 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Prenatal HIV Testing and Antiretroviral Prophylaxis at an Urban Hospital --- Atlanta, Georgia, 1997--2000In 1994, the U.S. Public Health Service (USPHS) recommended the use of zidovudine (ZDV) to reduce perinatal human immunodeficiency virus (HIV) transmission; in 1995, USPHS recommended universal prenatal HIV counseling and voluntary testing (1,2). Widespread implementation of these recommendations, together with increased use of antiretroviral therapy (ART) and scheduled cesarean delivery, has resulted in substantial declines in perinatal HIV transmission (3--5). However, perinatal HIV transmission continues to occur (3). To identify missed prevention opportunities, CDC analyzed the incidence of perinatal HIV infection among a cohort of HIV-exposed infants born during 1997--2000 at Grady Memorial Hospital (GMH) in Atlanta, Georgia. This report describes the results of that analysis and underscores the challenges to universal prevention of infant HIV infections. Efforts to reduce perinatal HIV transmission should focus on increasing prenatal care rates, promoting adherence to recommended treatment regimens during pregnancy, and increasing prenatal HIV testing, particularly in areas where missed opportunities for prevention of perinatal HIV transmission persist. All children born to women identified as HIV infected and delivered at GMH during 1997--2000 were included in this analysis. The 2000 birth cohort was the most recent cohort for which complete data on perinatal HIV transmission were available. Women usually met with trained HIV counselors in groups of two to five women during their initial prenatal visits. Pregnant women were provided pretest counseling and asked to give written informed consent for HIV-antibody testing. Since September 1994, the rate of HIV-testing acceptance has been >90% among women registered for prenatal care at GMH; acceptance of maternal and infant ZDV among HIV-infected women also has been >90% (6). Since 1999, scheduled cesarean delivery has been recommended routinely to HIV-infected pregnant women at GMH. The incidence of perinatal HIV transmission was calculated as the number of HIV-infected children divided by the total number of children born to HIV-infected mothers. Children exposed to HIV perinatally were followed at the GMH pediatric HIV clinic. A child with two positive HIV DNA polymerase chain reaction (PCR) tests was classified as HIV infected; a child with at least one negative DNA PCR test after age 2 months or a negative HIV-antibody test after age 18 months was classified as uninfected. The risk for perinatal HIV transmission was 5% in 1997 and 8% in 1998. A low of 3% was reached among HIV-exposed infants born during 1999, coincident with an increased percentage of HIV-infected pregnant women receiving a scheduled cesarean delivery and combination ART and an increased percentage with HIV viral loads of <1,000 copies/mL during the peripartum period (Table). During 1999, dual- or triple-drug ART was administered to 29 (58%) of 50 pregnant HIV-positive women, compared with eight (16%) of 51 women during 1997 (p<0.001). The percentage of pregnant women receiving no ART did not change significantly during the study period (Table). The percentage of women with viral loads of <1,000 copies/mL near the time of delivery increased from 10% in 1997 to 48% during 1999--2000 (p<0.001). For all 54 exposed infants born in 1999 for whom information was available, maternal HIV testing had been performed in time (i.e., prenatally or at the time of delivery) for the infants to receive the recommended 6-week course of postnatal ZDV prophylaxis. Scheduled cesarean delivery rates increased from one (1%) of 114 women during 1997--1998 to 46 (37%) of 125 women during 1999--2000 (p<0.001). During 1999--2000, nine HIV-infected infants were born at GMH. Neither of the mothers of the two infected infants born in 1999 had prenatal care, nor did they know their HIV-infection status during pregnancy. One of the mothers was an active cocaine user who went into labor after rupture of the fetal membranes. Both infected infants received ZDV prophylaxis postnatally (i.e., within 24 hours after birth) but not intrapartum. In 2000, seven HIV-infected infants were born. Three of the mothers had received some prenatal care, including two women who knew their HIV status and had been prescribed combination ART. However, either the prescriptions were unfilled or the medications were taken irregularly; both women received ZDV during the intrapartum period. The third mother, who had prenatal care, was first tested for HIV 3 days before delivery; the positive test result was returned during labor, and she was started on intravenous ZDV. Of the four mothers without any prenatal care, one knew her HIV status before pregnancy. Two of the four mothers were cocaine users, one of whom had a negative HIV test during the fourth month of her pregnancy performed outside the prenatal care setting but had an HIV-positive test during the first postpartum day because of a positive drug screen. In six of the seven transmission cases in 2000, the infant was started on postpartum ZDV prophylaxis within 24 hours of birth. The remaining infant, whose mother first tested positive postpartum, was started on ZDV on the fourth day after birth. Reported by: S Nesheim, MD, S Henderson, MD, M Lindsay, MD, J Zuberi, MD, V Grimes, Grady Memorial Hospital, Atlanta; J Buehler, MD, Div of Public Health, Georgia Dept of Human Resources. ML Lindegren, MD, M Bulterys, MD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:GMH serves an economically disadvantaged population with high rates of illicit drug use. Since 1987, GMH has offered voluntary HIV testing to pregnant women receiving prenatal care or going into labor, and efforts at GMH to prevent perinatal HIV transmission have been successful in lowering transmission rates among HIV-infected pregnant women (6). However, the findings in this report underscore the challenges to universal prevention of perinatal HIV transmission. During 1997--2000, no cases of perinatal HIV transmission were identified among pregnant women who participated in the full program of prenatal care, HIV testing in pregnancy, and ART. Of the seven cases among women with perinatal transmission in 2000, at least four might have been prevented by using the full regimen of ART. Two of the four women received prenatal care and were aware of their HIV infections, one received prenatal care and was unaware of her infection, and one did not receive prenatal care but was aware of her infection. In 2001, the Georgia Division of Public Health initiated a program focused on further reducing perinatal HIV transmission among women living in Atlanta. Through collaborations with hospital staff and local county health departments, HIV-infected pregnant women are linked to community resources to support and facilitate their adherence to appropriate therapy and other prevention services. Certain perinatal HIV infections might be attributed to inadequate prenatal care. However, HIV testing of pregnant women even as late as the time of labor allowed nearly all HIV-exposed infants to receive the recommended neonatal ZDV postexposure prophylaxis for 6 weeks, demonstrating the value of HIV testing during labor. In 2001, the U.S. Department of Health and Human Services revised its guidelines for routine, voluntary HIV testing of pregnant women (7), including rapid HIV testing at the time of labor for women whose HIV status is unknown. CDC is continuing to promote these recommendations as part of a new initiative aimed at reducing barriers to early diagnosis of HIV infection and increasing access to medical care and ongoing prevention services (8). Perinatal HIV transmission can be prevented (3--5); the perinatal HIV infections described in this report highlight missed opportunities for perinatal HIV prevention and the need for multiple prevention strategies to reach women at high risk for infection. Innovative approaches must be developed that address the needs of mothers who receive little or no prenatal care or who have not had HIV testing before labor (3). Routine prenatal HIV testing of all pregnant women affords the best opportunity for the prevention of perinatal HIV transmission (9). Repeat HIV testing during the third trimester of pregnancy (10) probably would have identified the risk status of two of the infants described in this report and resulted in appropriate peripartum antiretroviral prophylaxis. Resident treatment programs for cocaine-addicted pregnant women, together with supervised antiretroviral therapy, if indicated, for homeless and addicted mothers late in pregnancy, might further prevent perinatal HIV infection. For pregnant women who receive prenatal care and know their HIV status, prevention programs should focus on promoting adherence to recommended treatment regimens and administering ART during pregnancy (4,5). Efforts to reduce perinatal HIV transmission should continue to focus on increasing prenatal care rates and prenatal HIV testing, particularly in areas where missed opportunities for prevention of perinatal HIV transmission persist. References
Table 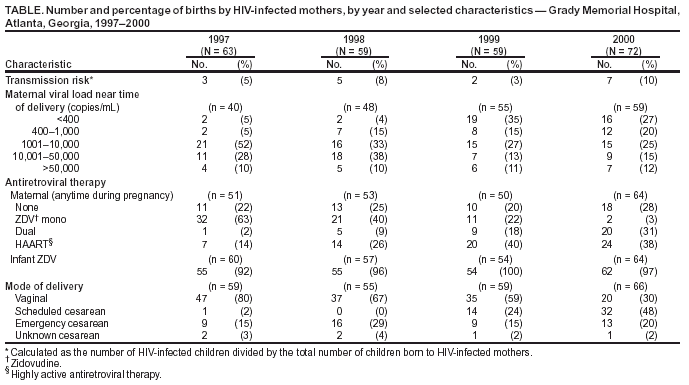 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 12/30/2003 |
|||||||||
This page last reviewed 12/30/2003
|