital discharges in NIS data; four states contributing to NIS provided no race/ethnicity data and one state provided race/ethnicity information for approximately 25% of discharges. Therefore, race/ethnicity-specific rates are underreported and may be biased if race/ethnicity disease patterns vary across reporting and nonreporting states. Finally, because the NIS sample was constructed from only 22 states, these data might be biased and might differ from estimates of the National Hospital Discharge Sample (NHDS). However, in 1997, both data sources produced similar estimates of discharges with diabetes as the primary diagnosis (AHRQ, unpublished data, 2000). Serious foot conditions or LEA can be decreased by 44%--85% in persons with diabetes (5). Proper footware can lower abnormal pressure and protect the foot from calluses and ulcers, precursors of LEA (6). Education intervention, multidisciplinary care, and insurance coverage for therapeutic shoes are effective in reducing diabetes-related LEA (2). Interventions also include early detection of feet at risk through regular foot examination, knowledge of foot hygiene, nonweight-bearing exercise, and provider education on screening examinations for high-risk foot conditions (6,7). Good glycemic control can reduce the development of neuropathy, a high-risk condition for LEA (8,9). Because no nationally representative data on lower extremity disease and its risk factors exist, in 1999, CDC and the National Heart, Lung, and Blood Institute of the National Institutes of Health added to the National Health and Nutrition Examination Survey a lower extremity disease examination component for peripheral vascular disease, peripheral neuropathy, and foot deformities, ulcers, and amputations. This component will allow national estimates of the extent of lower extremity disease and identification of its risk factors. It also will increase an understanding of racial/ethnic differences in lower extremity disease and provide information to clinicians and public health providers to develop preventive care and community-based interventions. Materials designed to make good foot care an essential part of diabetes care among health-care providers and persons with diabetes are available at <http://ndep.nih.gov/materials/pubs/feet/feet.htm>. References
Table 1 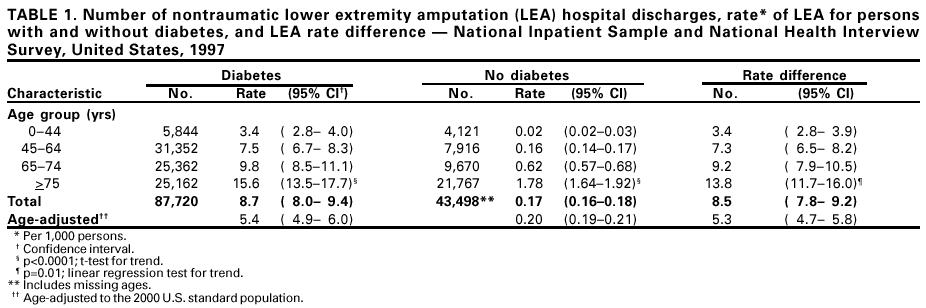 Return to top. Figure 1 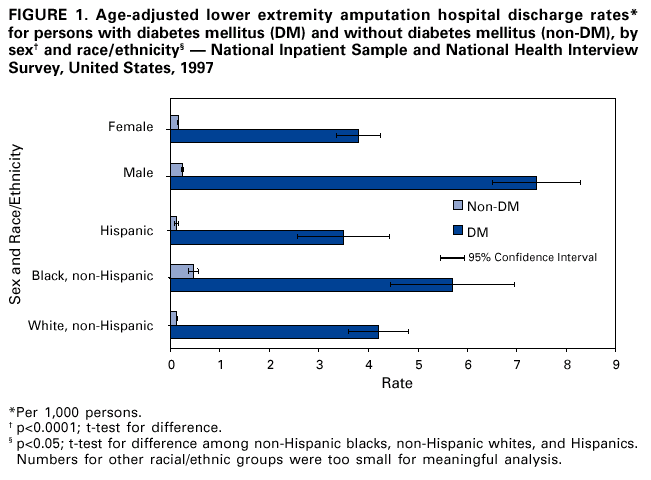 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 11/2/2001 |
|||||||||
This page last reviewed 11/2/2001
|