 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Increasing Infant Mortality Among Very Low Birthweight Infants --- Delaware, 1994--2000One of the national health objectives for 2010 is to reduce the U.S. infant mortality rate (IMR) to <4.5 deaths per 1,000 live births (objective no. 16-1c) (1). Historically, Delaware's IMR exceeded the national average; however, during the early 1990s, Delaware's IMR decreased, reaching the U.S. average in 1993. During 1995--2000, the overall U.S. IMR decreased from 7.6 to 6.9; since 1996, Delaware's IMR has increased, and the state now has the seventh highest IMR nationally (2). To understand the cause of this increase, the Delaware Division of Public Health and CDC analyzed Delaware birth and death data. This report summarizes the results of the investigation, which attributed the Delaware IMR increase primarily to increased mortality among very low birthweight (VLBW) infants born to older, married, suburban mothers who were insured privately and who received early prenatal care. Further study, including collection of data on method of conception, is required to determine the etiology of the increased mortality in this subpopulation. IMR was analyzed by using a state-based linked birth-death certificate cohort database, which included data on all live births to women residing in Delaware. IMR was averaged by using 3-year increments. Normal birthweight was defined as >2,500 g, moderately low birthweight (MLBW) as 1,500 g--2,499 g, and VLBW as <1,500 g. Plurality was classified as singletons, twins, and triplets-plus (i.e., multiple births of three or more infants). The 3-year period when Delaware's IMR was lowest (1994--1996) was used as a baseline and compared with the most recent 3-year period for which data were available (1998--2000). IMR was adjusted for changes in plurality distribution over time; the plurality-adjusted IMR represents IMR in a given period, assuming the same plurality distribution as in 1994--1996. IMR also was adjusted for changes in birthweight distribution. Stratified analyses were conducted to examine IMR trends within infant birthweight and plurality subpopulations and by maternal characteristics. Use of assisted reproductive technology (ART) procedures in Delaware in 2000 was assessed by using data from the population-based U.S. Registry of ART Procedures maintained by CDC, which includes data on pregnancies and live births conceived through the use of infertility treatment procedures in which both egg and sperm are handled outside the body (e.g., in vitro fertilization). Delaware's IMR increased from 7.1 deaths per 1,000 live births during 1994--1996 to 8.7 during 1998--2000; the rate of twin births increased from 2.8% to 3.3%, the rate of triplets-plus births was unchanged (0.2%), and the VLBW rate increased from 1.7% to 1.9% (Table 1). Adjusting for plurality distribution did not alter the observed IMR trend significantly (Figure). Adjusting for birthweight distribution attenuated the IMR trend, but a 16% increase remained. Analysis of birthweight-specific mortality indicated that IMR among normal birthweight and MLBW infants did not change significantly; however, IMR among VLBW infants increased 25%, from 235 to 294 (p = 0.03). When the birthweight-adjusted IMR was analyzed while IMR among VLBW infants was held constant, the IMR trend no longer was evident. Examination of VLBW infants indicated increased mortality among all plurality subpopulations: 8% for singletons (from 261 to 283; p = 0.6), 93% for twins (from 160 to 315; p = 0.03), and 304% for triplets-plus (from 95 to 385; p = 0.08). During 1998--2000, VLBW singletons accounted for 26% of the excess mortality, and twins and triplets-plus accounted for 54% and 20%, respectively. Analyses of birthweight in 500-gram increments indicated that the IMR trend was not attributable to an increase in extremely LBW infants (i.e., those weighing <1,000 g), because neither the proportion of infants weighing <500 g nor that of infants weighing <1,000 g increased. Among VLBW infants, the largest increase (67%) in IMR (from 29 to 48; p = 0.3) was among infants weighing 1,000 g--1,499 g. The distribution of maternal demographic and pregnancy factors during 1994--1996 was similar to that during 1998--2000 (Table 2). Analyses of IMR trends among VLBW infants according to these factors (Table 3) revealed statistically significant increases in IMR for infants of mothers who were aged >30 years, were married, had prenatal care during their first trimester, were insured privately, and resided in New Castle County excluding Wilmington (i.e., Delaware's only predominantly suburban area). The increase in IMR for infants of mothers who had at least a high school education approached statistical significance (p = 0.06). Increased use of and improved success rates for ART have led to an increase in the annual number of ART-conceived infants born to Delaware residents. ART use has increased in surrounding states, which might have provided ART services to Delaware residents (3). During 1996--2000, the number of ART procedures performed in Delaware increased 13%. In 2000, an estimated 113 (1%) of the 11,046 live births recorded in Delaware were conceived with the use of ART; however, ART-conceived infants accounted for approximately 8% of VLBW infants born in 2000. Among multiple-birth infants born in Delaware in 2000, an estimated 56% were born through natural conception; this estimate was made on the basis of national multiple-birth rates in 1971, before the widespread use of infertility drugs or ART. On the basis of births reported to the ART registry, approximately 17% of the multiple births in 2000 were attributable to ART; the other approximately 28% likely were attributable to other non-ART infertility treatments. Reported by: AL Hathcock, PhD, P Silverman, DrPH, Div of Public Health, Delaware Health and Social Svcs. C Ferré, MS, MA Reynolds, PhD, LA Schieve, PhD, Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; M Drees, MD, EIS Officer, CDC. Editorial Note:The findings in this report indicate that the IMR increase in Delaware is attributable primarily to increased mortality among VLBW infants. Analysis of maternal risk factors suggested that mortality rates were higher among infants born to women of higher socioeconomic status (SES) as indicated by age, marital status, education level, suburban residence, insurance status, and access to early prenatal care. A trend toward higher LBW rates among mothers with higher SES has been reported previously for births in Massachusetts (4); however, that study did not evaluate the impact on IMR trends. The etiology of this excess mortality is uncertain. ART and other infertility treatments might increase risk for poor outcomes. Women who undergo ART are more likely to deliver preterm and to undergo Cesarean section, even with singleton pregnancies (5), and they have a higher risk for preeclampsia (6). ART is a well-recognized factor in the increasing multiple-birth rate in the United States. Evidence exists that singletons born through use of ART have higher rates of LBW (7) and congenital malformations (8) than infants who were conceived naturally. Because insurance coverage for ART often is limited or lacking (and is not mandated in Delaware), parents of infants conceived from these treatments tend disproportionately to have high SES. Studies also suggest that other infertility treatments (e.g., ovarian stimulation) increase the risk for adverse infant outcomes (9). These treatments are less well studied. Infertility itself might result in lessened capacity to maintain a healthy pregnancy. Higher rates of LBW have been observed among subfertile couples who take >1 year to conceive but do not undergo infertility treatment (10). The findings in this report are subject to at least three limitations. First, some trends noted in this report should be interpreted with caution because numbers of infant deaths among certain subpopulations were small, a common occurrence in smaller states. Second, although ART might have an increasing impact on births in Delaware generally, the hypothesis that the increase in ART births contributed to the increasing IMR in Delaware could not be evaluated. Because the method of conception is not recorded on Delaware birth certificates, analyses of ART were based on comparison between two unlinked data sources. ART births were estimated from a registry that includes approximately 95% of all ART conceptions, and no means were available to account for migration between conception and birth. In addition, although the ART registry includes data on plurality and birthweight, it is not designed to capture infant mortality. Finally, no data are available on which to base an evaluation of the contributions of births conceived using non-ART infertility treatments or, with the national trend toward delayed childbearing, an increase in conceptions among subfertile couples. Changes in prenatal care practices might have contributed to Delaware's increased IMR. Timing of initiation of prenatal care could be established by using vital statistics data, but quality and content of prenatal care could not. Differences might have affected maternal, fetal, and infant health, and might have affected some subpopulations more negatively than others. Prepregnancy health also could not be assessed, nor could the contribution of changes in fetal survival and subsequent early neonatal death. The finding that the heaviest VLBW infants (1,000 g--1,499 g) had the greatest increases in mortality suggests the need for more detailed study of this subpopulation. Limiting the number of embryos transferred with ART will help reduce multiple births. Recording the method of conception on birth certificates, as has been initiated in Massachusetts, would provide additional data about risk for infant mortality resulting from infertility treatments. Further study is required to assess the direct contribution of infertility treatments and changes in prenatal care strategies to infant mortality. Acknowledgments This report is based on assistance provided by T Jarrell, PhD, Delaware Health Statistics Center, Div of Public Health, Delaware Health and Social Svcs. A De, PhD, Div of Applied Public Health Training, Epidemiology Program Office, CDC. References
Table 1 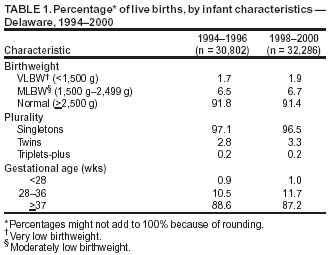 Return to top. Table 2 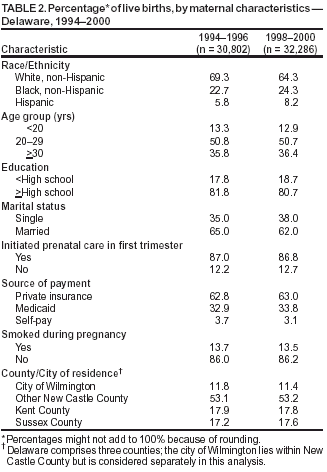 Return to top. Table 3 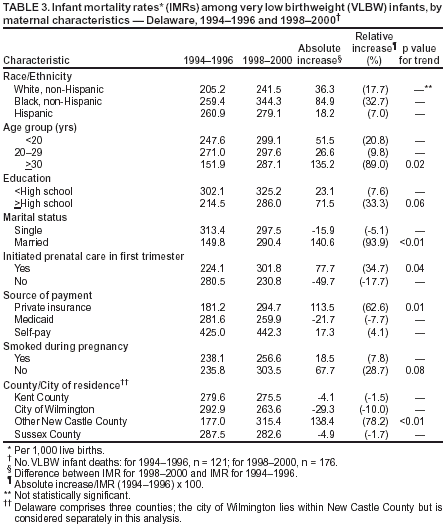 Return to top. Figure 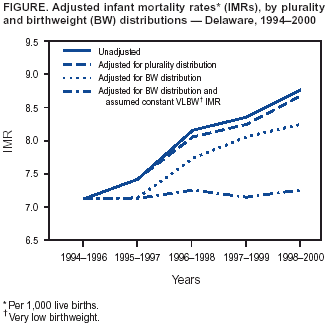 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 9/11/2003 |
|||||||||
This page last reviewed 9/11/2003
|