Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Apparent Disappearance of the Black-White Infant Mortality Gap --- Dane County, Wisconsin, 1990--2007
Please note: An erratum has been published for this article. To view the erratum, please click here.
Despite substantial reductions in U.S. infant mortality during the past several decades, black-white disparities in infant mortality persist (1). Among 40 states with sufficient numbers of black infant deaths to generate reliable rates for the years 2002--2004, Wisconsin had the highest black infant mortality rate (IMR) at 17.6 deaths per 1,000 live births, approximately three times the state rate for whites (2). However, in contrast to trends in Wisconsin and the other 39 states, the black IMR in Dane County, Wisconsin, has declined substantially, achieving parity with whites and meeting Healthy People 2010 objective 16-1 for reducing fetal and infant deaths (3). The county rate declined 67%, from 19.4 per 1,000 live births for the period 1990--2001 to 6.4 for the period 2002--2007. To gain understanding of this development, Public Health Madison Dane County (PHMDC) analyzed approximately 100,000 birth and death records from 1990 through 2007 for birthweight, gestational age, prenatal care, and other infant mortality risk factors. The main contributors to the decrease in black infant mortality were a large decrease in the extremely premature (≤28 weeks gestation) birth rate and a decrease in the mortality rate for newborns weighing <1,500 g. Because the observed trend in black infant mortality is based on small reductions in the absolute number of deaths (approximately three infants per year), conclusions based on these results should be considered preliminary, and additional studies are needed to confirm the reduction in rates over time. PHMDC is planning continued surveillance and other studies to determine whether the reduction in mortality is stable.
The population of Dane County, including the city of Madison, had grown to more than 472,000 in 2007, with blacks comprising 4.8% of the total. The black population and number of black births per year in the county have approximately doubled since 1990. Black women giving birth in Dane County are predominately poor ($28,103 median household income versus $50,927 for whites), and rely on subsidized health care (62% on Medicaid versus 13% for whites) (Wisconsin Department of Administration [WDA], 2000 U.S. Census, and Wisconsin Department of Health Services [WDHS], unpublished data, 2009). The proportions of black women giving birth who are unmarried (77% versus 19% for whites), and lacking higher education (71% have a high school diploma or less versus 21% for whites) have been stable since 1990 (4).
Wisconsin birth, infant death, and fetal death records (certificates) contain more than 100 data elements that affect birth outcomes, including infant and fetal characteristics, maternal demographics and behaviors, medical conditions diagnosed before and during pregnancy, and complications of labor and delivery. Using 97,590 birth, infant death, and fetal death records compiled by WDHS, mean non-Hispanic black and non-Hispanic white IMRs were calculated for 1990--2001 and 2002--2007. For each period, percentages and mortality rates were calculated, by race, for prematurity (defined as <37 weeks gestation), extreme prematurity (defined as ≤28 weeks gestation), low birthweight (defined as <2,500 g), very low birthweight (defined as <1,500 g), and other risk factors. Locally weighted polynomial regression was used to display the data graphically. Race of infant was assigned according to race of mother. Fetal death was defined according to the standard form* used in all Wisconsin hospitals throughout the study period as any delivery of 20 weeks or more gestation or if a fetus weighs 350 g or more when death is indicated by the fact that the fetus shows no evidence of life.
During 1990--2007, 79,439 white births, 405 white infant deaths (14--38 per year), 6,410 black births, and 90 black infant deaths (1--10 per year) occurred in Dane County (Table 1). During the 1990s, black-white infant mortality disparity in Dane County was relatively constant and similar to the rest of the state (a black-white ratio of approximately 3:1). In 2002, Dane County black IMRs began to decline, achieving parity with whites during 2004--2007, even though Dane County white IMRs also had improved (Figure).
Analysis of risk factors indentified in birth records showed declines in smoking and teenage pregnancy (especially among persons aged 15--17 years) and an increase in high school graduation for blacks, although significant racial disparities persist (Table 2). The percentage of black women receiving adequate, adequate plus, and intermediate prenatal care (measured by expected number and timing of clinical visits using the Adequacy of Prenatal Care Utilization Index [the Kotelchuck Index]) increased from 81.6% to 85.3%. Improvement in quality of care received is suggested by an increase in maternal medical conditions recorded on the birth record from 48.9% to 59.4%, and a decrease in birth record reported obstetrical complications from 50.2% to 42.5%, coupled with substantial reductions in infant mortality for black women with reported medical conditions or obstetrical complications (Table 2). The decrease in infant deaths per 1,000 live births for babies born to black mothers with previous child deaths (from 84.2 IMR [eight of 95] for 1990--2001 to zero IMR [none of 47] for 2002--2007) and to those with previous premature births (from 54.3 IMR for 1990--2001 to 8.1 IMR for 2002--2007) underscores major improvement in birth outcomes among highest-risk pregnancies.
The change in infant mortality risk factors for blacks that most affected the IMR over time was a decline in the percentage of extremely premature births, from 2.8% to 1.1%. The mean IMR of 391 per 1,000 for black infants <1,500 g for 1990--2001 dropped to 154 per 1,000 for 2002--2007, a decline in birthweight-specific mortality of 61%. For all races, during the 18 years studied, 70% of infant deaths occurred during the neonatal period (≤28 days of life).
Reported by: T Schlenker, MD, M Ndiaye, MD, Public Health Madison and Dane County, Wisconsin.
Editorial Note:
IMRs reflect the health of infants, their mothers, their families, and the communities into which they are born and are universally recognized as key indicators of the health of populations. The United States ranks poorly among industrialized nations in this regard, largely because of excessive infant mortality among blacks (3). Many have suggested that the black-white infant mortality gap in the United States will not decrease without reducing the high rates of extreme prematurity and very low birthweight births among blacks (3,5,6). In recent years, despite improved gestational age-specific survival, the U.S. black-white infant mortality gap has widened (7,8). In contrast, in Dane County, Wisconsin, decreases in the rates of extreme prematurity and very low birthweights and increases in birthweight and gestational age-specific survival appear to have eliminated the black-white infant mortality gap. Thus, during 2002--2007, 34 black infants who might have died, survived, and 45 who might have been born extremely premature, at high risk for life-long disabilities, were instead born at or closer to term.
The apparent disappearance of the black-white infant mortality gap in Dane County is likely attributed to the convergence of the two related but independent trends: greater survival of high-risk infants and fewer high-risk infants being born. The main factors for these trends were a large decline in the extremely premature (<28 weeks gestation) birth rate and a decline in the mortality rate for babies born weighing <1,500 g. Although extremely premature babies constitute a very small percentage of total live births, their IMR is approximately 100 times that of term infants, and they account for approximately half of all infant deaths (population-attributable fraction [PAF] for all races = 51%, PAF for blacks = 70%) (9). Extremely premature births account for the larger part of the black-white infant mortality gap in Dane County and nationally (2,9,10). The local trend toward fewer extremely premature births among blacks appears to have begun in the mid-1990s, followed by marked improvements in survival of extremely premature and low-birthweight infants born at local hospitals.
No significant changes in local health-care systems, infrastructure, or practice that correspond to these improvements have been identified. Nearly all (98%) of Dane County births occur at two local hospitals, both of which have full obstetrical services and level-three neonatal intensive-care units (WDA, 2000 U.S. Census, and WDHS hospital discharge data, personal communication, February 2009). No other hospitals in the county offer obstetrical services and delivery. During the study period, no changes in routine or high-risk obstetrical or neonatal referral patterns were recognized.
Factors that might contribute to improved birth outcomes are broader health insurance coverage, advances in prenatal and postnatal care, and targeted public health programs such as Perinatal Care Coordination services and the federal Women, Infants, and Children health-care and nutrition program. These targeted programs are available statewide, suggesting that differences in health-care access and quality specific to Dane County, and community quality-of-life elements, including improved neighborhood safety, organizational support and advocacy for black women and families, social inclusion, and improved economic status, might be important variables for further study.
Conclusions based on these data should be considered preliminary because closer examination of demographics trends in Dane County are needed to understand the small changes in annual number of black infant deaths. The declining black infant mortality in Dane County has continued since 2002 and coincides with a growing black population of stable fertility. The steadily declining rate of extremely premature births, which began in the mid-1990s, represents larger annual numbers than infant deaths, and thereby might provide additional insight into these trends.
The findings in this report are subject to at least four limitations. First, delivery room misclassification of infant death as fetal death might occur, thereby artificially reducing the rate of infant deaths. However, systematic misclassification appears unlikely because both fetal death and infant death declined during the study period. Second, vital records do not provide information on important contextual risk factors for infant mortality (e.g., paternal involvement and quality of prenatal care). Also, vital records have poor validity for reporting medical risk factors and complications of pregnancy, and often lack details on cause of death. Third, key health-care variables such as neonatal intensive-care unit admissions and health insurance coverage were not examined. Finally, improved or expanded birth record coding, if it occurred, might be mistaken for improvement in quality of care.
These findings should be interpreted with caution and studied further to determine if the apparent reduction in deaths is an artifact or can be attributed to yet unidentified factors, such as changes in medical care or population characteristics. PHMDC, in collaboration with state and local health departments and the University of Wisconsin, has initiated an in-depth, follow-up investigation to include interviews with mothers, hospital chart reviews, and community resource assessments. Detailed vital records analyses are planned comparing Dane County to other population centers in Wisconsin where excessive infant mortality persists. The collaborative investigation will document and compare pre-, peri-, and post-natal care; individual characteristics of pregnant women; and the social and physical environments in which those women live. These pending analyses could reveal key factors contributing to fewer black extremely premature births and associated improved survival of extremely premature and low-birthweight infants in Dane County. Public health officials who conduct similar evaluations of IMRs in their local jurisdictions should be alert for similar infant mortality patterns during this period. Reports from such studies could provide supporting information to aid in understanding these preliminary findings and direct future research.
References
- CDC. Infant mortality and low birth weight among black and white infants---United States, 1980--2000. MMWR 2002;51:589--92.
- Mathews TJ, MacDorman MF. Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl Vital Stat Rep 2007;55(14).
- US Department of Health and Human Services. Reduce fetal and infant deaths. Objective 16-1. Healthy People 2010 (conference ed, in 2 vols). Washington, DC: US Department of Health and Human Services; 2000. Available at http://www.healthypeople.gov/document/html/volume2/16mich.htm.
- Wisconsin Department of Health Services. Birth record file, 1990--2007 [Database]. Madison, WI: Wisconsin Department of Health Services, Division of Public Health, Bureau of Health Information and Policy; 2009.
- Carmichael SL, Iyasu S. Changes in the black-white infant mortality gap from 1983 to 1991 in the United States. Am J Prev Med 1998;15:220--7.
- Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics 2008;118:1566--73.
- Alexander GR, Wingate MS, Bader D, Kogan MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. Am J Obstet Gynecol 2008;198:51.e1--9.
- Allen MC, Alexander GR, Tompkins ME, Hulsey TC. Racial differences in temporal changes in newborn viability and survival by gestational age. Paediatr Perinatal Epidemiol 2000;14:152--8.
- Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15--9.
- Schempf AH, Branum AM, Lukacs SL, Schoendorf KC. The contribution of preterm birth to the black-white infant mortality gap, 1990 and 2000. Am J Public Health 2007;97:1255--60.
* WDHS, Division of Public Health, Report of Fetal Death, standard form DPH 5042.
FIGURE. Infant mortality rates per 1,000 live births, by race --- Wisconsin and Dane County, 3-year moving averages,* 1990--2007
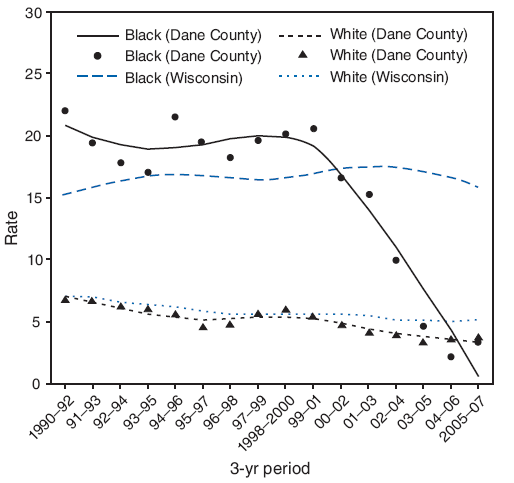
* Fitted lines and scatter points.
Alternative Text: The figure above shows the infant mortality rates (IMRs) per 1,000 live births, by race; 3-year moving averages for Wisconsin and Dane County, from 1990 through 2007. During the 1990s, black-white infant mortality disparity in Dane County was relatively constant and similar to the rest of the state (a black-white ratio of approximately 3:1). In 2002, Dane County black IMRs began to decline, achieving parity with whites during 2004-2007, even as Dane County white IMRs also improved.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 5/27/2009


