 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Public Health and Aging: Nonfatal Physical Assault--Related Injuries Among Persons Aged >60 Years Treated in Hospital Emergency Departments --- United States, 2001As the U.S. population ages, public health efforts have expanded to ensure the independence, function, and safety of older adults. Such efforts focus on consequences associated with the normal aging process. The incidence and consequences of violent victimization are assumed to be a problem of young populations and not an area of concern among older populations (1), and little data are available to monitor the incidence or consequences of violence-related injuries among older adults. To characterize serious injuries from physical assaults among older adults, CDC analyzed data from the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP). This report summarizes the results of that analysis, which indicate that approximately 33,000 persons aged >60 years in the United States were treated in hospital emergency departments (EDs) for nonfatal assault--related injuries in 2001, with injuries occurring disproportionately among persons aged 60--69 years. NEISS-AIP data can increase the understanding of nonfatal physical assault--related injuries among older adults and guide the development and evaluation of prevention strategies. NEISS-AIP provides data on approximately 500,000 injury- and consumer product--related ED cases each year (2,3). NEISS-AIP data are drawn from a nationally representative subsample of 66 out of 100 NEISS hospitals, which were selected as a stratified probability sample of hospitals with a minimum of six beds and a 24-hour ED in the United States and its territories. For this analysis, NEISS-AIP provided national, annualized, weighted estimates of nonfatal, nonsexual, physical assault--related injuries among persons aged >60 years who were treated in U.S. EDs during 2001. Data from these cases were weighted by the inverse of the probability of selection to provide annualized national estimates (3). A direct variance estimation procedure was used to calculate 95% confidence intervals and to account for the complex sample design (4). All cases were classified into mutually exclusive categories according to intent (i.e., physical assault, sexual assault, self-inflicted injury, injury related to legal intervention, and unintentional injury) of the most severe injury received. Annualized estimates for this report were based on weighted data for 488 nonfatal physical assault--related injuries treated in EDs during 2001. Suspected and confirmed instances of interpersonal violence were coded as assaults. Data were collected about sex, age, race/ethnicity, diagnosis, cause of injury, body part primarily affected, location, and disposition. To evaluate the "struck by/against" category of injury cause further, CDC analyzed verbatim text comments recorded in the NEISS-AIP database from ED patient charts for each injury. Subcategories of "struck by/against" were defined as body (e.g., hand, fist, elbow, or foot), blunt object (e.g., cane, baseball bat, or butt of gun), and push (i.e., injury sustained by fall secondary to being pushed). The remaining injuries in the "struck by/against" category were classified as unspecified. During 2001, an estimated 33,026 persons aged >60 years were treated in U.S. hospital EDs for nonfatal assault--related injuries (rate: 72 per 100,000 population), compared with an estimated 1,154,579 persons aged 20--59 years (rate: 754.6); 21,309 (65%) persons were aged 60--69 years, 7,064 (21%) were aged 70--79 years, and 4,653 (14%) were aged >80 years (Table). Rates for persons aged 60--69 years (105) were more than two times greater than those for the two older age categories (44 and 49, respectively). The majority (55.4%) of adults aged >60 years who were examined in EDs were men. Older adults were at similar risk for being assaulted at home (25.9%) compared with a public area (27.5%). The types of injuries sustained were primarily contusion/abrasion (31.9%), laceration (21.1%), and fracture (12.7%). Of the classifiable cases, the majority of older adults (83.7%) were injured as a result of being struck by/against, most often by a body part (20.3%), followed by a blunt object (17.1%), push (14.4%), and an undetermined cause (31.8%); 91.3% of assaulted older adults were treated and released from EDs, and 8.3% required hospitalization. Compared with persons aged 20--59 years, a greater proportion of older assault victims were women (43.4% versus 39.1% p = 0.11), had fractures (12.7% versus 9.8% p = 0.61), and were hospitalized at the time of diagnosis (8.3% versus 6.4% p = 0.52); however, these differences were not statistically significant. Reported by: RA Mitchell, Jr, MD, New Jersey Medical School, Newark, New Jersey. L Hasbrouck, MD, E Ingram, PhD, Div of Violence Prevention; C Dunaway, MS, JL Annest, PhD, National Center for Injury Prevention and Control, CDC. Editorial Note:The findings in this report underscore the magnitude of nonfatal physical assault--related injuries among persons aged >60 years. Some of the reported injuries probably represent a form of elder maltreatment (EM). EM refers to acts of commission or omission that result in harm or threatened harm to the health or welfare of an older adult, occurring within any relationship in which there is an expectation of trust (5). The various forms of EM include physical, sexual, and psychological abuse; abandonment; exploitation; and neglect, either intentional or unintentional. Reported EM cases comprise only a fraction of cases. A national incidence study estimated that approximately half a million older persons were maltreated in 1996; however, for every reported incident of EM, an estimated five were unreported (6). The findings in this report are consistent with previous studies that indicate that older adults are less likely to be victims of violent crime than younger persons (7), possibly because younger persons might be at greater risk for violent assault within the broader community. This hypothesis is supported by perpetrator data for fatal assaults among older persons (CDC, unpublished data, 2003). Among younger victims, perpetrators are more likely to be strangers. Among older victims, the perpetrators are more likely to be family members or acquaintances. The findings in this report are subject to at least five limitations. First, NEISS-AIP data are based on information in ED records and are not linked to or supplemented by other data sources (e.g., Adult Protective Services [APS] records). Second, outcomes are specific to ED visits and do not include subsequent outcomes of the injuries. Third, NEISS-AIP data reflect only those injuries that were severe enough to require treatment in an ED. Fourth, NEISS-AIP data might provide a conservative estimate of the number of physical assault--related injuries among older adults treated in EDs because the violent intent of injury might not be reported. Finally, although limited data are presented for settings in which assaults occurred (i.e., home or public area), data for perpetrators of assault-related injuries were unavailable. Injury is a physical sign for EM, and EDs are a key point of contact for its recognition (8). However, reporting rates of EM by hospitals are low, and the majority of ED physicians are uncertain about EM definitions or applicable state laws (6,9). Because the older adult population is expected to more than double by 2025 (5), the number of physical assault--related injuries among the elderly probably will increase, requiring more attention from clinicians and public health agencies. ED workers should be prepared to explore the cause of injuries suggestive of physical assault to ensure that proper referral is made when needed. References
Table 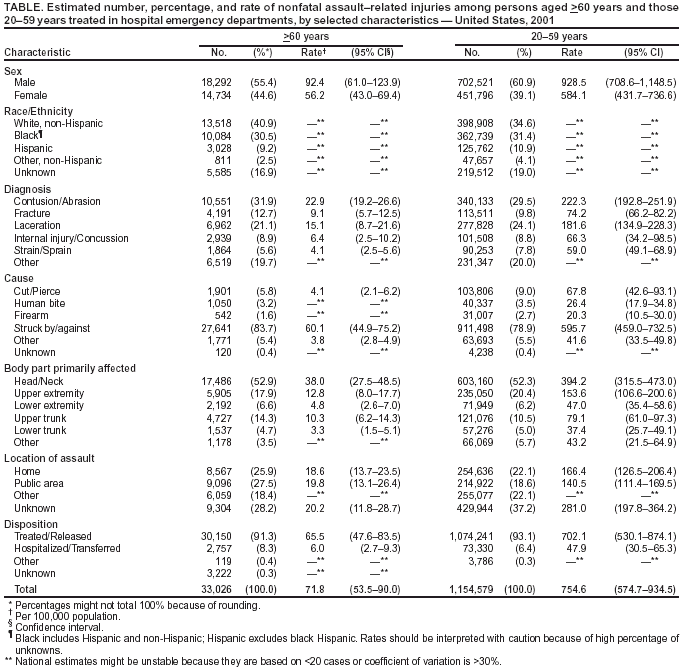 Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 8/28/2003 |
|||||||||
This page last reviewed 8/28/2003
|