 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Partner Counseling and Referral Services to Identify Persons with Undiagnosed HIV --- North Carolina, 2001Approximately one fourth of the 850,000--950,000 persons living with human immunodeficiency virus (HIV) in the United States are not aware of their infection and their risk for transmitting HIV (1). Identifying HIV-infected persons promptly after infection and directing them to medical care and prevention services is a national priority. Voluntary partner counseling and referral services (PCRS) help HIV-infected persons notify sex and needle-sharing partners of their need for HIV testing, enabling partners to receive early care and prevention counseling (2). To evaluate the success of these services in North Carolina, CDC analyzed PCRS data collected in 2001 by the North Carolina Department of Health and Human Services (NCDHHS). This report summarizes the results of that analysis, which determined that 125 (20.5%) of 610 tested partners of HIV index patients had HIV infections that were undiagnosed previously. These findings suggest that local and state health departments should consider PCRS an essential component of any comprehensive HIV-prevention program. In 1989, NCDHHS began offering PCRS to clients who tested HIV positive in confidential and anonymous testing venues. HIV infections were made reportable in 1990, and anonymous counseling and testing services were discontinued in 1997. PCRS in North Carolina is conducted by a disease intervention specialist (DIS), a trained health-care professional who 1) investigates health-care provider or laboratory reports of new HIV infections; 2) verifies that patients have not been reported as HIV positive previously; 3) contacts patients' health-care providers to initiate PCRS and obtain demographic and clinical information; 4) conducts voluntary, confidential interviews requesting information regarding all sex and needle-sharing partners during the preceding year; 5) assesses potential for partner violence; and 6) ensures that index patients receive HIV-prevention counseling, care, and case management. After obtaining partner information, the DIS searches confidential public health records to identify partners reported previously with HIV infection and then contacts the remaining partners to inform them they might have been exposed to HIV. All notified partners receive risk-reduction counseling and appropriate referrals; partners are either referred to clinic-based HIV testing services or provided voluntary testing in the field. The DIS attempts to document that all locatable partners are notified and receive or decline HIV testing. This analysis used data collected in 2001 regarding index-patient demographics and partner notification and testing outcomes. Pearson chi square and Fisher's exact test were used to test associations between partner outcomes and the age, race/ethnicity, HIV-exposure category, and diagnosing clinic type (i.e., public or private) of index patients. For PCRS outcomes significant at the p<0.05 level, pairwise comparisons were performed by using a Bonferoni adjustment for multiple comparisons. In 2001, a total of 1,603 persons were newly reported with HIV infection in North Carolina. DIS personnel were assigned to conduct PCRS with 1,580 (99%) of these index patients; 1,379 (87%) were located and interviewed. Through PCRS, 1,532 sex or needle-sharing partners were identified; the partner index (i.e., number of identified partners divided by number of index patients interviewed) was 1.1. Of the 1,532 named partners (Figure), 173 (11%) could not be notified, 592 (39%) had been tested previously for HIV, and 767 (50%) had not been tested previously for HIV. Among the 592 partners tested previously for HIV, 404 (68%) had tested HIV positive. Among the remaining 188 partners who had tested HIV negative previously and were notified, 122 (65%) were retested; 17 (14%) of those retested were HIV positive. Among the 767 partners not tested previously for HIV infection, 488 (64%) were tested after PCRS; 108 (22%) of those newly tested partners were HIV positive. Overall, one new HIV case was diagnosed for every 11 index patients interviewed through PCRS. Among the 1,128 partners (i.e., 1,532 identified partners minus the 404 known positives) not known to have tested HIV positive previously, 955 (85%) were notified and counseled; 610 (64%) of those 955 were tested or retested for HIV infection; 125 (20%) of the 610 tested positive for HIV infection. Among persons testing positive, 121 (97%) received their test results; four could not be contacted. The proportion of index patients located and interviewed did not vary significantly by age, race/ethnicity (Table 1), or HIV-exposure category. Index patients whose HIV infections were diagnosed in private facilities were slightly less likely to be located and interviewed than those with infections diagnosed in public facilities (Table 2); however, in both venue types, the yield was high (>85%). Partners of index patients whose HIV infections were diagnosed in private facilities also were less likely to have tested HIV positive previously, to have been notified and counseled by a DIS, and to have received HIV testing after PCRS (Table 2). Partners of non-Hispanic white index patients were more likely than partners of non-Hispanic black and Hispanic index patients to be notified and counseled but less likely to have received HIV testing after PCRS (Table 1). The proportion of tested partners with newly diagnosed HIV did not vary by index patient age, race/ethnicity, HIV-exposure category, or diagnosing clinic type. Reported by: E Foust, MPH, P Leone, MD, T Vanhoy, J Owen-O'Dowd, M Hilton, D Williams, PhD, Div of Public Health, North Carolina Dept of Health and Human Svcs. GR Burstein, MD, HY Kim, PhD, S Dooley, MD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:After receiving an HIV-positive test result, patients often reduce or discontinue behaviors that might lead to further HIV transmission (3). The results of this analysis indicate that PCRS can effectively identify sex and needle-sharing partners with previously undiagnosed HIV infection. Among 610 partners tested or retested for HIV infection after PCRS, 125 (20.5%) tested positive for HIV. In contrast, of the 109,172 HIV tests performed in 2001 at HIV counseling and testing sites in North Carolina, only 764 (0.7%) were positive. Among the 1,359 partners who were notified and counseled, 767 (56.4%) had not been tested previously, suggesting that PCRS can be effective in locating persons at risk for HIV infection who are not receiving HIV counseling and testing services through other programs. Certain persons continue high-risk behaviors even after learning they are HIV positive or at risk for infection. Of the 1,532 partners identified, 404 (26.4%) had tested HIV positive previously, indicating that PCRS can locate HIV-positive persons who remain at high risk for transmitting infection and refer them to prevention case management and care. Through retesting, PCRS also identified 17 (13.9%) HIV-positive partners among 122 who had tested negative previously, suggesting that certain persons who test HIV negative continue to engage in high-risk behavior and need reassessment of HIV status and ongoing prevention services. A new CDC initiative, Advancing HIV Prevention: New Strategies for a Changing Epidemic, is aimed at reducing barriers to early diagnosis of HIV infection and increasing access to quality medical care, treatment, and ongoing prevention services (4). A key strategy in the initiative is preventing new infections by counseling HIV-positive persons and their partners. PCRS can be a cost-effective method for combating the spread of HIV infections (5--7). Successful programs will require 1) extensive work with the community and health-care providers to gain support for PCRS; 2) intensive DIS training, close supervision, and quality assurance; and 3) full integration of PCRS into a comprehensive program of HIV care and prevention services. CDC helps fund comprehensive local and state programs aimed at reducing HIV transmission. Because PCRS is an effective counseling and testing strategy that targets persons at high risk for HIV, CDC requires funded health departments to include PCRS among their HIV-prevention services. Because PCRS cannot function effectively in isolation, health officials should work closely with community-based organizations and other service providers to develop strategies for integrating PCRS into a comprehensive counseling, testing, referral, and care program (8). References
Table 1 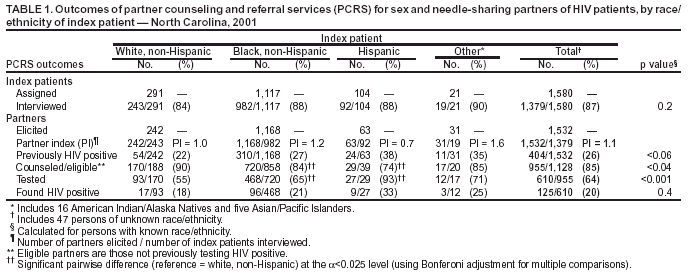 Return to top. Table 2 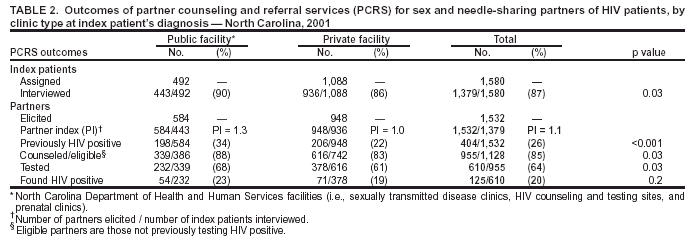 Return to top. Figure 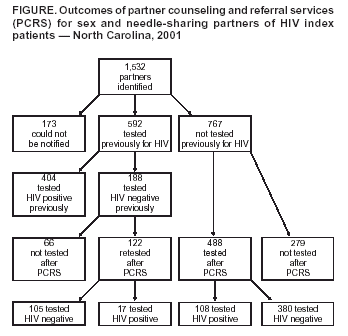 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 12/4/2003 |
|||||||||
This page last reviewed 12/4/2003
|