 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Completeness and Timeliness of Reporting of Meningococcal Disease --- Maine, 2001--2006Neisseria meningitidis is an important cause of invasive bacterial disease in the United States (1), with a total of 1,077 cases of meningococcal disease reported in 2007 (2). The case-fatality ratio is 10%--14%, and 11%--19% of survivors have long-term sequelae (1). In the United States, approximately 98% of cases of meningococcal disease occur sporadically; outbreaks are uncommon (1). Chemoprophylaxis is the primary means of preventing meningococcal disease among close contacts of patients in sporadic cases (1), and the ability of health departments to identify these contacts and provide treatment depends on the completeness and timeliness of disease reporting. To assess these attributes in meningococcal disease surveillance in Maine, the Maine Department of Health and Human Services (MDHHS) analyzed public health surveillance data from MDHHS and hospital discharge data from the Maine Health Data Organization (MHDO) for the period 2001--2006. This report describes the results of that analysis, which indicated that the completeness of reporting of meningococcal disease in Maine during this period was approximately 98%. Of cases reported to MDHHS, 56% were reported within 1 day of hospital admission. Passive disease surveillance efforts appear to have achieved near complete reporting of meningococcal disease in Maine; however, timeliness of reporting was sometimes suboptimal. Evaluation of surveillance efforts should be repeated periodically to determine whether completeness of reporting remains high and timeliness improves. Maine law requires that all health-care providers, laboratories, and health-care facilities report meningococcal disease (upon recognition or strong suspicion) immediately by telephone to MDHHS. Reports are assigned to epidemiologists for investigation. Reports meeting the Council of State and Territorial Epidemiologists (CSTE) and CDC case definition for meningococcal disease* are entered in the National Electronic Disease Surveillance System.† Beginning in 2006, the CSTE-CDC case definition was revised to include suspected cases of meningococcal disease; in previous years, the case definition only included categories for confirmed and probable cases. MHDO maintains the state's hospital discharge dataset, which includes inpatient and outpatient visits for all nonfederal, acute-care hospitals in the state. International Classification of Diseases, 9th Revision (ICD-9) codes 036.0--036.9 (for meningococcal disease) were used to identify patients with meningococcal disease. The dataset did not contain patient names, so MHDO data were matched with MDHHS data for the period 2001--2006 using date of birth, admission date, and hospital. Persons who were in both datasets were considered to have verified cases of meningococcal disease. Hospital records were reviewed for patients who were in the MHDO dataset but who had not been reported to MDHHS. The utility of various ICD-9 codes and clinical settings for identifying cases of meningococcal disease from the MHDO dataset was examined by calculating sensitivity and positive predictive value (PPV) (Table 1). The completeness of meningococcal disease reporting was estimated by the Sekar-Deming capture-recapture method (3)§ (Table 2). The capture-recapture method provides an estimate of the actual total number of cases (reported or unreported) and the completeness of disease reporting using data from two independent surveillance systems (3). This technique requires being able to identify cases found in both surveillance systems, cases found only by the first surveillance system, and cases found only by the second surveillance system (3). Cases that could not have been reported to both MDHHS and MHDO were excluded from the capture-recapture analysis. These cases included out-of-state residents hospitalized in Maine who would not have been included in MDHHS records and Maine residents hospitalized out of state or at a Veterans Health Administration (VHA) facility in the state who would not have been included in the MHDO dataset. Timeliness of reporting was assessed by determining the difference in days between hospital admission and notification to MDHHS. A total of 52 cases of meningococcal disease were reported to MDHHS during 2001--2006. These cases included two that occurred in Maine residents hospitalized out-of-state and one in a person hospitalized at a VHA facility in Maine. A total of 107 patients were identified in the MHDO dataset. A total of 42 patients were in both the MHDO and MDHHS datasets and were considered to have verified cases of meningococcal disease. Hospital records were reviewed for the 65 patients who were in the MHDO dataset but not in the MDHHS dataset. Nine (14%) of these patients were determined to have had meningococcal disease using the CSTE-CDC case definition; these included eight cases in out-of-state residents hospitalized in Maine. The remaining 56 patients in the MHDO dataset did not meet the CSTE-CDC case definition. Of these 56, 19 (34%) had meningeal signs but neither clinical purpura fulminans nor laboratory evidence of N. meningitides; 15 (27%) were coded incorrectly (e.g., with diagnoses other than meningococcal disease); 13 (23%) had noninvasive infections (e.g., a positive sputum culture for N. meningitides); and nine (16%) had medical records that were missing or incomplete. In the analysis of the utility of various ICD-9 codes for identifying cases of meningococcal disease using MHDO data, sensitivity (92%) and PPV (53%) were highest when a combination of code 036.0 (meningococcal meningitis) or 036.2 (meningococcemia) was used (Table 1). Other ICD-9 codes for meningococcal disease (036.1 and 036.3--036.9) had poor sensitivity and PPV. Inpatient data were more sensitive and had higher PPV than outpatient data. The completeness of reporting for meningococcal disease to MDHHS was estimated at 97.6% (95% confidence interval = 95.9%--99.3%) (Table 2), based on MDHHS receiving reports on 49.0 of 50.2 total cases. Information was sufficient to assess timeliness of reporting for 43 (83%) of 52 cases reported to MDHHS. Reports were received in a median of 1 day (range: 0--11 days); 35% of cases were reported to MDHHS on the day of hospital admission, 56% were reported within 1 day, and 79% were reported within 2 days. No secondary cases of meningococcal disease among close contacts of patients with meningococcal disease were reported in Maine during the study period. Reported by: V Rea, MPH, Maine Dept of Health and Human Svcs and Univ of Southern Maine. A Pelletier, MD, Coordinating Office for Terrorism Preparedness and Emergency Response, CDC. Editorial Note:Because of the severity of meningococcal disease symptoms, nearly all patients are treated in a hospital or emergency department setting. This results in a dataset (i.e., hospital discharge data) that can be compared with public health surveillance records to estimate the completeness of reporting to health departments using the capture-recapture technique (3). Most other nationally notifiable conditions either 1) do not result in routine hospitalization (e.g., salmonellosis) or 2) do not occur frequently enough at the state level (e.g., botulism) to allow use of the capture-recapture technique. Therefore, meningococcal disease provides an uncommon opportunity to assess completeness of reporting using hospital discharge data. Six other studies using the capture-recapture technique to compare health department data with hospital discharge data have described the completeness of meningococcal disease reporting. The results have ranged from 64% to 95%, with a median value of 94% (4--9). The only published study from the United States was conducted in New York State in 1991 and reported 93% completeness (4). Completeness of reporting for meningococcal disease likely is considerably higher than for most other notifiable conditions because of the severity of the illness and the availability of a widely accepted public health intervention. Although most cases of meningococcal disease were reported to MDHHS in a timely manner, 44% were reported more than 1 day after hospital admission. In the 1991 New York study, 34% of cases were reported more than 1 day after diagnosis (4). Timeliness of reporting is important for this disease because chemoprophylaxis of close contacts of an index patient is most effective when administered as soon as possible; ideally, chemoprophylaxis should be started within 24 hours after identification of the index case, but not later than 14 days after illness onset (1). During the attempt to identify cases of meningococcal disease in the MHDO dataset, certain diagnostic codes (i.e., 036.1 and 036.3--036.9) and outpatient data had poor sensitivity and PPV. Because each potential case required medical record review for confirmation, considerable effort was required to identify a small number of actual cases. For example, of 38 reports of meningococcal disease among outpatients in the hospital discharge dataset, only two (5%) cases were verified after reviewing medical records. The findings in this report are subject to at least two limitations. First, the two data systems used in this analysis might not have been completely independent because information from hospitals was included in both MHDO and MDHHS datasets. This type of dependence between data sources might result in an overestimate of the completeness of reporting (10). Second, some of the 19 patients in the MHDO dataset with meningeal signs, but neither clinical purpura fulminans nor laboratory evidence of N. meningitides, might have met the definition for a suspected case if such a category had existed before 2006. This might have affected the estimate for the completeness of reporting. Passive disease surveillance efforts appear to have been adequate for achieving near complete reporting of meningococcal disease in Maine; however, timeliness of reporting was sometimes suboptimal. Evaluation of this surveillance system should be repeated periodically to determine whether completeness of reporting remains high and timeliness improves. Other attributes of surveillance systems (e.g., simplicity, representativeness, and acceptability) also should be assessed in future evaluations. In Maine, a delay of approximately 18 months after the end of a calendar year occurs before hospital discharge data for that year become available. This delay limits usage of the data for public health surveillance. When hospital discharge data become available on a real-time basis in Maine, MDHHS will need to determine how best to use this information, given the apparent limitations of ICD-9 codes in the MHDO dataset for identifying cases of meningococcal disease. Acknowledgments The findings in this report are based, in part, on contributions by E Bartlett, Houlton Regional Hospital; T Beaulier-Fuller, Aroostook Medical Center; C Bouley, Mercy Hospital; S Dirrigl, Southern Maine Medical Center; D Dunton, H Elliot, D Fenn, and D McKenney, Eastern Maine Medical Center; P Hadley, Franklin Memorial Hospital; E King, Maine General Hospital; B MacPike, Maine Coast Memorial Hospital; D Peabody, St. Joseph Healthcare; C Reeder, York Hospital; P Rybak, Mercy Hospital; D Skalina, Central Maine Medical Center; D Theriault, St. Mary's Hospital; B Wagner, Maine Medical Center; S Whiting, Reddington-Fairview Hospital; P Carson, D Guppy, L LaRochelle, L Parker, and A Robbins, Maine Dept of Health and Human Svcs; and D Baughman and A Cohn, Div of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, CDC. References
* Case definition available at http://www.cdc.gov/ncphi/disss/nndss/casedef/case_definitions.htm. † Additional information available at http://www.cdc.gov/nedss. § Completeness of reporting was calculated as R / N, and the 95% confidence interval was calculated as R / N + 1.96 Var (N)1/2 where Var (N) = (R x S x N1 x N2) / C3. R = number of cases identified in MDHHS dataset, N = estimated total number of cases of meningococcal disease in Maine during 2001--2006 calculated as C + N1 + N2 + X where X = (N1 x N2) / C, S = number of cases identified in MHDO dataset, N1 = number of cases identified only in MDHHS dataset, N2 = number of cases identified only in MHDO data, and C = number of cases identified in both MDHHS and MHDO datasets. Table 1 ![TABLE 1. Sensitivity and positive predictive value of hospital discharge data to identify meningococcal disease, by diagnostic code and clinical setting — Maine, 2001–2006
Cases*
Noncases
Sensitivity (%)†
Positive
predictive value (%)§
ICD-9¶ code
036.0 (meningococcal meningitis)
19
31
37
38
036.2 (meningococcemia)
28
11
55
72
036.0 or 036.2
47
42
92
53
036.1 or 036.3–036.9
4
14
8
22
Clinical setting
Inpatient
49
20
96
71
Outpatient
2
36
4
5
Total
51
56
100
48
* Meeting the Council of State and Territorial Epidemiologists and CDC case definition for meningococcal
disease, available at http://www.cdc.gov/ncphi/disss/nndss/casedef/case_definitions.htm. Cases included persons with meningococcal disease in both Maine Health Data Organization (MHDO) and Maine Department of Health and Human Services datasets (n = 42) and those reported only to MHDO (n = 9). Eight persons who were reported only to MHDO were out-of-state residents hospitalized in Maine.
† Calculated as follows: [(cases) / 51] x 100%.
§ Calculated as follows: [(cases) / (cases + noncases)] x 100%.
¶ International Classification of Diseases, 9th Revision.](figures/m807a3t1.gif) Return to top. Table 2 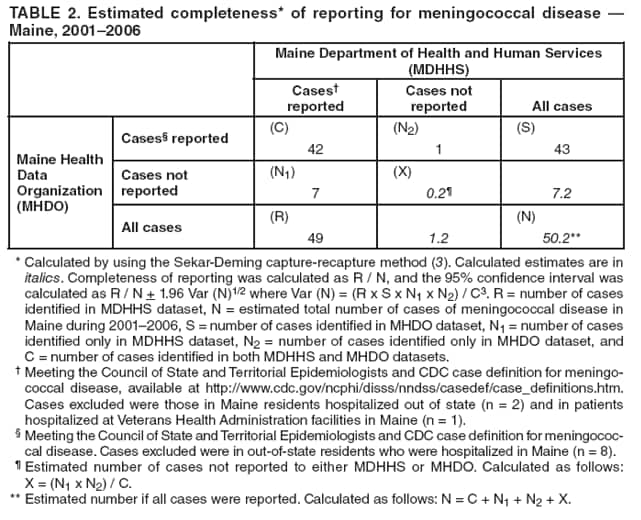 Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 2/25/2009 |
|||||||||
|