 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Correctable Visual Impairment Among Persons with Diabetes --- United States, 1999--2004Persons with diabetes are more likely to be visually impaired than persons without the disease (1). In 2005, CDC estimated that 14.6 million persons in the United States had diagnosed diabetes and an additional 6.2 million had undiagnosed diabetes (2). Despite the importance of detecting and treating vision problems caused by refractive errors (i.e., correctable visual impairment [CVI]), a limited number of studies have attempted to determine the proportion of persons with diabetes whose poor vision could be corrected with accurately prescribed glasses or contact lenses. To estimate that proportion, CDC analyzed 1999--2004 data from the National Health and Nutrition Examination Survey (NHANES). This report describes the results of that analysis, which indicated that among U.S. adults aged >20 years with diabetes,* 11.0% had visual impairment (i.e., presenting visual acuity worse than 20/40 in their better-seeing eye while wearing glasses or contact lenses, if applicable) and approximately 65.5% of these cases of visual impairment were correctable. Health-care providers and persons with diabetes should be more aware that poor vision often is correctable and that visual corrections can reduce the risk for injury and improve the quality of life for persons with diabetes. NHANES is an ongoing series of cross-sectional surveys on health and nutrition designed to be nationally representative of the noninstitutionalized, U.S. civilian population by using a complex, multistage probability design. All NHANES surveys include a household interview followed by a detailed physical examination. For the 1999--2000, 2001--2002, and 2003--2004 surveys, participants also were asked questions regarding vision function, and the physical examination included a vision examination in which visual acuity was measured before and after an objective autorefraction test (optical correction measured by an autorefractor). In this study, visual acuity before correction was defined as distance visual acuity with whatever form of current correction (e.g., glasses or contact lenses) the participant might have worn at the time of examination. Visual acuity after correction was defined as potential visual acuity as assessed by an objective autorefraction test. Only those participants whose visual acuity before correction was worse than 20/30 were administered the autorefraction test. Diabetes was defined as a self-reported previous diagnosis of the disease. In the NHANES surveys conducted during 1999--2004, the combined household interview response rate was approximately 82%, and the medical examination response rate was 77%. Of 15,332 adults aged >20 years, 22 were excluded because of lack of diabetes information or because their diabetes was diagnosed only during pregnancy. Another 2,306 adults for whom visual acuity before correction values were missing were excluded from the study. For this analysis, 1,237 adults aged >20 years with self-reported diabetes were divided into three groups according to their visual acuity in the better-seeing eye (before and after optical correction): 1) normal: visual acuity of 20/40 or better; 2) mild impairment: visual acuity better than 20/200 and worse than 20/40; and 3) severe impairment: visual acuity of 20/200 or worse. The prevalence of CVI was defined as the proportion of adults with mild or severe impairment before correction who were found to have the potential for normal visual acuity after correction. All analyses were weighted to make estimates representative of the U.S. civilian, noninstitutionalized population. Results also were analyzed by age group (20--64 years compared with >65 years), sex, and race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other). Overall, the prevalence of CVI among U.S. adults aged >20 years with diabetes was 7.2%, which indicated that the proper prescription for glasses or contact lenses would have restored normal visual acuity to 65.5% of visually impaired adults with diabetes (Table). The results indicated that 9.7% (95% CI [confidence interval] = 7.9%--11.8%) of U.S. adults with diabetes had mild visual impairment, and 1.4% (CI = 1.0%--1.9%) had severe visual impairment before correction; 2.9% (CI = 2.1%--3.9%) had mild impairment, and 1.0% (CI = 0.6%--1.5%) had severe impairment after correction. Approximately 0.3% of adults with diabetes who had severe visual impairment before correction had only mild visual impairment after correction. Thus, optical correction would have restored normal visual acuity to approximately 73.4% of adults with mild impairment and 9.1% of adults with severe impairment. Although the crude prevalence of CVI among adults aged >65 years with diabetes (7.3%) was similar to that among those aged 20--64 years (7.2%), 89.2% of visual impairment cases among the younger age group were correctable, compared with 46.4% of cases among the older age group. The age-adjusted prevalence of CVI was similar among men (7.3%) and women (7.2%). Although not statistically significant, the age-adjusted prevalence of CVI was higher among non-Hispanic blacks (7.9%) and Mexican Americans (8.1%) than among non-Hispanic whites (5.6%). Reported by: X Zhang, MD, PhD, EW Gregg, PhD, YJ Cheng, MD, PhD, T Thompson, MS, LS Geiss, MS, MR Duenas, OD, JB Saaddine, MD, MPH, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:This report describes the first nationally representative study to estimate the proportion of U.S. adults with diabetes who have visual impairment that can be corrected. The findings indicate that nearly two-thirds of adults with diabetes who have visual impairment can correct their vision with an accurate corrective prescription for glasses or contact lenses. This finding underscores the importance of public awareness and public health intervention in reducing the prevalence of CVI, especially among persons with diabetes. However, although simple eye examinations and the provision of prescription glasses or contact lenses can correct or improve most cases of visual impairment caused by refractive errors, persons with diabetes also can have ocular complications such as diabetic retinopathy, which is the leading cause of legal blindness in the United States. Persons with diabetes are recommended to have yearly dilated eye examinations or fundus photography to ensure early detection and timely treatment of the ocular complications of diabetes. CVI has been documented in several population-based studies (3--6) and has been determined to be related to reduced quality of life and increased mortality (7--9). One study reported that approximately 50% of participants had improved vision after refractive correction (6). Another study found that uncorrected refractive error accounted for nearly 73% of the cases of impaired visual acuity among Mexican Americans aged >40 years (5), and similar findings were reported among residents in the United Kingdom (7) and Australia (10). Moreover, on the basis of NHANES data from 1999--2002, the National Eye Institute reported the first nationally representative estimates of the prevalence of CVI in the general population (5.3%) and emphasized the importance of correcting visual impairments caused by refractive error as a means of improving safety (e.g., by reducing the risk for unintentional injuries, particularly falls) and quality of life for those affected by such impairments (1). The findings in this report are subject to at least five limitations. First, because institutionalized persons (e.g., nursing home residents) are excluded from NHANES participation, the overall prevalence of visual impairment among U.S. adults with diabetes likely was underestimated. Second, the exclusion of potential study participants who were completely blind, were unable to see in both eyes, or had a severe infection in one or both eyes might have resulted in lower prevalence estimates of visual impairment. Third, because this study measured only objective refraction and performed no subjective refinement of objective refraction measurements, estimates of visual acuity after correction might not reflect the best corrected vision that participants might attain, resulting in an underestimate of CVI prevalence. Fourth, although visual acuity of survey participants was measured with whatever glasses or contact lenses they wore at the time of examination, certain participants might not have had their current corrective devices at that time, a factor that might have led to an overestimate of CVI prevalence. Finally, certain estimates had a relative standard error of >30% and thus are considered statistically unreliable. CDC collaborates with the National Eye Institute through the National Eye Health Education Program to increase public and professional awareness of the importance of routine eye examinations. CDC also provides resources and technical assistance to states and nonprofit organizations (e.g., Prevent Blindness America) to help them increase their surveillance of vision loss and eye diseases, increase public awareness of how to prevent vision loss, and generally promote eye health to reduce the public burden of visual impairment. The findings of this study underscore a continued need for national visual acuity data from representative U.S. population surveys. These data are essential to the planning, implementation, and evaluation of public health practices designed to reduce the burden of visual impairment among persons with diabetes in the United States. The high prevalence of CVI among persons with diabetes indicates a need for enhanced vision-related public health interventions (e.g., vision screening) among adults with diabetes. The findings of this study also suggest that the use of visual acuity and refractive error assessments in concert with recommended dilated eye examinations might further contribute to improved vision outcomes for adults with diabetes. Identifying and pursuing ways of increasing access to eye care and ensuring that those with CVI receive appropriate vision correction will help reduce the morbidity and mortality among persons with diabetes associated with impaired vision and help persons achieve optimal vision and eye health. Acknowledgments This report is based, in part, on contributions by KM Venkat Narayan, MD, and J Wang, MD, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. References
* Excludes persons with diabetes who were completely blind, unable to see in both eyes, or with a severe infection in one or both eyes.
Table 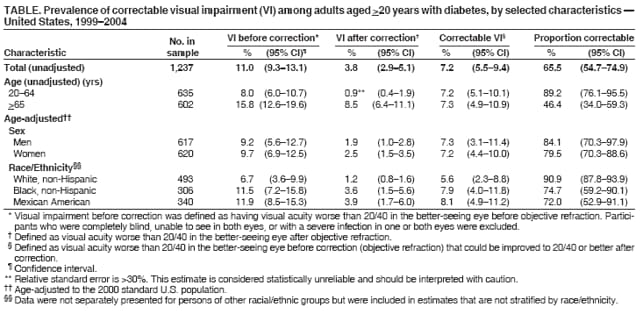 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 11/1/2006 |
|||||||||
|