 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. State Medicaid Coverage for Tobacco-Dependence Treatments --- United States, 1998 and 2000The Guide to Community Preventive Services (1) recommends reducing the cost of tobacco-dependence treatments because these interventions increase both the use of treatment by smokers during attempts to stop smoking and the number of smokers who actually stop. The Public Health Service (PHS) Clinical Practice Guideline (2) supports insurance coverage for tobacco-dependence treatment (i.e., individual, group, and telephone counseling, and Food and Drug Administration-approved pharmacotherapy) (2). One of the 2010 national health objectives (3) is to provide coverage in the 50 states and District of Columbia (DC) for nicotine-dependence treatment by Medicaid (objective 27.8b) (3). In 2000, approximately 32 million low-income persons in the United States received their health insurance coverage through the federal-state Medicaid program (4); approximately 11.5 million (36%) of these persons smoked (CDC, unpublished data, 2000). Medicaid recipients have approximately 50% greater smoking prevalence than the overall U.S. population. To assess the amount and type of coverage for tobacco dependence offered by Medicaid, the Center for Health and Public Policy Studies at the University of California, Berkeley, conducted state surveys in 1998 and 2000. In 1998, 24 states and DC offered some coverage for tobacco-dependence treatment; in 2000, nine started offering some coverage. In 1998 and 2000, one state offered coverage for all the counseling and pharmacotherapy treatments recommended by PHS. These findings indicate that states can reduce smoking prevalence among Medicaid recipients by implementing more extensive Medicaid coverage for treatment of tobacco dependence. To obtain and update information on Medicaid coverage of specific tobacco- dependence treatments, a survey was faxed to the 50 states and DC Medicaid programs during 1998 and 2000. State Medicaid program directors were asked to identify staff members most knowledgeable about tobacco-dependence treatment coverage and programs. A 10-page survey was faxed to the identified staff member in each state. Additional followup was conducted; the final response rate in both 1998 and 2000 was 100%. The survey included 26 questions about coverage of tobacco-dependence treatments, awareness of clinical practice guidelines for treatment of tobacco dependence, and state activities to document and support providers and health plans in delivering tobacco-dependence treatment services to Medicaid recipients. The only difference in the two surveys was that on the 2000 survey form, a question was asked about bupropion, the generic name for Wellbutrin® and Zyban® (GlaxoSmithKline, Research Triangle Park, North Carolina). To validate state Medicaid program responses to survey questions, all reporting areas were asked to submit a written copy of their coverage policies for tobacco-dependence treatment. Of the 34 Medicaid programs that reported offering coverage in 2000, 39 states and DC (91%) provided supporting documentation; 11 noted that pharmacotherapy was covered under standard drug benefits; three states (9%) did not provide a coverage policy statement. In 2000, a total of 33 states and DC offered some coverage for tobacco-dependence treatments; one state offered coverage for all treatments recommended by PHS. In 2000, some pharmacotherapy coverage was offered by 31 states, an increase of 35% from 1998. Sixteen states offered coverage for all recommended pharmacotherapy treatments in 2000. In 1998, a total of 23 states offered some coverage for prescription drugs and 17 for over-the-counter drugs; in 2000, a total of 31 states offered coverage for prescription drugs and 23 for over-the-counter drugs. In 2000, a total of 13 states offered special tobacco-dependence treatment programs for pregnant women; in two states, counseling services were covered for pregnant women only. In 2000, two states covered some form of counseling services without coverage for any drug treatments. During 1998--2000, one state dropped Medicaid coverage for bupropion and one state stopped Medicaid coverage for counseling. In 2000, a total of 11 states covered at least one type of pharmacotherapy and one type of counseling. In 2000, a total of 17 state Medicaid programs reported no coverage for tobacco-dependence treatments (Table 1). Reported by: HH Schauffler, PhD, J Mordavsky, MPH, Univ of California-Berkeley School of Public Health, Berkeley; D Barker, MHS, Barker Bi-Coastal Health, Calabasas, California. CT Orleans, PhD, Robert Wood Johnson Foundation, Princeton, New Jersey. Epidemiology Br, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:Coverage of tobacco-use treatment under Medicaid remains low despite available and effective treatments for tobacco dependence (2) and evidence that decreasing the cost of treatment increases successful cessation (1). Two major barriers to using treatment for low-income smokers are the lack of access to and cost of effective treatment (5). In 2000, a total of 17 states offered no coverage for tobacco-use treatment and only Oregon provided coverage for all cessation interventions recommended by PHS. Strategies to increase access include incorporating tobacco-use treatment into routine health-care visits, and offering coverage of treatment costs and access to telephone quit lines (1). Tobacco-use treatment is one of the most cost-effective prevention services (2,6,7). Based on disease impact, intervention effectiveness, and cost effectiveness, a recent study ranked tobacco-use treatment second (after childhood vaccination) among 30 prevention services recommended by the Guide to Clinical Preventive Services. Because the current provision of service is low, tobacco-use treatment was also the service that had the potential for the greatest improvement (8). The findings in this report are subject to at least one limitation. The data were self-reported. Among the 34 Medicaid programs reporting coverage in 2000, three could not document coverage. The absence of written policy increases the likelihood of reporting errors. These results might differ from other ratings of coverage as the result of interpretations of unwritten policies. Tobacco use is the leading preventable cause of death in the United States (9). Because smoking prevalence is high among Medicaid recipients, they are affected disproportionately by tobacco and tobacco-related disease and disability. CDC supports efforts to assist state Medicaid programs in meeting the PHS and Community Preventive Services Task Force recommendations and the national health objective for tobacco-dependence treatment coverage. Substantial action to improve coverage will be needed if the United States is to reach the 2010 national health objective to reduce from 24% in 1998 to 12% the prevalence of current cigarette smoking among persons aged >18 years. States are encouraged to cover all recommended pharmacotherapy and counseling for Medicaid populations. References
Table 1 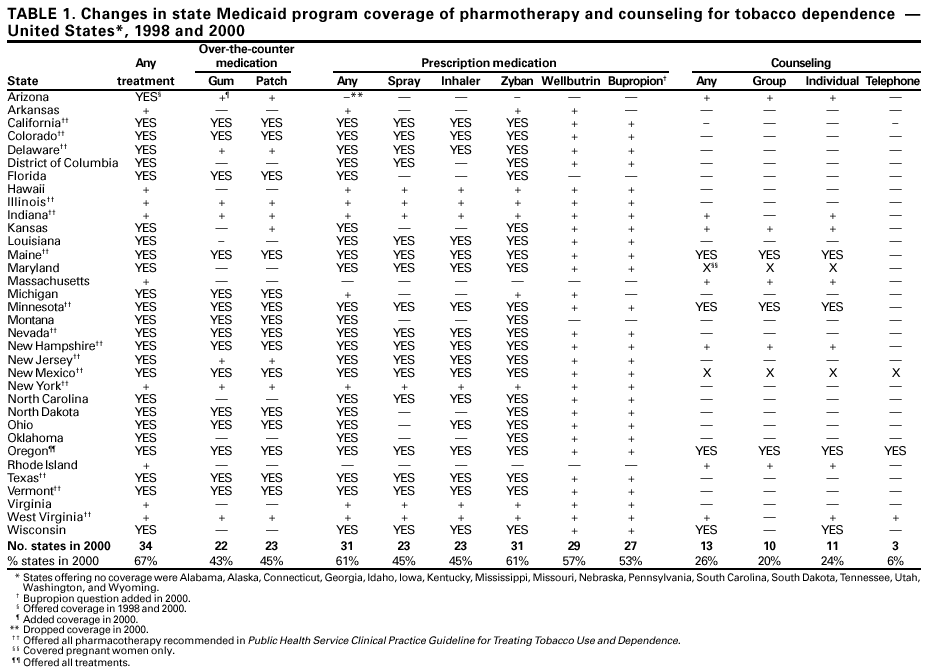 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 11/13/2001 |
|||||||||
This page last reviewed 11/13/2001
|