Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Surveillance for the 2009 Pandemic Influenza A (H1N1) Virus and Seasonal Influenza Viruses --- New Zealand, 2009
The 2009 pandemic influenza A (H1N1) virus,* which was first identified in the United States (1) and Mexico (2), was imported into New Zealand by a high school group returning from Mexico in late April 2009. By June, sustained community transmission of the virus had been established in New Zealand. To track the incidence of influenza-like illness (ILI) and compare the number of viruses identified as 2009 pandemic influenza A (H1N1) with the number identified as seasonal influenza, New Zealand public health officials analyzed weekly data from the country's sentinel general practitioner (GP) surveillance system and nonsentinel laboratory surveillance network for the period extending from the week ending May 3 through the week ending August 2. This report describes the results of those analyses, which determined that the number of viruses identified as 2009 pandemic influenza A (H1N1) rapidly overtook the number identified as seasonal influenza, and the peak weekly consultation rate for ILI was three times the peak rate in New Zealand during the same period in 2008. These findings demonstrate the value of using integrated epidemiologic and virologic surveillance in New Zealand to monitor the scope of an influenza epidemic, identify circulating strains, assist public health control measures, and guide effective use of influenza vaccines and antivirals.
GP Sentinel Influenza Surveillance
The New Zealand sentinel GP surveillance system was established in 1991 as part of the World Health Organization (WHO) global program for influenza surveillance; the system is operated nationally by the Institute of Environmental Science and Research (ESR) and locally by surveillance coordinators in the public health units of the country's 24 health districts. Surveillance is conducted during May--September (the southern hemisphere winter) by volunteer sentinel GPs distributed across New Zealand. The sentinel system defines a case of ILI as an acute respiratory tract infection characterized by an abrupt onset of at least two of the following: fever, chills, headache, and myalgia. Each participating GP records the daily number of patients consulted for ILI, along with the patient's age. These data are collected by local district coordinators each week. National ILI consultation rates are calculated weekly using the sum of the GP patient populations as the denominator.
The national level of ILI activity is described using a set of threshold values. A weekly consultation rate <50 consultations per 100,000 patient population is described as baseline activity. A weekly rate of 50--249 is considered indicative of normal seasonal influenza activity. Within the normal seasonal activity, 50--99 is low activity, 100--149 is moderate, and 150--249 is high activity. A rate of 250--399 indicates higher than expected influenza activity and ≥400 indicates an epidemic level of influenza activity. Because age group--specific GP patient population data are not provided by participating GPs, the denominator for age group--specific ILI consultation rates is based on New Zealand census data with the assumption that the age group distribution for GP patient populations is the same as the distribution for the entire New Zealand population.
Each participating GP also collects three respiratory samples (i.e., nasopharyngeal or throat swab) each week from the first ILI patient examined on Monday, Tuesday, and Wednesday. The GPs forward these samples to the WHO National Influenza Centre at ESR or to hospital virology laboratories in Auckland, Waikato, or Christchurch for virus characterization. Laboratory identification methods include molecular detection by polymerase chain reaction, isolation of the virus, or direct detection of viral antigen. Influenza viruses are typed and subtyped as influenza A, B, seasonal A, seasonal A (H1N1), seasonal A (H3N2), or 2009 pandemic influenza A (H1N1). The virus identification data are forwarded by hospital laboratories to ESR each week. ESR compiles and reports national epidemiologic and virologic data on influenza to WHO and also publishes these data on the ESR website.†
For the 2009 influenza season, 95 sentinel GPs were recruited, representing all of the country's 24 health districts and with a combined patient population of 409,044, approximately 9.6% of the New Zealand population. During the study period, the weeks ending May 3 through August 2, a total of 6,280 consultations for ILI were reported from the 24 health districts. Cumulative incidence of ILI consultation during this period was 1,518 per 100,000 patient population. As in previous years, 2009 consultation rates for ILI varied greatly among health districts. During July 6--12, a week of high influenza activity, multiple health districts reported ≥400 ILI consultations per 100,000 patient population, which is indicative of epidemic activity. Among those health districts with epidemic activity, South Auckland had the highest consultation rate (1,308 per 100,000), followed by Wellington (709) and South Canterbury (505) (Figure 1).
Weekly national ILI consultation rates for the study period were compared with the same period in 2008 and 2007. From the week ending May 3 through the week ending June 7, the weekly ILI consultation rate remained below the baseline level of 50 consultations per 100,000 patient population (Figure 2). The ILI rate first exceeded the baseline level in the second week of June and increased sharply from the week ending June 21 to the week ending July 12. The ILI consultation rate peaked at 287 consultations per 100,000 patient population in the week ending July 19, approximately three times the peak rate of 95 consultations recorded in 2008.
During the study period, the highest ILI consultation rates were recorded among children and youths aged ≤19 years. Children aged 1--4 years had the highest ILI consultation rate (154 per 100,000 age group population), followed by infants aged <1 year (110 per 100,000), and persons aged 5--19 years (97), 20--34 years (96), 35--49 years (66), 50--64 years (57) and ≥65 years (23).
A total of 1,963 swabs were sent to virology laboratories from sentinel GPs during the study period, compared with 543 swabs recorded for the same period in 2008. From the swabs recorded in 2009, 527 influenza viruses were identified. The predominant strain was 2009 pandemic influenza A (H1N1) (332 [63%]), followed by seasonal influenza A (72 [14%]), seasonal influenza A (H1N1) (70 [13%]), influenza A not subtyped (44 [8%]), seasonal influenza A (H3N2) (8), and influenza B not typed (1) (Figure 3). The percentage of viruses identified as 2009 pandemic influenza A (H1N1) increased from 14% during the week of June 8--14 to 80% during the week of June 29--July 5.
Nonsentinel Laboratory Surveillance
Nonsentinel laboratory surveillance is conducted by the New Zealand virus laboratory network consisting of the National Influenza Centre at ESR and four hospital virology laboratories in Auckland, Waikato, Wellington, and Christchurch. ESR collates year-round national laboratory data on influenza from mainly hospital in-patient and outpatients during routine viral diagnosis. In addition, this laboratory network conducted 2009 pandemic influenza A (H1N1)--related public health surveillance among arriving travelers and the contacts of patients with confirmed 2009 pandemic influenza A (H1N1) virus infection. During the containment phase (April 25--June 21), when New Zealand public health officials tried to prevent transmission from arriving travelers to their close contacts and contain transmission within small, localized clusters of 2009 pandemic influenza A (H1N1) virus infection, respiratory samples largely were collected from persons with suspected 2009 pandemic influenza A (H1N1) virus infection. However, during the management phase (June 22--August 2), when public health officials tried to mitigate the impact of sustained community transmission of the 2009 pandemic influenza A (H1N1) virus, the sampling priority was limited to persons with moderate or severe illness or who were vulnerable to severe illness.
A total of 3,931 influenza viruses were reported from the nonsentinel laboratory surveillance network during the study period. The predominant strain was 2009 pandemic influenza A (H1N1) (2,116), followed by influenza A (not subtyped) (1,076), seasonal influenza A (H1N1) virus (444), seasonal influenza A virus (244), seasonal influenza A (H3N2) virus (49), and influenza B (not typed) (2) (Figure 3). The percentage of viruses identified as 2009 pandemic influenza A (H1N1) increased from 22% during June 8--14 to 66% during June 29--July 5.
Reported by: QS Huang, PhD, D Bandaranayake, PhD, MBBS, LD Lopez, MSc, R Pirie, M Peacey, PhD, R Hall, PhD, J Bocacao, B Adlam, MBChB, Royal New Zealand College of General Practitioners; V Hope, MBChB, Institute of Environmental Science and Research; M Croxson, MBChB, I Basu, PhD, S Roberts, MBChB, Auckland Hospital Virology Laboratory; J Lindeman, C Gale, C Mansell, MBChB, Waikato Virology Laboratory; S Rooker, PhD, L Olsen, T Blackmore, MBChB, Wellington Virology Laboratory; L Jennings, PhD, A Werna, MBChB, K Barrett, MSc, Christchurch Virology Laboratory; D Hunt, MBChB, M Jacobs, MBChB, F McGrath, MBChB, Ministry of Health; G Mackereth, BVSc, JS O'Keefe, BVSc, PhD, Ministry of Agriculture and Forestry Investigation and Diagnostic Centre; M Baker, MBChB, Univ of Otago,Wellington, New Zealand.
Editorial Note:
On April 25, New Zealand became the first country in the southern hemisphere to report importation of 2009 pandemic influenza A (H1N1) virus infection, following the return of an airline flight containing a group of high school students who had traveled to Mexico. A concerted containment effort (e.g., screening arriving airline passengers for ILI, case isolation, quarantine of contacts, and treatment with oseltamivir) by the government, public health officials, border officials, hospitals, primary-care workers, and laboratorians appeared to delay establishment of community transmission for several weeks. New Zealand entered its management phase on June 22 after sentinel and nonsentinel surveillance data indicated that 2009 pandemic influenza A (H1N1) had established sustained community transmission. At that point, the objective of influenza surveillance in New Zealand shifted from early detection of individual cases toward tracking the progression and characteristics of the pandemic by monitoring the virulence, antigenic drift, and antiviral susceptibility of the 2009 pandemic influenza A (H1N1) virus, and also its clinical and epidemiologic features.
Since 1991, sentinel GP surveillance for influenza has operated continuously in New Zealand (3) and has been recognized as one of the best tools for understanding the influenza burden and monitoring year-to-year disease trends. Consultation rates for ILI in New Zealand in 2009 have been the highest observed since 1997 (3). However, the consultation rates likely underestimate the actual incidence of ILI because many persons with ILI will not consult a GP. Beginning June 22, which marked the start of the management phase of the influenza pandemic in New Zealand, national public health officials recommended that only persons who were more seriously ill with ILI or at risk for serious complications from influenza visit a GP.
Both sentinel GP surveillance and nonsentinel laboratory surveillance indicated that the number of viruses identified as 2009 pandemic influenza A (H1N1) rapidly overtook the number identified as seasonal influenza. However, age distribution for 2009 pandemic influenza A (H1N1) was different between sentinel and nonsentinel surveillance. Caution should be used when interpreting nonsentinel surveillance data from clinical and epidemiologic perspectives because the sampling criteria for the nonsentinel laboratory surveillance are not as consistent as those for sentinel GP surveillance. For example, the groups selected for sampling by nonsentinel surveillance were changed from arriving travelers and contacts of patients with 2009 pandemic influenza A (H1N1) virus infection (during the containment phase) to persons with moderate or severe illness or who were vulnerable to severe influenza complications (during the management phase).
Like other southern hemisphere countries with temperate climates, New Zealand entered its winter season with cocirculation of both seasonal and 2009 pandemic influenza A (H1N1) strains. By the week ending July 5, 80% of the viruses identified by sentinel GP surveillance were the 2009 pandemic influenza A (H1N1) virus. In neighboring Australia, the state of Victoria reported that the 2009 pandemic influenza A (H1N1) virus accounted for 87% of all influenza isolates by the week ending July 12 (4). Public health officials are watching closely to see whether the 2009 pandemic influenza A (H1N1) virus becomes equally dominant in other southern hemisphere countries and in northern hemisphere countries during their approaching influenza seasons.
Acknowledgments
The findings in this report are based, in part, on data provided by the Ministry of Health, sentinel GPs and nurses, and influenza surveillance personnel.
References
- CDC. Swine influenza A (H1N1) infection in two children---southern California, March--April 2009. MMWR 2009;58:400--2.
- CDC. Outbreak of swine-origin influenza A (H1N1) virus infection---Mexico. March--April 2009. MMWR 2009;58:467--70.
- Huang QS, Lopez LD, McCallum L, Adlam B. Influenza surveillance and immunisation in New Zealand, 1997--2006. Influenza Other Respi Viruses 2008;2:139--45.
- Victoria Infectious Diseases Reference Laboratory. The 2009 Victorian influenza vaccine effectiveness audit report. Report no. 11. Available at http://www.vidrl.org.au/surveillance/flu%20reports/flurpt09/pdf_files/flu0911.pdf.
* Previously referred to in MMWR reports as the novel influenza A (H1N1) virus.
† Available at http://www.surv.esr.cri.nz/virology/influenza_weekly_update.php.
FIGURE 1. Consultation rates per 100,000 patient population for influenza-like illness (ILI), by health district --- sentinel general practitioner surveillance system,* New Zealand, July 6--12, 2009
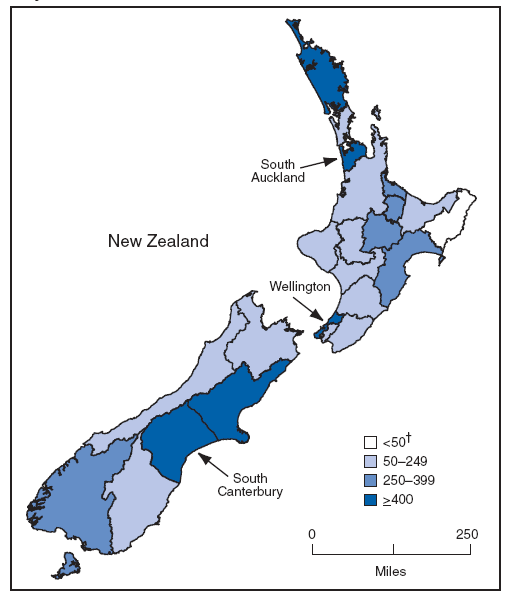
* 95 general practitioners, representing all 24 health districts, with a combined patient population of 409,044, approximately 9.6% of the New Zealand population.
† A weekly rate <50 ILI consultations per 100,000 patient population is considered baseline activity. A rate of 50--249 is considered indicative of normal seasonal influenza activity, and a rate of 250--399 indicative of higher than expected influenza activity. A rate ≥400 ILI consultations per 100,000 patient population indicates an epidemic level of influenza activity.
Alternative Text: The figure above shows consultation rates per 100,000 patient population for influenza-like illness (ILI), by health district, from the sentinel general practitioner surveillance system for New Zealand from July 6-12, 2009. During July 6-12, a week of high influenza activity, multiple health districts reported >400 ILI consultations per 100,000 patient population, which is indicative of epidemic activity. Among those health districts with epidemic activity, South Auckland had the highest consultation rate (1,308 per 100,000), followed by Wellington (709), and South Canterbury (505).
FIGURE 2. National consultation rates for influenza-like illness (ILI) compared with 2008 and 2007, by week --- sentinel general practitioner surveillance system,* New Zealand, week ending May 3 through week ending August 2, 2009
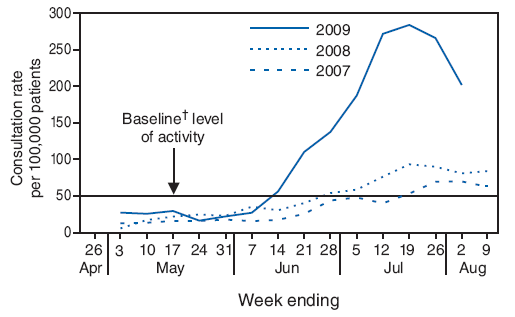
* 95 general practitioners, representing all 24 health districts, with a combined patient population of 409,044, approximately 9.6% of the New Zealand population.
† A weekly rate <50 ILI consultations per 100,000 patient population is considered baseline activity.
Alternative Text: The figure above shows national consultation rates for influenza-like illness (ILI) compared with 2008 and 2007, by week, from the sentinel general practitioner surveillance system for New Zealand, for the period from the week ending May 3 through the week ending August 2, 2009. Weekly national ILI consultation rates for the study period were compared with the same period in 2008 and 2007. From the week ending May 3 through the week ending June 7, the weekly ILI consultation rate remained below the baseline level of 50 consultations per 100,000 patient population.
FIGURE 3. Number of influenza viruses identified, by type --- New Zealand, week ending May 3 through week ending August 2, 2009
![The figure shows the number of influenza viruses identified by two surveillance systems, by type, in New Zealand for the period from the week ending May 3 through week ending August 2, 2009. For the general practitioner sentinel surveillance system, the predominant strain was 2009 pandemic influenza A (H1N1) (332 [63%]), followed by seasonal influenza A (72 [14%]), seasonal influenza A (H1N1) (70[13%]), influenza A not subtyped (44 [8%]), seasonal influenza A (H3N2) (8), and influenza B not typed. For the nonsentinel laboratory surveillance network, the strain was 2009 pandemic influenza A (H1N1) (2,116), followed by influenza A (not subtyped) (1,076), seasonal influenza A (H1N1) virus (444), seasonal influenza A virus (244), seasonal influenza A (H3N2) virus (49), and influenza B (not typed) (2).](figures/m833a2f3.gif)
* 527 influenza viruses identified by 95 general practitioners, representing all 24 health districts, with a combined patient population of 409,044, approximately 9.6% of the New Zealand population.
† 3,931 influenza viruses indentified by the National Influenza Center at the Institute of Environmental Science and Research, plus hospital laboratories at Auckland, Waikato, Wellington, and Christchurch.
Alternative Text: The figure above shows the number of influenza viruses identified by two surveillance systems, by type, in New Zealand for the period from the week ending May 3 through week ending August 2, 2009. For the general practitioner sentinel surveillance system, the predominant strain was 2009 pandemic influenza A (H1N1) (332 [63%]), followed by seasonal influenza A (72 [14%]), seasonal influenza A (H1N1) (70[13%]), influenza A not subtyped (44 [8%]), seasonal influenza A (H3N2) (8), and influenza B not typed. For the nonsentinel laboratory surveillance network, the strain was 2009 pandemic influenza A (H1N1) (2,116), followed by influenza A (not subtyped) (1,076), seasonal influenza A (H1N1) virus (444), seasonal influenza A virus (244), seasonal influenza A (H3N2) virus (49), and influenza B (not typed) (2).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 8/27/2009


