 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Nutritional and Health Status of Children During a Food Crisis --- Niger, September 17--October 14, 2005Media attention in 2005 brought worldwide awareness to a food and nutrition crisis in the West Africa country of Niger (population 11.5 million in 2002). The United Nations World Food Programme estimated that 2.5 million persons living in farming and grazing areas in Niger were vulnerable to food insecurity (i.e., not having access at all times to enough food for an active, healthy lifestyle) (1). Local surveys conducted in the Maradi and Tahoua administrative regions during April 2005 suggested critical levels (i.e., >15%) of global acute malnutrition (GAM) and greater mortality among Niger's estimated 2.7 million children aged <5 years than the emergency threshold (i.e., more than two deaths per 10,000 children per day) (2). To help ensure a proportionate and timely response, the Government of Niger and the United Nations Children's Fund (UNICEF) collaborated with CDC to conduct an emergency survey that assessed the magnitude of malnutrition and recent illness among young children in Niger. This report summarizes the results of that survey, which determined that, among children aged 6--59 months, 15.3% had GAM; during the preceding 2 weeks, 72.0% had fever, and 49.1% had diarrhea. Among children aged 9--59 months, 33.7% had not been vaccinated for measles. Health officials in Niger took immediate action to improve availability of food, increase accessibility to medical treatment (for fever, diarrhea, and respiratory illness), and administer measles vaccinations along with vitamin A supplements to children who had not been vaccinated. The survey used a two-stage sampling methodology in each of Niger's eight administrative regions (i.e., consisting of seven departments [Agadez, Diffa, Dosso, Maradi, Tahoua, Tillaberi, and Zinder] and the capital district of Niamey). A statistically valid sample size was calculated using data from nutrition surveys conducted previously in Niger (3). Data from the Niger 2001 census were used as the population sampling frame; these data excluded the country's nomadic population (estimated at 5% of the overall population) (4). In the first stage of sampling, 26 clusters (i.e., villages) were selected for each of the eight regions using probability proportional to population size, yielding a total of 208 clusters nationally. In the second stage, a systematic random sampling method was used to select 20 households per cluster; however, the number of children in the sample for each region varied depending upon the response rate from the 4,160 households and the number of children in each household. A household was defined as a group of persons who usually lived together in the same housing unit, ate food prepared in the same cooking pot, and agreed that the same person was head of the household (3). A standardized nutrition questionnaire (3) used for the survey was adapted to reflect cultural concerns and was translated and back-translated into French, Djerma, and Hausa. After granting informed consent, the mother or caretaker of children aged 6--59 months in each household responded to questions regarding illnesses (i.e., diarrhea, cough with difficulty breathing, or fever) during the preceding 2 weeks among the children. Children aged 9--59 months were checked for evidence of measles vaccination (with or without a vaccination card), and mothers were asked whether their children aged 6--59 months had received vitamin A supplementation. To determine the prevalence of malnutrition, all eligible children aged 6--59 months in each household were weighed, measured, and assessed for bilateral pedal edema. Height or recumbent length was measured to the nearest 1 mm using a standard height board; weight was measured using an electronic digital scale to the nearest 100 g. GAM was defined as a weight-for-height z-score <-2.0 standard deviations from the median of the CDC/World Health Organization reference population (5), or edema. Severe acute malnutrition (SAM) was defined as a weight-for-height z-score <-3.0 standard deviations from the median of the reference population, or edema. Total chronic malnutrition (i.e., stunted growth) was defined as a height-for-age z-score <-2.0 standard deviations from the median of the reference population, and severe chronic malnutrition was defined as a height-for-age z-score <-3.0 standard deviations from the median of the reference population (6). The nutrition analyses excluded children whose age, weight, or height were not recorded or whose z-scores were identified as extreme values. Statistical software was used to take into account the complex sample design and unequal probabilities of selection. Information was collected from 4,003 of 4,160 households, for an overall response rate of 95.6%. Overall, health information was gathered on 5,309 children aged <59 months. Anthropometry measurements were valid for 4,501 of 4,714 children aged 6--59 months. Forty-three percent of these children were aged 6--35 months, and 57% were aged 36--59 months; 51% were male. Among these children, the prevalences of GAM as defined by their weight-for-height z-scores exceeded those of the reference population by approximately sevenfold (Figure). The prevalence of GAM ranged from 9.0% in Niamey to 17.9% in Tahoua. The regions with the highest levels of SAM were Maradi and Tillaberi (2.3% and 2.0%, respectively) (Table 1). The prevalence of GAM among children aged 6--35 months (22.4%) was approximately four times greater (relative risk = 3.7; 95% confidence interval [CI] = 3.0--4.6) than among children aged 36--59 months (6.1%). In addition, 70% of the children aged 6--35 months who had GAM also had chronic malnutrition. Overall in Niger, 50.0% of children aged 6--59 months had chronic malnutrition. The prevalence of chronic malnutrition was greater among children aged 6--35 months (54.9%) than among children aged 36--59 months (43.5%) (Table 1). The national estimate for children aged 6--59 months with a history of fever during the 2 weeks preceding the survey was 72.0% (Table 2). The cumulative incidence of diarrhea during the preceding 2 weeks ranged from 22.9% in Niamey to 59.8% in Maradi. The national cumulative incidence of cough with difficulty breathing (i.e., symptoms suggestive of a respiratory infection) during the preceding 2 weeks was 39.0%. Overall, measles vaccination coverage among children aged 9--59 months was 66.3%, ranging from 58.1% in Zinder to 87.4% in Niamey (Table 2). Vitamin A supplement distribution among children aged 6--59 months was 73.7% (CI = 70.9--76.4), ranging from 48.9% (CI = 40.6--57.2) in Diffa to 89.3% in Tillaberi (CI = 82.2--93.8) Reported by: V Aguayo, PhD, UNICEF Regional Office for West and Central Africa, Dakar, Senegal. N Zagre, PhD, UNICEF Niger, Niamey; K Koumbe, MD, Niger Ministry of Health. B Tomczyk, DrPH, C Blanton, MS, Div of Emergency and Environmental Health Svcs, National Center for Environmental Health; A Reza, MD, EIS Officer, CDC. Editorial Note:Niger is one of the poorest countries in the world and is known for recurring droughts resulting in food production deficits that place the country at risk for famine. The United Nations Agencies and Programmes and the U.S. Agency for International Development closely monitor food security concerns such as meteorologic, crop, and grazing land conditions to provide early warnings on an ongoing basis. Emergency nutrition surveys can provide critical information regarding children aged <5 years, the population most sensitive to acute nutritional stress; the results of these assessments serve as indicators for the nutritional status of the whole population. Together, data on food insecurity and nutritional status provide an overall assessment of the scale of the crisis and required response (7). The findings from the emergency survey described in this report indicate that Niger had an acute nutrition crisis during September--October 2005 that affected children in all eight administrative regions to varying degrees. Gathering regional data on malnutrition enabled officials to gauge the breadth of the problem to determine how to target their response. Children with acute malnutrition are more susceptible to disease and have greater risk for dying when they become ill (7); chronic malnutrition can affect cognitive and social development. In four regions (Diffa, Maradi, Tahoua, and Zinder) the situation was critical (prevalence of GAM >15%), requiring immediate humanitarian action to prevent an increase in child morbidity and mortality. The four regions where the situation was defined as critical represent 60% of the total population in Niger. In addition, chronic malnutrition was pervasive in all regions, affecting 50% of children aged 6--59 months overall. The high prevalence of chronic malnutrition suggests a longstanding problem of poor nutrition and health among children. The findings from this survey also estimated prevalences of recent childhood illnesses. Prevalences of fever and diarrhea were high among children in regions with critical and serious levels of GAM. All regions indicated measles vaccination rates below the 90%--100% level needed to prevent an outbreak (8), even though a measles campaign had reported coverage of 90% among children aged 6 months--14 years, 8 months before the survey (9). This discrepancy might be the result of recall bias, inaccurate estimates of measles coverage, or both. Measles vaccination and use of vitamin A supplements, bed nets, antimalarial drugs, and oral rehydration salts are some of the methods used to prevent and decrease the incidence of childhood illnesses, but access to and availability of these resources are limited in Niger (9). These health resources should be included when planning solutions to decrease acute malnutrition among children. The findings in this report are subject to at least three limitations. First, the actual GAM level might have been higher than estimated, because the data collection coincided with the harvest, when food was more abundant. Second, food distributed by relief programs might have improved the nutritional status of some children and obscured the extent of the food crisis. Finally, estimates of recent illness came from reports made by the mothers or caretakers of children and were not confirmed by medical records. As a result of the survey findings, health officials in Niger took immediate action to 1) restore the general food supply by distributing food commodities in all regions with GAM >15% (i.e., Diffa, Maradi, Tahoua, and Zinder); 2) implement supplementary feeding programs for all children in those same four regions until improvement occurred in general food availability and accessibility; 3) improve availability and accessibility of oral rehydration salts for treatment of diarrhea; and 4) vaccinate all children aged 9 months--15 years for measles to maintain coverage greater than 90% and distribute vitamin A supplements to them. Further analyses of the direct and indirect causes of malnutrition are needed to target interventions that will improve the health and nutritional status of children in Niger. References
Table 1 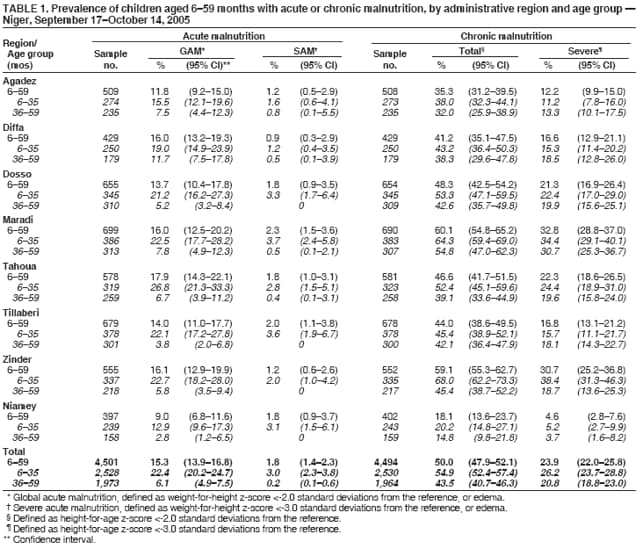 Return to top. Table 2 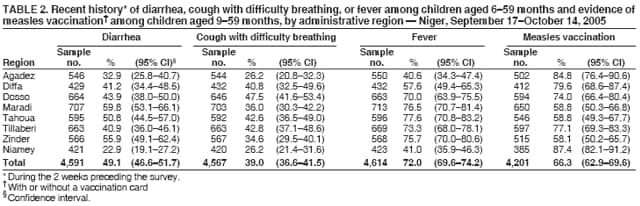 Return to top. Figure 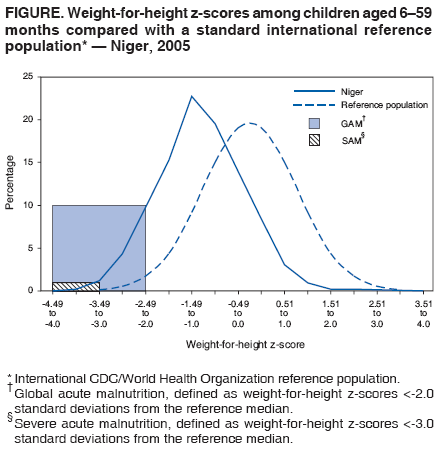 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 11/1/2006 |
|||||||||
|