 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Guidance for Control of Infections with Carbapenem-Resistant or Carbapenemase-Producing Enterobacteriaceae in Acute Care FacilitiesInfection with carbapenem-resistant Enterobacteriaceae (CRE) or carbapenemase-producing Enterobacteriaceae is emerging as an important challenge in health-care settings (1). Currently, carbapenem-resistant Klebsiella pneumoniae (CRKP) is the species of CRE most commonly encountered in the United States. CRKP is resistant to almost all available antimicrobial agents, and infections with CRKP have been associated with high rates of morbidity and mortality, particularly among persons with prolonged hospitalization and those who are critically ill and exposed to invasive devices (e.g., ventilators or central venous catheters). This report provides updated recommendations from CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) for the control of CRE or carbapenemase-producing Enterobacteriaceae in acute care (inpatient) facilities. For all acute care facilities, CDC and HICPAC recommend an aggressive infection control strategy, including managing all patients with CRE using contact precautions and implementing Clinical and Laboratory Standards Institute (CLSI) guidelines for detection of carbapenemase production. In areas where CRE are not endemic, acute care facilities should 1) review microbiology records for the preceding 6--12 months to determine whether CRE have been recovered at the facility, 2) if the review finds previously unrecognized CRE, perform a point prevalence culture survey in high-risk units to look for other cases of CRE, and 3) perform active surveillance cultures of patients with epidemiologic links to persons from whom CRE have been recovered. In areas where CRE are endemic, an increased likelihood exists for imporation of CRE, and facilities should consider additional strategies to reduce rates of CRE (2). Acute care facilities should review these recommendations and implement appropriate strategies to limit the spread of these pathogens. For CRKP, the most important mechanism of resistance is the production of a carbapenemase enzyme, blakpc. The gene that encodes the blakpc enzyme is carried on a mobile piece of genetic material (transposon), which increases the risk for dissemination. Since first described in North Carolina in 1999, CRKP has been identified in 24 states and is recovered routinely in certain hospitals in New York and New Jersey (3). Analysis of 2007 data regarding health-care--associated infections reported to CDC indicated that 8% of all Klebsiella isolates were CRKP, compared with fewer than 1% in 2000 (CDC, unpublished data, 2008). CRKP poses significant treatment challenges, and CRKP infections have been associated with increased mortality, length of stay, and increased cost (4). The emergence and spread of CRKP and other types of CRE is another in a series of worrisome public health developments regarding antimicrobial resistance among gram-negative bacteria and underscores the immediate need for aggressive detection and control strategies (5). A difficulty in detecting CRE is the fact that some strains that harbor blakpc have minimal inhibitory concentrations (MICs) that are elevated but still within the susceptible range for carbapenems. Because these strains are susceptible to carbapenems, they are not identified as potential clinical or infection control risks using current susceptibility testing guidelines. To address this challenge, in January 2009, CLSI published a recommendation that carbapenem-susceptible Enterobacteriaceae with elevated MICs or reduced disk diffusion zone sizes be tested for the presence of carbapenemases using the modified Hodge test (MHT) (6). The MHT is a phenotypic test used to detect carbapenemases in isolates demonstrating elevated but susceptible carbapenem MICs and has demonstrated sensitivity and specificity exceeding 90% in identifying carbapenemase-producing Enterobacteriaceae (6). If the MHT reveals the presence of a carbapenemase, CLSI recommends that a comment be added to the microbiology report to inform clinicians and infection preventionists. Because treatment information on MHT-positive, carbapenem-susceptible isolates is limited, CLSI guidelines do not recommend any changes regarding the reporting of susceptibility results themselves. Strains of Enterobacteriaceae that test intermediate or resistant to carbapenems should be reported as such and do not need to be subjected to the MHT. Patients with unrecognized CRKP colonization have served as reservoirs for transmission during health-care--associated outbreaks (7). For example, during an outbreak of 39 cases of CRKP infection in a hospital in Puerto Rico in 2008, in addition to a review of infection control practices, active surveillance cultures were performed on patients in the same units as persons with confirmed CRKP infection. Cultures performed on 30 patients in the intensive care unit revealed two colonized patients who were not previously known to harbor CRKP and were not placed in contact precautions (CDC, unpublished data, 2008). Control of the outbreak was hindered by lack of compliance with infection control practices. Health-care personnel adherence to recommendations for gown and glove use was low (62%) at the hospital, and appropriate hand hygiene (i.e., hand washing or using a waterless alcohol-based hand rub before and after patient contact) was observed in only 48% of patient encounters. The hospital eventually was able to control the outbreak through enhanced infection control compliance, patient cohorting, and weekly perirectal surveillance cultures of patients in the outbreak units until no new cases were identified. Experience from the outbreak in Puerto Rico and elsewhere (notably Israel) suggests that early detection through use of targeted surveillance and introduction of strict infection control measures (including reinforcement of hand hygiene and contact precautions) can help control the spread of CRKP (7). Other recent reports have demonstrated that microbiologic surveillance for CRKP can be accomplished using broth-based culture techniques that are widely available and also by in-house prepared molecular techniques and a commercial chromogenic agar (4,7--9); however, the latter two methods are not currently approved by the Food and Drug Administration. The screening tests used in several studies were performed on rectal or perirectal swabs; limited data indicate that surveillance screening of stool specimens, rectal swabs, or perirectal swabs might produce higher yield than testing of other body sites (e.g., nares or skin) (9). CDC and HICPAC RecommendationsIn light of the clinical and infection control challenges posed by CRE and advances in the ability to detect these pathogens, CDC and HICPAC have developed new guidance for CRE infection prevention and control in an effort to limit the further emergence of these organisms (Box). These recommendations are based on strategies outlined in the 2006 HICPAC guidelines for management of multidrug-resistant organisms in health-care settings (2). All patients colonized or infected with CRE or carbapenemase-producing Enterobacteriaceae should be placed on contact precautions. Acute care facilities should establish a protocol, in conjunction with CLSI guidelines, to detect nonsusceptibility and carbapenemase production in Enterobacteriaceae, particularly Klebsiella spp. and Escherichia coli, and immediately alert epidemiology and infection control staff members if identified. All acute care facilities should review microbiology records for the preceding 6--12 months to ensure that previously unrecognized CRE cases have not occurred. If previously unrecognized cases are identified, facilities should conduct a point prevalence survey (a single round of active surveillance cultures) in units with patients at high risk (e.g., intensive care units, units where previous cases have been identified, and units where many patients are exposed to broad-spectrum antimicrobials) to identify any additional patients colonized with carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli. The recommended surveillance culture methodology is aimed at detecting carbapenem resistance or carbapenemase production in Klebsiella spp. and E. coli only, because 1) this method facilitates performing the test in the microbiology laboratory without the use of molecular methods and 2) these organisms represent the majority of CRE encountered in the United States. When a case of hospital-associated CRE is identified, facilities should conduct a single round of active surveillance testing of patients with epidemiologic links to the CRE case (e.g., those patients in the same unit or patients who have been cared for by the same health-care personnel). The goal of active surveillance is to identify undetected carriers of carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli. Identification of other cases among patients with epidemiologic links to persons with confirmed infection suggests patient-to-patient transmission (7); in such instances, infection prevention measures should be vigorously reinforced, and surveillance cultures repeated periodically (e.g., weekly) until no new cases are identified. Situations where periodic point prevalence surveys repeatedly fail to identify other colonized patients suggest that infection control measures at the facility are effective in controlling transmission. In such instances, consideration should be given to halting active surveillance cultures in response to clinical cases and replacing them with periodic point prevalence surveys in units with patients at high risk to ensure that carbapenem-resistant or carbapenemase-producing Klebsiella spp. and E. coli do not reemerge. Because the prevalence of CRE is low in the majority of U.S. hospitals, routine microbiologic surveillance of persons admitted, such as that performed in some facilities to detect carriage of methicillin-resistant Staphylococcus aureus, is not recommended. However, in some areas of the United States, notably New York City, CRE are routinely recovered, including from many patients who are admitted from the community. In these settings, point prevalence surveys in response to detected clinical cases might be less useful in controlling transmission of CRE. Facilities in regions where CRE are endemic should monitor clinical cases of CRE and implement the intensified (i.e., Tier 2) infection control strategies outlined in the 2006 HICPAC guidelines if rates of CRE are not decreasing (2). The challenges to hospitals of allocating additional resources to prevent and control CRE are balanced by the fact that an aggressive infection control strategy, such as that recommended in this report, offers an opportunity to limit the impact of these problematic pathogens while CRE prevalence remains low in most U.S. hospitals. Reported by: W Lledo, M Hernandez, E Lopez, MD, OL Molinari, MD, RQ Soto, MD, E Hernandez, N Santiago, M Flores; GJ Vazquez, MD, IE Robledo, MD, Univ of Puerto Rico; E García-Rivera, MD, A Cortes, M Ramos, Puerto Rico Dept of Public Health. R Goering, PhD, Creighton Univ, Omaha, Nebraska. A Srinivasan, MD, C Gould, MD, N Stine, M Bell, MD, K Anderson, B Kitchel, B Wong, JK Rasheed, PhD, J Patel, PhD, Div of Healthcare Quality Promotion, National Center for the Preparedness Detection and Control of Infectious Diseases; K Tomashek, MD, Div of Vector-Borne Infectious Diseases, National Center for Vector-Borne, Enteric, and Mycotic Diseases; E Llata, MD, CJ Gregory, MD, EIS officers, CDC. References
Box 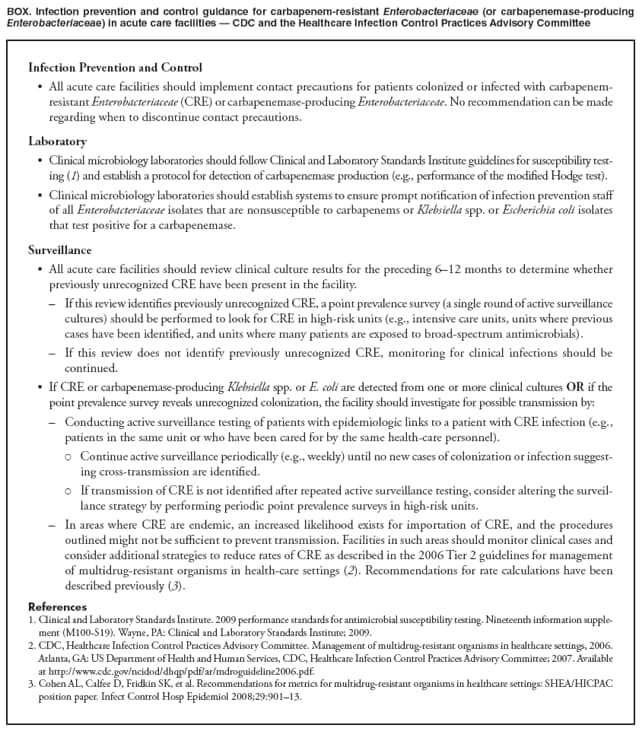 Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 3/19/2009 |
|||||||||
|