* Information on blood lead laboratory results reporting requirements by state is available at the ABLES program website http://www.cdc.gov/niosh/topics/ABLES/State-Contacts.html.
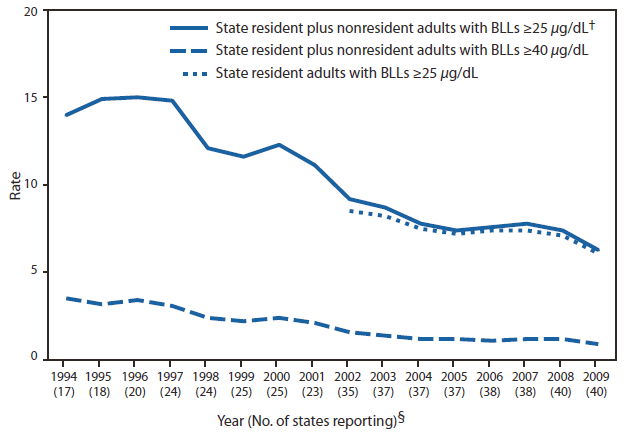
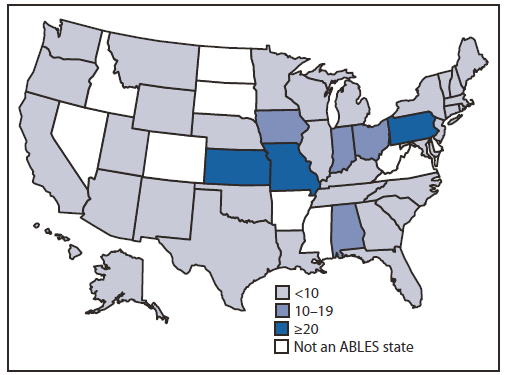
† A total of 40 states submitted data in 2008 and 2009: Alabama, Alaska, Arizona, California, Connecticut, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, New Hampshire, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Utah, Vermont, Washington, Wisconsin, and Wyoming.
§ A total of 38 of the 40 states (all except Indiana and Kentucky) provided data on industry in 2009 and 37 in 2008 (all except Alabama, Indiana, and Kentucky).
¶ Interventions include 1) conducting follow-up interviews with physicians, employers, and workers; 2) investigating worksites; 3) providing technical assistance; 4) providing Occupational Safety and Health Administration (OSHA) referrals for consultation and enforcement; and 5) developing and disseminating educational materials and conducting outreach programs.
** Additional information available at http://www.osha.gov/OshDoc/Directive_pdf/CPL_03-00-0009.pdf.
†† Engineering controls and good work practices are the preferred methods of minimizing exposures to airborne lead at the worksite. Engineering control methods that can be used to reduce or eliminate lead exposures can be grouped into three main categories: 1) substitution, 2) isolation, and 3) ventilation. Additional information available at http://www.osha.gov/dts/osta/otm/otm_v/otm_v_3.html#2.
§§ Additional information available at http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=fact_sheets&p_id=161.
 ShareCompartir
ShareCompartir