 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Imported Plague --- New York City, 2002On November 1, 2002, a married couple traveled from Santa Fe County, New Mexico, to New York City (NYC), where they both became ill with fever and unilateral inguinal adenopathy; bubonic plague (Yersinia pestis) was diagnosed subsequently. This report summarizes the clinical and public health investigation of these cases and underscores the importance of rapid diagnosis and communication among health-care providers, public health agencies, and the public when patients seek medical attention for an illness that might be caused by an agent of terrorism. Case ReportsCase 1. On November 5, a man aged 53 years sought medical care in a NYC emergency department (ED) after consulting with his physician in New Mexico and the physician at the hotel in which he was staying. He reported 2 days of fever, fatigue, and painful unilateral inguinal swelling. On clinical examination, he appeared ill with diaphoresis, rigors, and lower extremity cyanosis. His temperature was 104.4º F (40.2º C), blood pressure was 78/50 mm Hg, and oxygen saturation was 98% on room air. He had tender left inguinal adenopathy with overlying edema. White blood cell (WBC) count was 24,700/µL (normal: 4,300--10,800/µL), and platelet count was 72,000/µL (normal: 130,000--400,000/µL). A blood culture grew Y. pestis. Gram stain of the blood culture isolate revealed bipolar gram-negative rods with a "safety pin" appearance. On November 6, direct fluorescent antibody (DFA) to Y. pestis F1 antigen and polymerase chain reaction (PCR) performed on the initial blood culture conducted by the NYC Public Health Laboratory (NYCPHL) both were positive. The patient received gentamicin, doxycycline, ciprofloxacin, vancomycin, and activated protein C. The patient's condition deteriorated, and he was admitted to the intensive care unit (ICU) in shock with a diagnosis of septicemic plague, acute renal failure, acute respiratory distress syndrome, and disseminated intravascular coagulation. He required hemodialysis and mechanical ventilation and underwent bilateral foot amputations subsequently because of ischemia. After a 6-week ICU stay, he recovered and was discharged to a long-term--care rehabilitation facility. Case 2. On November 3, the wife, aged 47 years, of patient 1 also became ill. On November 5, she sought medical care for fever, fatigue, myalgias, and unilateral inguinal swelling. A physical examination noted tender right inguinal and femoral adenopathy with overlying erythema and induration. Her temperature was 102.2º F (39.0º C), blood pressure was 120/72 mm Hg, and oxygen saturation was 98% on room air. WBC was 9,500/µL, and platelet count was 189,000/µL. Aspiration of the inguinal lymph nodes did not yield any material. The patient received a presumptive diagnosis of bubonic plague because of her clinical signs and symptoms and the recovery of Y. pestis from her husband's blood culture. She was hospitalized and treated with gentamicin, doxycycline, and ticarcillin-clavulanic acid, followed by a 14-day course of oral doxycycline 100 mg twice daily, when initial blood cultures were found to be negative. Paired acute and convalescent serum samples collected on November 5 and December 26 demonstrated a fourfold rise in Y. pestis F1 antigen-specific antibodies, confirming the diagnosis of bubonic plague. She recovered without complication. Public Health ResponseDuring the initial consultations with medical personnel, the couple reported that routine surveillance conducted by the New Mexico Department of Health (NMDOH) had identified Y. pestis in a dead wood rat and fleas collected in July 2002 on their New Mexico property. The hotel physician notified the ED about the arrival of two possible plague patients and the need for respiratory isolation pending the exclusion of pulmonary infection. Hospital infection-control and administration personnel were contacted to coordinate appropriate in-hospital precautions and education. The NYC Department of Health and Mental Hygiene (NYCDOHMH), the New York State DOH, NMDOH, and CDC were contacted to facilitate diagnostic testing, coordinate public health response, and assess the possibility of terrorism. After determining that these two plague cases probably were acquired naturally, a press conference was held to reassure the public that the exposures had occurred in New Mexico, a known plague-endemic area, and not in NYC. Environmental InvestigationOne day after the patients were evaluated, NMDOH and CDC investigated the couple's New Mexico property. Rodent traps were placed in and around the couple's home and along a nearby hiking trail, where wood rat (Neotoma species) nests and rodent burrows were abundant. From 41 trapped rodents, five flea pools comprising 88 fleas were harvested. Laboratory InvestigationsAll fleas were cultured for Y. pestis, and all rodents were bled for culture. Y. pestis isolates from patient 1 and flea samples were compared by using pulsed-field gel electrophoresis (PFGE) and multiple locus variable number tandem repeat assay (MLVA) sequences (1). The PFGE patterns from the isolate of patient 1 and from seven New Mexico flea pools, two obtained in July and five obtained during the November investigation, were indistinguishable. The MLVA pattern of the isolate of patient 1 was similar to the Y. pestis isolates obtained from the same wood rat fleas collected on the couple's property in July and November. The MLVA patterns were distinguishable from other Y. pestis MLVA patterns from surrounding regions. Plague warning signs were placed at trailheads near the couple's property. Plague information pamphlets were distributed in the community, and close neighbors were contacted directly to inform them of the risk for infection in the area. Reported by: DC Perlman, MD, R Primas, MD, B Raucher, MD, R Lis, MD, B Weinberg, MD, A Davilman, C Yampierre, MS, J Protic, MD, Beth Israel Medical Center, New York City; D Weiss, MD, J Ackelsberg, MD, L Lee, MS, M Layton, MD, New York City Dept of Health and Mental Hygiene; ST Beatrice, PhD, New York City Public Health Laboratory; PF Smith, MD, New York State Dept of Health. PJ Ettestad, DVM, PJ Reynolds, CM Sewell, DrPH, New Mexico State Dept of Health. RE Enscore, MS, MY Kosoy, PhD, K Kubota, MPH, JL Lowell, MS, M Chu, PhD, J Kool, MD, KL Gage, PhD, Div of Vector-Borne Infectious Diseases, National Center for Infectious Diseases; CC Chow, MD, CB Smelser, MD, EIS officers, CDC. Editorial Note:Plague is a rodent-associated zoonosis caused by infection with Y. pestis. The disease occurs naturally in 17 western states (Figure), where Y. pestis is maintained through transmission between certain rodents and their fleas. Other mammals also become infected and some, including humans, suffer severe disease and high mortality rates. Human cases are acquired typically through the bites of infectious fleas; the incubation period for plague is usually 2--6 days (2) (Box). During 1988--2002, a total of 112 human cases of plague were reported from 11 western states. The majority (97 [87%]) were exposed in four states (New Mexico [48 cases], Colorado [22], Arizona [16], and California [11]). Approximately 80% of these exposures occurred in peridomestic environments, particularly those that provided abundant food and harborage for flea-infested, plague-susceptible rodents. Travelers can acquire plague in one area and become ill in another area where plague is not endemic (i.e., peripatetic plague) (3--7). Although rare, peripatetic plague is more likely to result in fatal outcomes because of delays in seeking treatment or misdiagnosis in areas where health-care providers might be less familiar with the disease (3--7). In the current state of heightened awareness of possible terrorism, peripatetic cases also might be confused with those arising from an intentional release of plague bacteria. The two cases described in this report did not cause such confusion because the initial history provided a plausible exposure. In addition, both patients had inguinal adenopathy, indicating that transmission was from bites of infectious fleas rather than inhalation of airborne materials, the route considered more likely for terrorism (8). However, intentional release should be considered as a cause of cases occurring outside an area where plague is endemic, particularly for patients with primary pneumonic or primary septicemic plague. Plague prevention depends on the timely implementation of preventive measures, including public education, applying insecticides to kill fleas, using various personal protective measures (e.g., common insect repellents), and avoidance of sick or dead animals (2) (Box). A vaccine is not available in the United States. The rapid identification of peripatetic cases depends on public health surveillance systems that include the availability of laboratory expertise and facilities to provide rapid presumptive evidence and laboratory confirmation of Y. pestis infection. Because NMDOH had identified plague previously on the patients' property, the patients were able to alert clinicians of their potential plague exposure, which enabled early diagnosis and prompt treatment. NYCPHL, which had received training and reagents for diagnosis of Y. pestis as part of a nationwide effort to enhance terrorism response capabilities (9), also performed DFA and PCR analyses that presumptively identified Y. pestis as the bacterium cultured from patient 1. This was later confirmed by phage-lysis and other analyses. Genotyping at CDC indicated that the isolate was indistinguishable from (by PFGE) or highly similar to (by MLVA) an isolate obtained earlier in the year from wood rat fleas collected on the patients' property (10). The findings in this report highlight how clinical, epidemiologic, and laboratory programs can act in a coordinated manner to diagnose peripatetic plague cases rapidly and identify probable exposure sites and sources of infection. Communication between public health and law enforcement agencies remains paramount in the effective diagnosis, treatment, and investigation of infections with potential terrorism agents. These capabilities have been enhanced, particularly in areas such as NYC, where plague is not endemic by a series of efforts undertaken by local, state, and federal agencies to prepare for the possibility of terrorist attacks. Acknowledgments This report is based on data contributed by G Beaudry, W Oleszko, AM Incalicchio, M Wong, S Clark, L Lee, T Rodriguez, New York City Public Health Laboratory, New York. References
Figure 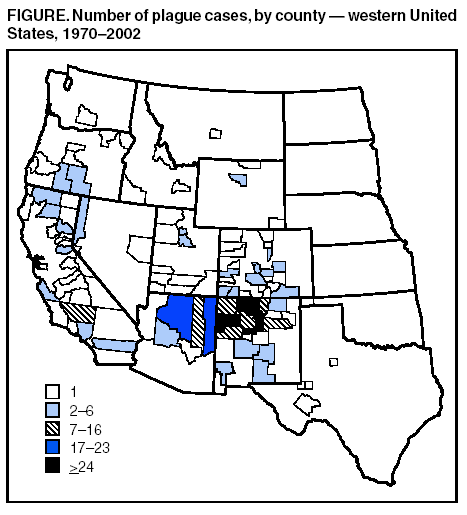 Return to top. Box  Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 8/7/2003 |
|||||||||
This page last reviewed 8/7/2003
|