 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Racial/Ethnic Disparities in Influenza and Pneumococcal Vaccination Levels Among Persons Aged >65 Years --- United States, 1989--2001Influenza and pneumococcal diseases are key causes of mortality among persons aged >65 years, accounting for approximately 36,000 and 3,400 deaths per year, respectively, during 1990--1999 (1,2). Substantial racial/ethnic disparities in adult vaccination have been documented in national surveys (2,3). Although the national health objective for 2000 of 60% receipt of influenza vaccination during the preceding 12 months by persons aged >65 years (objective no. 20.11) was met in 1997, and the objective of 60% for pneumococcal vaccination was nearly met in 2000, vaccine coverage levels among non-Hispanic blacks and Hispanics were 31% and 30%, respectively, compared with 57% for non-Hispanic whites (4,5). To characterize these disparities, CDC analyzed data from the 2000 and 2001 National Health Interview Surveys (NHIS) and examined trends in NHIS results for 1989--2001. This report summarizes the results of these analyses, which indicate that marked differences in vaccination coverage by race/ethnicity are observed even among persons most likely to be vaccinated (e.g., persons with the highest education level and persons with frequent visits to health-care providers). Racial/ethnic disparities in influenza and pneumococcal vaccination coverage have persisted over time. Several approaches to reduce these disparities are needed, including increasing demand for vaccination among racial/ethnic minority populations and the use of standing orders and other systems changes that promote vaccination. The 2000 and 2001 NHIS adult core questionnaires were administered by personal interview to a nationally representative sample of the U.S. civilian, noninstitutionalized population aged >18 years; the response rate was 72% in 2000 and 74% in 2001. In both years, respondents aged >65 years were asked, "During the past 12 months, have you had a flu shot?"; in 2000, they were asked, "Have you ever had a pneumonia vaccination, sometimes called a pneumonia shot?"; and in 2001, they were asked, "Have you ever had a pneumonia shot?" Vaccine receipt was tabulated for non-Hispanic whites, non-Hispanic blacks, and Hispanics and stratified by selected demographic variables. Respondents who refused to answer the question or who reported an unknown status for influenza or pneumococcal vaccination were excluded from the analyses (1.4% and 3.5% for influenza and pneumococcal vaccination, respectively). NHIS data from 2000 and 2001 were combined to provide more precise estimates of vaccine coverage in the stratified analysis. Trends by survey year in reported vaccine coverage by race/ethnicity were examined based on responses to the 1989--2001 surveys, which used similarly worded questions. Vaccination questions were not included on the 1990, 1992, and 1996 surveys. For these years, a midpoint value between the preceding and the next year was assigned. Data were adjusted for nonresponses and weighted to provide national estimates. SUDAAN was used to calculate point estimates and 95% confidence intervals (CIs) and to conduct multivariable logistic regression analysis to assess the independent association between race/ethnicity and vaccination status while controlling for other sociodemographic factors. During 2000--2001, a total of 9,435 non-Hispanic white, 1,341 non-Hispanic black, and 1,133 Hispanics aged >65 years were included in the analyses. A lower proportion of non-Hispanic blacks and Hispanics had >12 years of education than non-Hispanic whites (22% and 19% versus 37%), were above poverty level* (31% and 33% versus 63%), and had supplemental insurance (i.e., any insurance in addition to Medicare, except Medicaid) (39% and 26% versus 73%). A higher proportion of Hispanics than non-Hispanic blacks or whites had fewer than two doctor visits during the preceding 12 months (24% versus 18% and 17%). A similar proportion in each of the three racial/ethnic populations reported >10 doctor visits during the preceding 12 months (21% of non-Hispanic whites, 22% of non-Hispanic blacks, and 25% of Hispanics). During 2000--2001, the average influenza and pneumococcal coverage levels reported, respectively, were 66% and 57% for non-Hispanic whites, 48% and 33% for non-Hispanic blacks, and 54% and 32% for Hispanics (Table). In general, influenza vaccination coverage was highest for non-Hispanic whites, followed by Hispanics and then non-Hispanic blacks (Table); for pneumococcal vaccination, coverage was similar for non-Hispanic blacks and Hispanics. Vaccine coverage was <60% for all subgroups of non-Hispanic blacks and the majority of subgroups of Hispanics. After accounting for variations in sex, age, education, poverty status, region, insurance status, number of doctor visits, and high-risk conditions, non-Hispanic blacks remained significantly less likely than non-Hispanic whites to report influenza vaccination (odds ratio [OR] = 0.7; 95% CI = 0.6--0.8); the difference between Hispanics and non-Hispanic whites was not statistically significant (OR = 0.9; 95% CI = 0.7--1.1). Both non-Hispanic blacks and Hispanics were significantly less likely than non-Hispanic whites to report a pneumococcal vaccination (OR = 0.4; 95% CI = 0.3--0.5 and OR = 0.4; 95% CI = 0.3 and 0.5, respectively). During 1989--1999, national influenza vaccination coverage increased nearly each survey year for non-Hispanic whites, non-Hispanic blacks, and Hispanics, but the rate of increase has declined since 1997 (Figure 1). A slight decline was observed in 2001, probably reflecting delays in influenza vaccine manufacturing and distribution in 2000 (1). In 2001, differences in influenza coverage between non-Hispanic whites and Hispanics and between non-Hispanic whites and blacks were 13 and 16 percentage points, respectively; in 1989, these differences were 8 and 14 percentage points, respectively. Pneumococcal vaccination has increased steadily; however, the increase for non-Hispanic whites during 2000--2001 was smaller than previous annual increases (Figure 2). In 2001, differences in pneumococcal vaccination coverage between non-Hispanic whites and Hispanics and between non-Hispanic whites and blacks were 25 and 23 percentage points, respectively, and 5 and 9 percentage points in 1989. Reported by: CR Stein, Association of Schools of Public Health, Atlanta, Georgia. PM Wortley, Immunization Svcs Div; JA Singleton, Epidemiology and Surveillance Div, National Immunization Program, CDC. Editorial Note:The findings in this report indicate that although influenza and pneumococcal vaccination rates have increased for non-Hispanic blacks and Hispanics, as they have for non-Hispanic whites, substantial gaps persist by race/ethnicity. Differences in coverage are observed among persons with similar education levels, similar numbers of health-care encounters, and similar insurance status. These differences remain after controlling for factors with multivariable analysis, with the exception of receipt of influenza vaccination among Hispanics. Increases in vaccination rates for non-Hispanic blacks and Hispanics have not occurred at a rate sufficient to reach the national health objective for 2010 of eliminating disparities in health. Among non-Hispanic whites, influenza vaccination coverage was stable during 1997--2001 at <70% (2), and for all three groups, coverage was below the 90% health objective for 2010. Reasons for differences in coverage are poorly understood. In this analysis, substantial racial/ethnic disparities in vaccination coverage were observed among persons with zero to one, two to nine, and >10 health-care provider contacts during the preceding 12 months, suggesting that access to care might not be a key factor. In the 1996 Medicare Current Beneficiary Survey, race/ethnicity was not related to reasons given for not being vaccinated (6). For influenza vaccination, the two leading reasons for not being vaccinated were not knowing it was recommended and concerns about the vaccine (e.g., fear of getting influenza and fear of side effects); for pneumococcal vaccination, the leading reason for not being vaccinated was not knowing it was recommended. Determining the reasons for the racial/ethnic disparity requires further examination. Possible reasons might include non-Hispanic blacks and Hispanics receiving care disproportionately in settings in which vaccination coverage is lower or differences in the provider-patient interaction for non-Hispanic blacks and Hispanics compared with non-Hispanic whites. CDC is addressing these disparities through 2-year demonstration projects in Chicago, Illinois; Milwaukee, Wisconsin; a rural area of Mississippi; Rochester, New York; and San Antonio, Texas. In these areas, local and state health departments are working with community partners and federal agencies to improve influenza and pneumococcal vaccination levels among elderly non-Hispanic blacks and Hispanics. Strategies include development of culturally specific messages, working with health-care providers who care for elderly non-Hispanic black and Hispanic patients to implement effective interventions (e.g., standing orders and provider reminders) (7), and conducting vaccination clinics in underserved neighborhoods. A critical outcome of the demonstration project is development of new partnerships to reach populations that have not been targeted. The findings in this report are subject to at least two limitations. First, self-reports of pneumococcal vaccination are less reliable than self-reports of influenza vaccination, in part because the recall usually is longer (8). Second, validity of self-report of vaccination by race/ethnicity has not been studied, and differential validity by race/ethnicity could affect these findings. System changes that promote adherence to evidence-based guidelines play a key role in reducing disparities (9). The absence of racial/ethnic disparities in Veteran's Administration clinics, in which standing orders and other interventions to increase vaccination have been implemented, suggests that this approach might be effective in eliminating disparities (10). In addition, programs are needed to increase demand for vaccination among older non-Hispanic blacks and Hispanics through state and local outreach programs and coalitions to engage new partners. References
*Calculated on the basis of U.S. Census Bureau 2000 poverty thresholds. Figure 1 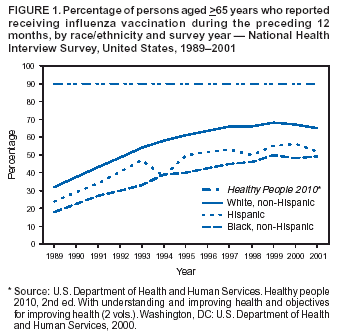 Return to top. Figure 2 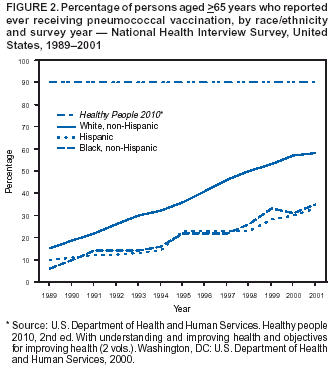 Return to top. Table 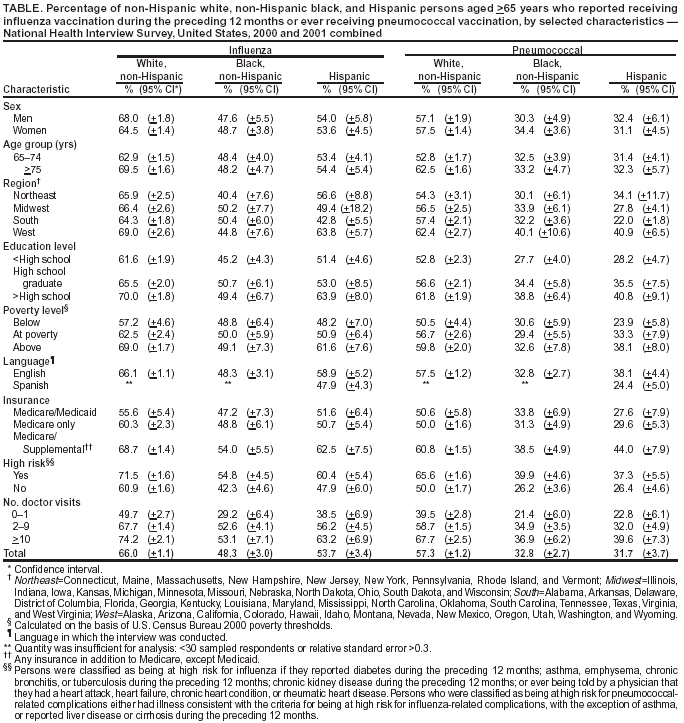 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/9/2003 |
|||||||||
This page last reviewed 10/9/2003
|