 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Local Transmission of Plasmodium vivax Malaria --- Palm Beach County, Florida, 2003The majority of malaria cases diagnosed in the United States are imported, usually by persons who travel to countries where malaria is endemic (1). However, small outbreaks of locally acquired mosquito-transmitted malaria continue to occur (2). Despite certification of malaria eradication in the United States in 1970 (3,4), 11 outbreaks involving 20 cases of probable locally acquired mosquito-transmitted malaria have been reported to CDC since 1992 (5--7), including two reported in July 1996 from Palm Beach County, Florida (Palm Beach County Health Department, unpublished data, 1998). This report describes the investigation of seven cases of locally acquired Plasmodium vivax malaria that occurred in Palm Beach County during July--August 2003. In addition to considering malaria in the differential diagnosis for febrile patients with a history of travel to malarious areas, health-care providers also should consider malaria as a possible cause of fever among patients who have not traveled but are experiencing alternating fevers, rigors, and sweats with no obvious cause. Case ReportsCase 1. On July 24, a man aged 37 years was admitted to hospital A with a 6-day history of fever, chills, headache, anorexia, and vomiting. On July 25, P. vivax was identified on a blood smear. The patient recovered after treatment with doxycycline, quinine, and primaquine. The patient is a plumber who reported working outside during the day but who stayed indoors at night. Case 2. On July 22, a man aged 46 years reported to the emergency department (ED) of hospital A with a 3-day history of fever, headache, chills, anorexia, nausea, vomiting, dehydration, and malaise. He was treated with intravenous fluids and discharged with levofloxacin. On July 24, he returned to the ED with worsening symptoms and was admitted with a diagnosis of pneumonia. On July 25, P. vivax was identified on a blood smear. The patient recovered after treatment with doxycycline, quinine, and primaquine. The patient is a construction worker who reported working outside. Case 3. On August 15, a man aged 32 years was admitted to hospital A with a 33-day history of fever, chills, headache, vomiting, and intermittent sweating. He had consulted several physicians for his symptoms and had been treated unsuccessfully with azithromycin and prednisone. On the day of admission, P. vivax was identified on a blood smear. The patient recovered after treatment with doxycycline, quinine, and primaquine. He reported having played golf and tennis in the evenings. Case 4. On August 19, a man aged 45 years visited the ED of hospital A with a 2-day history of fever, chills, anorexia, arthralgias, and diarrhea and was discharged on ibuprofen. The patient visited the ED again on August 21 for these same symptoms, was evaluated, and discharged. On August 22, he returned to the ED with worsening symptoms and mental confusion and was admitted; a blood smear demonstrated the presence of P. vivax. He recovered after treatment with chloroquine and primaquine. The patient slept in a homeless camp in a wooded area near a canal. He reported using insect repellent. Case 5. On August 24, a man aged 23 years was admitted to hospital A with a 12-day history of fever, chills, arthralgias, diarrhea, and vomiting. On the day of admission, P. vivax was identified on a blood smear. He had visited the ED several days previously with the same complaints and had been treated with antibiotics for a respiratory infection. The patient recovered after treatment with chloroquine and primaquine. He reported fishing at a community pond in the evenings. Case 6. On August 25, a person aged 17 years was admitted to hospital B with an 8-day history of fever, chills, and headaches. On August 26, P. vivax was identified on a blood smear. He recovered after treatment with doxycycline, quinine, and primaquine. The patient is a student and reported spending time at a pond near his house. Case 7. On August 26, a man aged 48 years was admitted to hospital C with a 7-day history of fever and chills. He had self-treated earlier that week with antibiotics. P. vivax was identified on a peripheral blood smear on the day of admission. He recovered after treatment with chloroquine and primaquine. The patient is a carpenter and works until 8 p.m. in an open warehouse. Epidemiologic InvestigationAll seven patients reported having no previous history of malaria, recent blood transfusion, organ transplantation, or intravenous drug use. Six of the seven patients reported never having traveled to regions where malaria is endemic. Patient 7 emigrated to the United States from Bogota, Colombia, in July 2001; although Bogota is free of malaria transmission, malaria is endemic in some areas of Colombia. All seven patients live within the West Palm Beach area (Figure) within 10 miles of Palm Beach International Airport. No international seaport exists nearby. Patients 1 and 2 attended the same local party on July 4. None of the other patients had any known common activities or interactions. Laboratory InvestigationBlood specimens were reviewed, and P. vivax infection was confirmed by both microscopic diagnosis and polymerase chain reaction rRNA gene analysis. In addition, parasite multilocus genotyping confirmed that all seven patients were infected by the same strain of P. vivax. Entomologic InvestigationTargeted mosquito trapping was conducted within 1 mile of the homes of patients. Anopheles quadrimaculatus (n = 33) and An. crucians (n = 425) were tested by CDC. None demonstrated the presence of malaria parasites. Prevention Measures and Enhanced Surveillance ActivitiesSeveral strategies to prevent further transmission of malaria and to enhance case detection were implemented by the Palm Beach County Health Department. Reverse 911 telephone calls delivering a prerecorded message, warning of the presence of malaria in the region and advising the use of prevention measures, were made to all homes in the county; approximately 300,000 residents were reached. Postcards in multiple languages were mailed to residents. Flyers and posters in English and Spanish were distributed at soup kitchens, trailer parks, and at outdoor activities at which persons were at high risk for malaria. Local media were encouraged to provide relevant malaria messages in multiple languages. Multilingual notices were sent home with all public school students. Several local homeless camps were visited to distribute brochures and insect repellent. Case-finding was conducted after reports of fever in these camps. One person was evaluated for malaria, but his smears did not demonstrate the presence of malaria parasites. Notices were sent to local physicians and hospitals by e-mail, fax, and mail, informing them of the presence of malaria and requesting information and advising testing for persons with a history of unexplained fever. Mosquito-control practices were already in place in Palm Beach County for control of the West Nile virus vector and nuisance mosquitoes. Additional mosquito spraying was implemented within a 3-mile radius of the homes of each malaria patient. Reported by: JM Malecki, MD, S Kumar, MD, BF Johnson, ML Gidley, TE O'Connor, J Petenbrink, Palm Beach County Health Dept; L Bush, MD, J Morand, MT Perez, MD, JFK Hospital, Palm Beach County; S Pillai, PhD, L Crockett, MD, C Blackmore, DVM, Florida State Health Dept; E Bradford, Palm Beach County Mosquito Control, Florida. RA Wirtz, PhD, JW Barnwell, PhD, AJ DaSilva, PhD, LM Causer, MBBS, ME Parise, MD, Div of Parasitic Diseases, National Center for Infectious Diseases, CDC. Editorial Note:This outbreak shares common features with other outbreaks of malaria reported previously in the United States, including 1) an initial introduced case without risk factors for malaria, 2) presence of competent malaria vectors, 3) proximity to a person with malaria parasitemia, and 4) environmental conditions conducive to the maturation of the parasite in the mosquito. Possible infected persons providing a source for this outbreak in Palm Beach County include both international travelers and the immigrant population, including migrant farm laborers from Mexico and Central and South America. This outbreak represents the first reported outbreak of malaria with extended transmission in the United States since 1986 (8,9). Early cases might have been sources of subsequent cases or ongoing transmission might have resulted from an index patient with unresolved parasitemia being the source for each subsequent case. Also unique to this outbreak has been the use of molecular techniques to genetically type the strain of the infecting parasite. These results support the hypothesis that this cluster of cases was the result of extended malaria transmission originating from a single infected person. This outbreak demonstrates the potential for reintroduction of malaria into the United States despite intensive surveillance, vector-control activities, and local public health response to educate clinicians and the community. Rapid recognition, accurate diagnosis, and appropriate case management are essential for limiting the spread of a malaria outbreak. If an outbreak has occurred, clinicians must consider malaria in the diagnosis of any patient with fever without apparent cause. Prevention of mosquito bites through personal protection measures (e.g., using insect repellent containing DEET) and vector control are important measures to limit transmission. Risks for locally acquired malaria are unlikely to abate given migration and travel patterns and a global yearly malaria burden of 300--500 million cases and one million deaths. However, prompt reporting of patients with malaria to public health authorities and adequate assessment of risk factors for malaria in all cases allows initiation of an appropriate public health response to prevent reestablishment of malaria transmission. References
Figure 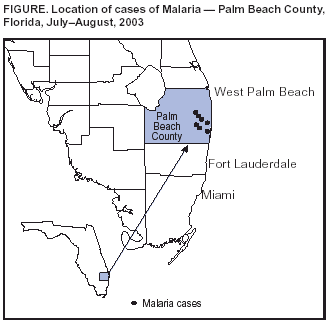 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 9/25/2003 |
|||||||||
This page last reviewed 9/25/2003
|