 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Increase in Coccidioidomycosis --- California, 2000--2007Coccidioidomycosis is an infection resulting from inhalation of airborne spores of Coccidioides immitis or Coccidioides posadasii, soil-dwelling fungi endemic to California's San Joaquin Valley; southern regions of Arizona, Utah, Nevada, and New Mexico; western Texas; and regions of Mexico and Central and South America (1). Of an estimated 150,000 new infections annually in the United States (2), approximately 60% are asymptomatic (1). Patients with symptoms usually experience a self-limited influenza-like illness (ILI), although some develop severe pneumonia. Fewer than 1% of patients develop disseminated disease. Infection usually produces immunity to reinfection. During 1995--2000, the number of reported coccidioidomycosis cases in California averaged 2.5 per 100,000 population annually. However, from 2000 to 2006, the incidence rate more than tripled, increasing from 2.4 to 8.0 per 100,000 population. To characterize this increase, the California Department of Public Health (CDPH) analyzed case and hospitalization data for the period 2000--2007 and preliminary case report data for 2008. The results indicated that, during 2000--2006, the number of reported cases and hospitalizations for coccidioidomycosis in California increased each year, before decreasing in 2007. Annual incidence during 2000--2007 was highest in Kern County (150.0 cases per 100,000 population), and the hospitalization rate was highest among non-Hispanic blacks, increasing from 3.0 to 7.5 per 100,000 population. Health-care providers should maintain heightened suspicion for coccidioidomycosis in patients who live or have traveled in areas where the disease is endemic and who have signs of ILI, pneumonia, or disseminated infection. Coccidioidomycosis is a reportable disease in California, although laboratories are not required to report. During 1991--1995, California experienced a large epidemic of coccidioidomycosis in the San Joaquin Valley; since 1995, cases of coccidioidomycosis have been reported consistently to local health departments in California using Confidential Morbidity Reports (CMRs). For the analysis summarized in this report, CDPH reviewed case and hospitalization data for the period 2000--2007 using CMRs and California Patient Discharge Data Set (CPDDS) data. Preliminary CMR case data for 2008 also were analyzed. CMRs include data on the patient's county of residence, sex, and dates of birth, illness onset, diagnosis, and case report. CPDDS data include inpatient discharge diagnoses from all California nonfederal hospitals. Cases with codes for coccidioidomycosis (114--114.5 and 114.9) from the International Classification of Diseases, Ninth Edition were selected. Duplicate records were removed so that the CMR data set retained only the first report of a case and the CPDDS retained only the first report of a patient's hospitalization. For the 3% of reported CMR cases with no date of illness onset or diagnosis, year of illness onset was presumed to be year of case report. CMR data were used to calculate incidence rates of reported cases overall and by age, sex, region, and county. Because 34% of reported CMR cases had missing data on race, incidence rates by race were not calculated. CPDDS data were used to calculate rates of first hospitalization overall and by age, sex, race/ethnicity, region, and county. California Department of Finance population projections were used for denominators (3). Negative binomial regression was used to test for statistical significance of change in rates of reported cases and hospitalizations during 2000--2006, the period of annual increase in reported cases and hospitalizations. Fatality rates among hospitalized patients were calculated by using CPDDS data for 2000--2007. After remaining stable since 1995, reported coccidioidomycosis cases in California increased from 816 in 2000 (incidence rate: 2.4 per 100,000 population) to 2,981 in 2006 (8.0 per 100,000 population) (p<0.001) (Figure 1), before decreasing in 2007 to 2,791 cases (7.4 per 100,000 population). Preliminary 2008 CMR data indicated that 1,718 cases were reported in California during January 1--December 6, 2008, compared with 2,210 and 2,426 cases reported during the same period in 2006 and 2007, respectively. During 2000--2007, estimated average annual incidence was highest among adults aged 40--49 years (3,518 cases [8.0 per 100,000 population]) versus other age groups (Table). A total of 10,909 (65%) cases were reported in male patients, for an average annual rate of 7.6 per 100,000 population, compared with 5,848 cases in females (4.0 per 100,000 population) (Table). The greatest incidence occurred in the San Joaquin Valley region, where coccidioidomycosis is endemic. A total of 12,855 (76%) of California's 16,970 cases were reported from the San Joaquin Valley during 2000--2007. Reported cases from this region increased from 490 (14.7 per 100,000 population) in 2000 to 2,135 (53.9 per 100,000 population) in 2007. Within the region, Kern County reported the highest incidence every year. Rates of reported cases in Kern County averaged 150.0 per 100,000 population during 2000--2007 (Figure 2), peaking in 2004 at 195.3 per 100,000 population. In California, coccidioidomycosis cases requiring hospitalization increased from 611 in 2000 (1.8 per 100,000 population) to 1,587 in 2006 (4.3 per 100,000 population) (p<0.001), before decreasing to 1,368 (3.6 per 100,000 population) in 2007 (Figure 1). Hospitalizations for coccidioidomycosis were highest among persons aged 60--79 years, averaging 5.8 per 100,000 population during 2000--2007 (Table). By race/ethnicity, hospitalizations were highest among non-Hispanic blacks, compared with non-Hispanic whites, Hispanics, and Asians/Pacific Islanders. From 2000 to 2007, hospitalizations among non-Hispanic blacks increased from 66 (3.0 per 100,000 population) to 169 (7.5 per 100,000 population). Hospitalizations among non-Hispanic whites increased from 297 (1.9 per 100,000 population) in 2000 to 570 (3.5 per 100,000 population) in 2007; hospitalizations among Hispanics increased from 182 (1.6 per 100,000 population) to 485 (3.6 per 100,000 population), and hospitalizations among Asians/Pacific Islanders increased from 36 (0.9 per 100,000 population) to 86 (1.9 per 100,000 population). By geographic region, hospitalizations for coccidioidomycosis in the San Joaquin Valley increased from 230 (6.9 per 100,000 population) in 2000 to 701 (17.7 per 100,000 population) in 2007. Within the region, Kern County reported the highest hospitalization rates, increasing from 121 (18.2 per 100,000 population) in 2000 to 285 (34.9 per 100,000 population) in 2007, and peaking in 2005 at 353 hospitalizations (45.8 per 100,000 population). Overall in California, during 2000--2007, a total of 752 (8.7%) of the 8,657 persons hospitalized for coccidioidomycosis died. Reported by: DJ Vugia, MD, C Wheeler, MD, KC Cummings, MPH, California Dept of Public Health. A Karon, DVM, EIS Officer, CDC. Editorial Note:This report describes increases in reported coccidioidomycosis cases and hospitalizations during 2000--2007 and the highest incidence rate in California since 1995, the first year that CMR data were available consistently. The number of reported cases and hospitalizations decreased in 2007, and preliminary data indicate those decreases might have continued in 2008. However, rates of coccidioidomycosis in California remain substantially higher than during 1995--2000. These increased rates likely are real, rather than surveillance artifact, because no major changes in diagnosis or reporting of coccidioidomycosis in California occurred before or during the period studied. Increases in coccidioidomycosis in California are similar to those observed in neighboring Arizona and in the United States overall. Arizona, which annually reports approximately 60% of all coccidioidomycosis cases in the United States, reported a substantial increase in coccidioidomycosis from 1,812 cases (37 per 100,000 population) in 1999 to 5,535 cases (91 per 100,000 population) in 2006 (4). In the United States overall, the number of reported coccidioidomycosis cases increased from 1,697 (0.64 per 100,000 population) in 1996 to 8,917 (6.79 per 100,000 population in 2006) (5). Reasons for these recent increases in reported coccidioidomycosis are not fully understood. Some previous increases have been associated with local environmental and climatic variations (6). Other hypothesized causes include aerosolization of spores caused by soil disturbance during periods of increased construction activity (4), growing numbers of persons who are immunocompromised or have other risk factors for severe disease (7), and immigration of previously unexposed persons from areas where coccidioidomycosis is not endemic (2). Recent increases in coccidioidomycosis in California are partially attributable to several hundred cases reported from two San Joaquin Valley prisons (8) with inmates from areas where the disease is not endemic. Multiple clusters also have been reported at California military bases, where personnel often have intensive dust exposure (9). Such exposure is hypothesized to increase the risk for infection; local outbreaks of coccidioidomycosis have been noted after dust storms (1). Coccidioidomycosis hospitalization rates in California were highest among persons aged 60--79 years, which is consistent with previous reports that older age might be a risk factor for severe coccidioidomycosis (7). Hospitalization rates also were substantially higher among non-Hispanic blacks, compared with non-Hispanic whites, Hispanics, and Asians/Pacific Islanders. Black race has been associated previously with increased risk for coccidioidomycosis hospitalization (7). In addition, blacks and persons of Filipino ancestry have been found to have increased risk for disseminated coccidioidomycosis, possibly because of underlying differences in susceptible host genetics (1,10). Immunocompromised persons and women in their second and third trimesters of pregnancy also have increased risk for disseminated disease (1). The findings in this report are subject to at least three limitations. First, because not all persons with coccidioidomycosis seek medical care and not all diagnosed cases are reported to local health departments, this report likely underestimates the actual rate of coccidioidomycosis in California. Second, for cases in which patients were hospitalized, medical chart review was not performed to confirm laboratory diagnosis or cause of death from coccidioidomycosis, resulting in possible overestimation of hospitalizations and deaths in persons with coccidioidomycosis diagnosed. Finally, Kern County's public health laboratory performs much of the coccidioidomycosis testing for patients in that county and might be more likely to report cases routinely than laboratories in most other counties in the San Joaquin Valley region where this is not the practice. In 2009, California plans to make coccidioidomycosis a laboratory-reportable disease to improve completeness and timeliness of case reporting and delivery of targeted public health recommendations during periods of increased disease. Given the recent increases in coccidioidomycosis in California and Arizona, heightened consideration of this disease is warranted in the differential diagnosis of any patient with ILI, pneumonia, or signs of disseminated infection who has lived or traveled in areas where coccidioidomycosis is endemic. Because intensive dust exposure appears to increase the risk for infection, CDC recommends that persons living or traveling in regions where coccidioidomycosis is endemic who are at risk for severe or disseminated disease (e.g., older persons, pregnant women, immunocompromised persons, and persons of black race or Filipino ancestry) should avoid exposure to outdoor dust as much as possible.* When such exposure is unavoidable, measures to reduce inhalation of outdoor dust, such as wetting soil and using respiratory protection when engaging in soil-disturbing activities, might be effective. However, options for environmental control of coccidioidomycosis are limited, and no safe, effective vaccine for the disease exists currently. Developing such a vaccine appears to be the best option for preventing disease in those persons at risk for coccidioidomycosis (9). Acknowledgments The findings in this report are based, in part, on contributions by SR Bissell, MS, California Department of Health; and EC Weiss, MD, Office of Workforce and Career Development, CDC. References
* Additional information available at http://wwwn.cdc.gov/travel/yellowbookch4-coccidioidomycosis.aspx. Figure 1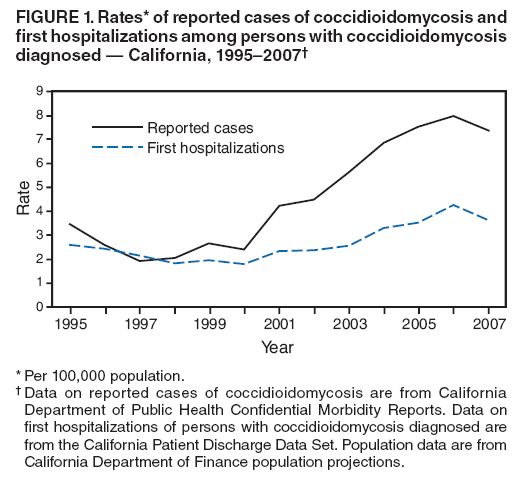 Return to top. Figure 2 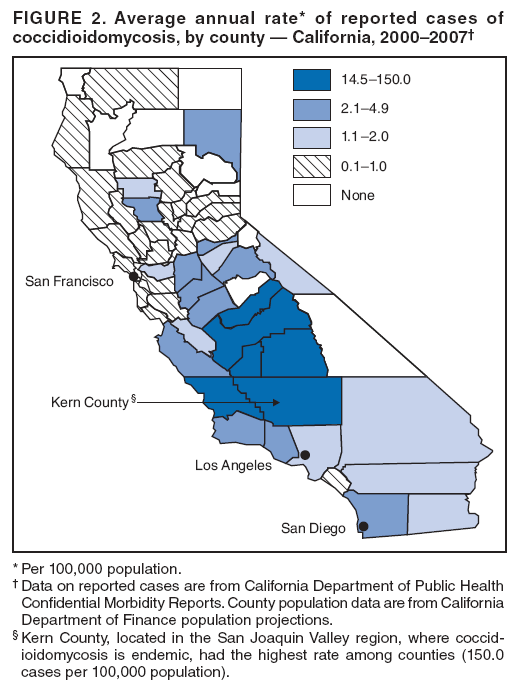 Return to top. Table 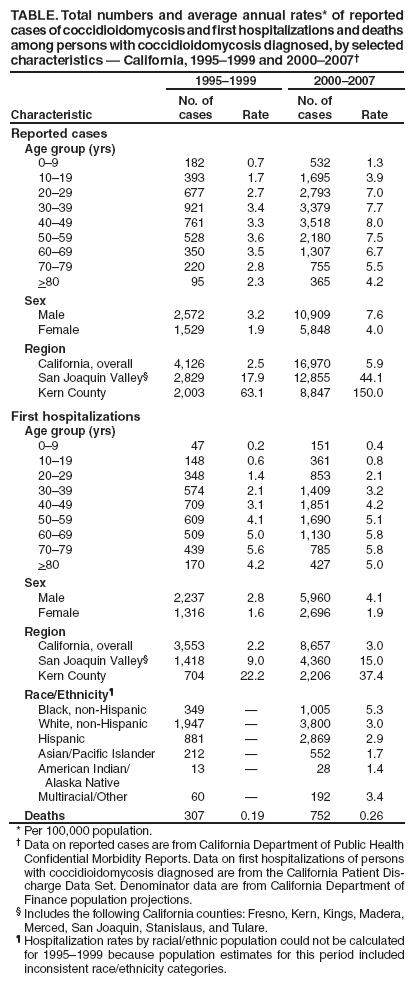 Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 2/12/2009 |
|||||||||
|