 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Implementing Recommendations for the Early Detection of Breast and Cervical Cancer Among Low-Income WomenThe material in this report was prepared for publication by: National Center for Chronic Disease Prevention
and Health Promotion Division of Cancer Prevention and Control Implementing Recommendations for the Early Detection of Breast and Cervical Cancer Among Low-Income WomenHerschel W. Lawson, M.D. Abstract Scope of the Problem: Among U.S. women, breast cancer is the most commonly diagnosed cancer and remains second only to lung cancer as a cause of cancer-related mortality. The American Cancer Society (ACS) estimates that 182,800 new cases of female breast cancer and 41,200 deaths from breast cancer will occur in 2000. Since the 1950s, the incidence of invasive cervical cancer and mortality from this disease have decreased substantially; much of the decline is attributed to widespread use of the Papanicolaou (Pap) test. ACS estimates that 12,800 new cases of invasive cervical cancer will be diagnosed, and 4,600 deaths from this disease will occur in the United States in 2000. Etiologic Factors: The risk for breast cancer increases with advancing age; other risk factors include personal or family history of breast cancer, certain benign breast diseases, early age at menarche, late age at menopause, white race, nulliparity, and higher socioeconomic status. Risk factors for cervical cancer include certain human papilloma virus infections, early age at first intercourse, multiple male sex partners, a history of sexually transmitted diseases, and low socioeconomic status. Black, Hispanic, or American Indian racial/ethnic background is considered a risk factor because cervical cancer detection and death rates are higher among these women. Recommendations for Prevention: Because studies of the etiology of breast cancer have failed to identify feasible primary prevention strategies suitable for use in the general population, reducing mortality from breast cancer through early detection has become a high priority. The potential for reducing death rates from breast cancer is contingent on increasing mammography screening rates and subsequently detecting the disease at an early stage -- when more treatment options are available and survival rates are higher. Effective control of cervical cancer depends primarily on early detection of precancerous lesions through use of the Papanicolaou test, followed by timely evaluation and treatment. Thus, the intended outcome of cervical cancer screening differs from that of breast cancer screening. In 1991, the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) was implemented to increase breast and cervical cancer screening among uninsured, low-income women. Research Agenda: To support recommended priority activities for NBCCEDP, CDC has developed a research agenda comprising six priorities. These six priorities are a) determining effective strategies to communicate changes in NBCCEDP policy to cancer screening providers and women enrolled in the program; b) identifying effective strategies to increase the proportion of enrolled women who complete routine breast and cervical cancer rescreening according to NBCCEDP policy; c) identifying effective strategies to increase NBCCEDP enrollment among eligible women who have never received breast or cervical cancer screening; d) evaluating variations in clinical practice patterns among providers of NBCCEDP screening services; e) determining optimal models for providing case-management services to women in NBCCEDP who have an abnormal screening result, precancerous breast or cervical lesion, or a diagnosis of cancer; and f) conducting economic analyses to determine costs of providing screening services in NBCCEDP. Conclusion: The NBCCEDP, through federal, state, territorial, and tribal governments, in collaboration with national and community-based organizations, has increased access to breast and cervical cancer screening among low-income and uninsured women. This initiative enabled the United States to make substantial progress toward achieving the Healthy People 2000 objectives for breast and cervical cancer control among racial/ethnic minorities and persons who are medically underserved. A continuing challenge for the future is to increase national commitment to providing screening services for all eligible uninsured women to ultimately reduce morbidity and mortality from breast and cervical cancer. INTRODUCTIONAlthough the causes and natural histories of breast and cervical cancer are different, the public health responses to these diseases have been similar. Early detection of breast cancer and primary prevention of cervical cancer are possible through community-based screening programs; however, early detection of both breast and cervical cancer is less common among low-income* women (1). This report presents morbidity and mortality data regarding breast and cervical cancer, screening recommendations, an update on the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), and recommended priority activities for NBCCEDP. NBCCEDP is a major public health effort to increase breast and cervical cancer screening among uninsured, low-income women. SCOPE OF THE PROBLEMBreast CancerAmong women in the United States, breast cancer is the most commonly diagnosed cancer and remains second only to lung cancer as a cause of cancer-related death. The American Cancer Society (ACS) estimates that 182,800 new cases of female breast cancer and 41,200 deaths from breast cancer will occur in 2000 (2). In 1996, data from the National Cancer Institute's (NCI) Surveillance, Epidemiology, and End Results (SEER) Program† indicated that the incidence of breast cancer increased 25.3% during 1973-1996 (Figure 1). Most of the increase occurred during 1973-1991; incidence rates remained stable during 1992-1996. In 1996, the incidence rate for breast cancer was 110.7 cases per 100,000 women, a 29.6% increase since 1980. In addition, in 1996, the case-fatality rate for breast cancer was 24.3 per 100,000 women, a 4.5% decrease since 1992, representing the first sustained decline in breast cancer-related mortality since 1973 (when SEER surveillance for breast cancer began). Although the percentage increases in incidence during 1973-1996 were similar among black and white women, the percentage decrease in mortality during 1992-1996 was substantially greater among white women than black women (3,4). Overall during 1992-1996, breast cancer incidence rates were higher among white women (113.1 per 100,000) than black women (100.3), but breast cancer death rates were lower among white women (25.1) than black women (32.0). Furthermore, these race-specific differences in rates varied by age. Among women aged <50 years, the incidence rate for black women (32.7) was higher than that for white women (31.1). Among women aged >50 years, the rate was higher for white women (365.8) than for black women (308.7). The death rate among women aged <65 years was higher for black women (20.4) than for white women (14.3). Although the death rate among women aged >65 years was higher for white women than for black women before 1987, recent data indicate that the death rate among this age group is higher for black women (130.9) than for white women (124.0) (4,5). On the basis of SEER data for 1988-1992 (most recent data available), incidence rates were highest for white (145.7), Hawaiian (105.6), and black women (95.4) and lowest for Korean (28.5), American Indian (31.6), and Vietnamese (37.5) women. Incidence rates among white, non-Hispanic women were four times higher than among Korean women (3). Stage-specific survival rates among women with breast cancer have increased slightly since the 1970s (6). The overall 5-year survival rates for women during 1989-95 were 86% for white women and 71% for black women (4). Survival was greatest at the earliest stage of disease. Age-specific survival rates were similar for white and black women. One explanation for the disparity in race-specific survival rates is that white women, on average, seek medical care for tumors at an earlier stage of disease than black women. However, the interim between symptom recognition and medical consultation does not appear to account for these race-specific differences in survival rates or stage at diagnosis of breast cancer (6). Limited data are available regarding survival for other ethnic groups in the United States. In a study of stage at diagnosis and tumor histology among white and Asian women, the 5-year survival rate at all stages was higher among Asian women than among white women (7). In addition, based on data from another study, the survival rate among Hispanic women is similar to the rate among white women in the United States (8). Cervical CancerSince the 1950s, the incidence of invasive cervical cancer and mortality from this disease have decreased substantially. In large part, the decline has been attributed to widespread use of the Papanicolaou (Pap) test -- a highly effective preventive measure. However, the rate of decline in invasive cervical cancer has slowed since the early 1980s and appears to have stabilized in recent years (Figure 2). ACS projects that approximately 12,800 cases of invasive cervical cancer will be diagnosed and that approximately 4,600 cervical cancer deaths will occur in the United States in 2000 (2). During 1992-1996, the incidence rate at SEER sites was 7.9 cases per 100,000 women, and the death rate for cervical cancer was 2.8 per 100,000 women (4). On the basis of SEER data, both incidence and death rates for cervical cancer vary among racial/ethnic groups. The incidence rate for cervical cancer is highest among Vietnamese women (43.0), and the death rate for cervical cancer is highest among black women (6.7) (3). The incidence rate among black women (11.2 per 100,000) is approximately 50% higher than among white women (7.3) (3,4). Death rates among black women (5.9) are approximately twice as high as those among white women (2.4). Although the disparities in rates between blacks and whites have declined since 1990, differences in rates persist. This persistent disparity has been attributed to several factors, including differences in the prevalence of risk factors for cervical cancer; differences in screening, diagnostic evaluation, and treatment; and differences in the stage of disease at diagnosis (9). Race-specific differences in incidence and death rates for cervical cancer also varied by age (4). During 1992-1996, among women aged <35 years, the rate of invasive cervical cancer among black women was lower than the rate among white women. However, in older age groups, incidence rates among white women fluctuated between 13 and 15 per 100,000 women, whereas rates among black women tended to increase with age to approximately 32 per 100,000 for those aged >75 years. Among both black and white women, death rates for cervical cancer increased with advancing age; however, rates were substantially higher for black women aged >40 years than for white women the same age. Regardless of race, most cervical cancer deaths occur among women aged >50 years (4). For women in whom invasive but localized (i.e., Stage I) cervical cancer has been diagnosed, the 5-year relative survival rate is approximately 90% (4). In contrast, for women with advanced invasive cervical cancer (beyond the cervix and pelvis [i.e., Stage III and IV, respectively]), the 5-year relative survival rate is approximately 12%. As with breast cancer, diagnosis of invasive cervical cancer in black women usually occurs at a later stage of disease compared with white women. Moreover, 5-year relative survival rates for local and regional stages are lower for blacks than for whites. ETIOLOGIC FACTORSBreast CancerThe risk for breast cancer increases with advancing age. Other risk factors include personal or family history of breast cancer, history of certain benign breast diseases, early age at menarche, late age at menopause, exposure to ionizing radiation, obesity, white race, nulliparity, late age at first birth, nodular densities on mammogram, higher socioeconomic status, and residence in urban areas of the northern United States (6,10). Less clearly established risk factors include the duration between menstrual periods, use of oral contraceptives, use of replacement hormones (estrogen), height, alcohol consumption, and not breast-feeding. Studies of immigrants to the United States suggest that environmental factors rather than genetic factors are responsible for variations in breast cancer rates among countries. For example, the rate of breast cancer among first-generation JapaneseAmerican women is only slightly higher than the rate among their mothers, but the rate among their daughters is considerably higher (6). No primary prevention measures suitable for use in the general population have been established for breast cancer. Preliminary results from clinical trials among high-risk women regarding the use of the drug tamoxifen indicate a 45% decline in incidence from its use (11). Although side effects and potential development of other neoplasms are associated with tamoxifen use, other medications in its class might offer even greater benefits in breast cancer treatment. The Study of Tamoxifen and Raloxifene (STAR) trial is under way to evaluate tamoxifen versus raloxifene and the potential for reducing the incidence of breast cancer in high-risk postmenopausal women. Cervical CancerThe risk for cancer of the cervix has been associated with several factors, including infection with certain types of human papilloma virus (HPV), early age at first intercourse, multiple male sex partners, a history of sexually transmitted diseases, smoking, certain nutritional deficiencies, and low socioeconomic status (12). HPV is widely accepted as the cause of most squamous cell cervical cancers, and the sexual practices listed are well-established risk factors for the disease; however, the role of other demographic and behavioral factors is less clear. Black, Hispanic, or American Indian race/ethnicity is considered a risk factor for cervical cancer because rates of detection and death from cervical cancer are higher among these women (13). However, some of the racial/ethnic differences in cervical cancer rates can be explained by the strong inverse association between socioeconomic indicators and the risk for invasive cervical cancer (13). This increased risk could be associated with differences in access to care and cultural behavior. RECOMMENDATIONS FOR PREVENTIONBreast CancerStudies of the etiology of breast cancer have failed to identify feasible primary prevention strategies suitable for use in the general population. Many established risk factors for the disease are neither environmental nor behavioral and, therefore, are not amenable to prevention. Most of the hypothesized behavioral factors are not fully accepted as risk factors and are typically difficult to alter at the individual level. For these reasons, reducing mortality from breast cancer through early detection has become a high priority. The potential for reducing death rates from breast cancer is contingent on increasing initial and repeat mammography screening rates and subsequently detecting the disease at an early stage -- when more treatment options are available, and survival rates are higher. Mammography is the most effective method of detecting breast cancer in its earliest and most treatable stage (14). Mammography is a low-dose X-ray procedure that visualizes the internal structure of the breast to detect cancers too small to be palpated during a clinical breast examination (CBE) performed by a health-care provider. Mammography detects cancer before the woman can palpate the lump herself. Cancers de tected at a small size are more likely to be localized (i.e., not spread to regional lymph nodes or distant body sites). The sensitivity of mammography (75%-94%) is higher than comparable values for CBE alone or breast self-examination (14,15). The specificity of mammography (i.e., the likelihood that a mammogram will correctly indicate that breast cancer is not present) is also high (83%-98%) (14,15). Widespread use of this procedure, alone or with a CBE performed by a trained health-care provider, can reduce overall mortality from breast cancer (14,16). Since the 1970s, scientific studies have demonstrated that regular screening mammograms among women aged 50-69 years can reduce mortality from breast cancer by 30% (14,17-19). However, evidence is not as conclusive for women aged 40-49 years and >70 years (14). The ability of mammography to identify breast cancer at an early stage improves the opportunity for effective treatment and survival. Women in whom localized/Stage I disease has been diagnosed have a 5-year relative survival rate of 94% (4). In comparison, women with disease spread beyond regional lymph nodes have a 5-year relative survival rate of only 18.2%. Treatment at this late stage is substantially less effective, as well as more debilitating. Breast Cancer Screening Guidelines Recommended by Various GroupsAnnual breast cancer screening for women aged >50 years is widely recommended. In addition, screening is recommended for women aged 40-49 years; however, consensus has not been reached regarding the effectiveness of screening or the optimal interval for screening in this age group (20). Several review groups have reached different conclusions about the efficacy of mammography among younger women because of the limitations of studies conducted among women in this age group. These limitations include small sample sizes and limited duration of follow-up after entry into the screening programs (21). In 1996, the U.S. Preventive Services Task Force (USPSTF) recommended that women aged 50-69 years receive routine breast cancer screening every 1-2 years using mammography alone or mammography combined with annual CBE (14). USPSTF noted that insufficient evidence exists to recommend or not recommend routine mammography or CBE for women aged 40-49 years and >70 years. Moreover, insufficient evidence exists to recommend CBE alone or teaching breast self-examination. In addition, USPSTF noted that recommendations for mammography among high-risk women aged 40-49 years and among healthy women aged >70 years might be made on other grounds. In 1997, a National Institutes of Health Consensus Development Conference panel reviewed new data not previously available to USPSTF, which documented mortality benefit from mammography among women aged 40-49 years (22). However, the panel concluded that these data did not warrant a universal recommendation for mammography for women aged 40-49 years. As a result, the panel encourages these women to determine for themselves whether to receive mammography on the basis of objective analysis of scientific evidence, individual health history, and perceived risks and benefits (20). Because mortality can be reduced among women aged 40-49 years, in 1997 the National Cancer Institute (NCI) accepted new guidelines for mammography screening recommended by the presidentially appointed National Cancer Advisory Board. These guidelines recommend that all women aged >40 years receive mammography every 1-2 years to achieve the best possible outcome if breast cancer is detected (22). Prevalence of Breast Cancer ScreeningData collected through CDC's 1997 Behavioral Risk Factor Surveillance System (BRFSS) indicate that 85% of all interviewed women aged >40 years had ever received a mammogram (23). The percentage of low-income women and women without health insurance who had ever received a mammogram was comparable (77% and 69%, respectively). The percentage of all interviewed women aged >40 years who had received a mammogram within the preceding 2 years was 71%. Rates for low-income women and women without health insurance were substantially lower (58% and 50%, respectively). A Healthy People 2000 objective is to increase to at least 80% the proportion of women aged >40 years who have ever received a CBE and a mammogram, and to at least 60% those aged >50 years who have received them within the preceding 1-2 years (objective 16.11) (24). Although 1997 BRFSS data indicate the goal has been attained for all women interviewed aged >40 years who had ever received a mammogram, progress is still needed to attain the goal for low-income women and women without health insurance. Cervical CancerEffective control of cervical cancer depends primarily on early detection of precancerous lesions through use of the Pap test, followed by timely evaluation and treatment. The Pap test is probably the most successful screening test ever developed to detect a cancer. Although the efficacy of cervical cancer screening using the Pap test has not been evaluated in clinical trials, at least two factors support the positive impact of this screening test: a) evidence from many observational studies and b) the marked decline in cervical cancer incidence and death rates in the United States and other countries since the introduction of the Pap test >40 years ago (14,25). In the United States, approximately 50 million Pap tests are performed annually (26). Approximately 10% of these tests indicate an abnormality requiring further testing. Detection and treatment of precancerous cervical intraepithelial neoplasia (CIN) lesions identified by the Pap test can prevent cervical cancer. Thus, the intended outcome of cervical cancer screening differs from breast cancer screening. The primary goal of cervical cancer screening is to detect and treat CIN to prevent the occurrence of invasive cancer. For women in whom CIN lesions have been detected, the likelihood of survival is nearly 100% with appropriate evaluation, treatment, and follow-up. Cervical Cancer Screening Guidelines Recommended by Various GroupsThe American College of Obstetricians and Gynecologists (ACOG) and ACS recommend that women have a Pap test and pelvic examination when they become sexually active or at age 18 years, whichever occurs first (13). Annual Pap tests are recommended until three consecutive Pap tests are interpreted as being normal. Following this, the two groups recommend that Pap tests can be performed less frequently at the discretion of the provider (13). In 1996, USPSTF recommended routine screening for women who are or who have been sexually active and who have a uterine cervix (14). The task force recommends Pap tests with the onset of sexual activity and repeated screening every 3 years. A reduced interval between screenings can be recommended by the physician on the basis of a woman's risk factors for cervical cancer. In addition, USPSTF recommends that, on the basis of existing evidence, Pap screening might not be necessary for women after age 65 years. Moreover, USPSTF recommended not performing Pap tests on women who have undergone total hysterectomies for diseases unrelated to cervical cancer or its precursors (14). In recent years, several studies have been conducted to determine the value of expanding HPV testing from testing only women with abnormal Pap test results to routinely testing all women to detect those women at greatest risk for developing CIN or invasive cervical cancer. Evidence from these studies does not support routine HPV testing to screen for cervical cancer (26). Although new cervical cancer screening technologies have been approved for primary screening, professional organizations have not endorsed their widespread use because of concerns about cost effectiveness. An increasing concern is that rescreening the same women annually will not result in further reductions in cervical cancer mortality (27). Increased effort is needed to target groups with large proportions of unscreened or rarely screened women, including women residing in rural areas; minorities; and recent immigrants who have different attitudes, knowledge, and behaviors regarding disease prevention and health promotion. Screening for cervical cancer among these women could further reduce the burden of disease from cervical cancer. Prevalence of Cervical Cancer ScreeningThe 1997 BRFSS documented that 93% of women aged >18 years with a uterine cervix reported ever having received a Pap test (23). Corresponding values for low-income and uninsured women were 89% and 85%, respectively. Among all women with a uterine cervix, 80% had obtained a Pap test within the preceding 2 years. For low-income women and uninsured women, the proportion who had obtained a Pap test was substantially lower (69% and 65%, respectively). A Healthy People 2000 objective is to increase to at least 95% the proportion of women aged >18 years with a uterine cervix who have ever received a Pap test, and to at least 85% those who have received a Pap test within the preceding 1-3 years (objective 16.12) (24). Although 1997 BRFSS data indicate the goal for women aged >18 years with a uterine cervix who reported ever having received a Pap test is near attainment, progress is still needed, as with breast cancer screening, to attain the goal for low-income women and women without health insurance. Low income and lack of health insurance are barriers to both cervical and breast cancer screening. These factors increase the likelihood that these diseases will be diagnosed at a later stage, when survival rates are lower (1). Implementation of the National Breast and Cervical Cancer Early Detection ProgramIn August 1990, Congress enacted the Breast and Cervical Cancer Mortality Prevention Act, thereby authorizing CDC to establish a national public health infrastructure to increase breast and cervical cancer screening among low-income women who are uninsured (28). Consequently, CDC established the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), a comprehensive women's health initiative implemented through cooperative agreements with qualifying health agencies (including state and territorial health departments and American Indian/Alaska Native tribes and tribal organizations). In addition to providing breast and cervical cancer screening, participating programs provide diagnostic testing, surveillance and follow-up, case management, public education and outreach, professional education and training, quality assurance of screening tests, coalition and partnership development, and program evaluation. NBCCEDP-sponsored programs have initiated outreach efforts to serve women in high priority groups (e.g., women with increased risk for breast or cervical cancer and women who do not or rarely access breast and cervical cancer screening), including older women, racial/ethnic minorities, foreign-born women, women with disabilities, lesbians, and women residing in rural or other hard-to-reach areas. Fiscal year (FY) 2000 marked the 10th year of the NBCCEDP, with Congressional appropriations of $167 million. CDC provides funds to all 50 states, six U.S. territories, the District of Columbia, and 15 American Indian/Alaska Native tribes and tribal organizations to implement comprehensive screening programs for breast and cervical cancer (29). During the reporting period July 1991-March 1999, approximately 2.2 million screenings for breast and cervical cancer were provided to uninsured women. The program supported 1,049,752 mammograms: 64% of the mammograms were provided to women aged >50 years; 48% were provided to racial/ethnic minorities (Figure 3). Breast cancer was diagnosed in 6,265 women aged >40 years. Although the rate of abnormalities detected by a mammogram was highest for younger women, the rate of breast cancers detected per 100,000 mammograms increased directly with advancing age (Figure 4). A total of 1,192,346 Pap tests were performed: 72% of the tests were provided to women aged >40 years; 47% were provided to racial/ethnic minorities (Figure 5). Cervical intraepithelial neoplasia was detected in 34,046 women. Invasive cervical cancer was diagnosed in 561 women. The rate of abnormal Pap tests varied inversely with age. Policy of NBCCEDPAs NBCCEDP has evolved, the program has addressed many challenges, especially regarding screening recommendations and treatment resources for women in whom precancerous cervical lesions or cancer of the breast or cervix has been diagnosed through NBCCEDP. FY 2000 Congressional appropriations will enable NBCCEDP to screen approximately 12%-15% of the eligible uninsured women aged 50-64 years in the United States (30). The remaining unmet need and the absence of funding to cover treatment expenses for women who have received a diagnosis of precancerous cervical lesions or breast or cervical cancer have been persistent challenges to the program. A key public health priority of NBCCEDP is to direct program resources to eligible women who have rarely or have never received breast or cervical cancer screening. To address this priority and maximize efficient use of limited resources, the program has developed cancer-control policies on the basis of programmatic data, current scientific research, and availability of screening services through other government-supported programs (e.g., Medicare and Title X Family Planning programs). Breast Cancer Screening PoliciesFollowing implementation of NBCCEDP in 1991, CDC encouraged NBCCEDP- sponsored programs to place a high priority on screening women aged >50 years. NBCCEDP data indicated that only 57% of their mammograms were provided to women aged >50 years. In October 1994, CDC established the first age-specific targets for the breast cancer screening component of NBCCEDP. For 1995, 75% of the mammograms were to be provided to women aged >50 years. The percentage was gradually increased to 90% by October 1998. A review of NBCCEDP mammography screening data in 12-month intervals indicated that, since 1994, programs had screened increasing numbers of women aged >50 years for breast cancer; however, the age-specific percentage goals had not been attained. For example, the percentage of initial mammograms provided to women aged >50 years for the reporting period October 1996-September 1997 was 74%. In 1998, NBCCEDP mammogram screening policy was revised in response to new scientific research, recent changes in recommendations by NCI and ACS, changes in Medicare preventive services coverage, and the need to establish a more realistic national target based on historical programmatic screening data. The new NBCCEDP policy is to provide at least 75% of mammograms to women aged >50 years who are not eligible to receive Medicare Part B benefits or are unable to pay the premium to enroll in Medicare Part B. Correspondingly, no more than 25% of mammograms should be provided to women aged <50 years. As a result of this new policy, some participating health agencies have developed strategies to cover breast cancer screening for women aged 40-49 years. Several programs have obtained breast cancer screening resources for these women from state appropriations or tobacco tax revenues and through collaborative efforts with foundations (e.g., the Susan G. Komen Breast Cancer Foundation). During October 1997-September 1998, 75% of NBCCEDP-sponsored mammograms were provided to women aged >50 years. Cervical Cancer Screening PoliciesThe primary purpose of the cervical cancer component of NBCCEDP is to identify and treat precancerous cervical lesions and to detect and treat invasive cervical cancer at an early stage. When the program was established in 1991, CDC implemented program guidelines for cervical cancer screening that were consistent with ACS guidelines. Women enrolled in NBCCEDP who were aged >18 years, with an intact uterine cervix, were eligible for an annual Pap test and pelvic examination. After a woman has had three consecutive annual examinations with normal findings, Pap tests could be performed less frequently at the discretion of the woman and her health-care provider. In 1999, CDC, in consultation with an external work group comprising clinical experts, epidemiologists, and public health practitioners, reexamined NBCCEDP's cervical cancer screening policy and other emerging issues related to Pap testing. One of the key issues addressed by this work group was recommendations for Pap screening intervals. ACOG's and ACS's recommendations regarding the frequency of screening are similar and advise that after a woman has had three consecutive annual examinations with normal findings, the Pap test can be performed less frequently at the discretion of the woman's provider. Scientific data suggest that once a woman has demonstrated no signs of CIN, as evidenced by three consecutive annual Pap tests with normal findings, her chance of developing CIN II or worse within a 3-year period is extremely low, regardless of other risk factors (31). Preliminary analysis of NBCCEDP data supports these findings (CDC, unpublished data, 2000). Beginning in March 2000, NBCCEDP-sponsored programs will be required to direct more cervical cancer screening resources to women who have never had a Pap test or who have not had a Pap test for at least 5 years. Among all women screened, at least 20% should be women who have either never been screened or have rarely been screened (i.e., not screened for >5 years). Programs are also being required to reduce over-screening among program-enrolled women. Beginning in October 2001, programs will be required to document that at least 75% of women with three consecutive annual Pap tests with normal findings did not receive a fourth annual Pap test. Their screening interval will be changed to every 3 years. To successfully implement this policy change, CDC will assist NBCCEDP-sponsored programs in assessing current program provider practices, modifying patient recall systems, and developing professional and public education strategies. Breast and Cervical Cancer Follow-Up and Treatment PolicyThe policy issue that has caused the greatest controversy in NBCCEDP concerns the availability of funds to pay for treatment of cancerous or precancerous lesions diagnosed in enrolled women (28). A crucial component of NBCCEDP is to ensure that all women with abnormal screening results, precancerous breast or cervical lesions, or a diagnosis of cancer receive timely and appropriate follow-up care. Program providers receive reimbursement for most diagnostic procedures, including diagnostic mammography, breast ultrasound, fine-needle aspiration of the breast, breast and cervical biopsies, and colposcopy of the cervix. However, the Breast and Cervical Cancer Mortality Prevention Act of 1990 prohibits use of federal program funds for any component of breast or cervical cancer treatment primarily because of a concern that such payment would rapidly deplete resources available for screening services. NBCCEDP-sponsored programs are required to identify and secure resources for treatment from other sources. In 1996, CDC conducted in-depth case studies of seven state programs to determine how early detection programs identified and obtained resources for treatment. The results indicated that state health agencies and their partners had developed a wide range of strategies for procuring treatment services in the absence of program resources. However, the study respondents considered the strategies used to obtain these services as short-term solutions that were labor intensive and that diverted resources away from screening activities (32). NBCCEDP surveillance data for October 1991September 1998 indicate that 92% of the clients in whom breast cancer had been diagnosed and 93% of the clients in whom invasive cervical cancer had been diagnosed initiated treatment. The remainder either refused treatment, were lost to follow-up, or had an outcome pending. In FY 1999, CDC received increased Congressional appropriations to expand case-management activities to assist women in overcoming financial, logistical, and other barriers to obtaining these services. Recommended Priority Activities for CDCThe Breast and Cervical Cancer Mortality Prevention Act of 1990 has played an important role in focusing public health efforts on cancer control in the United States. Since 1991, CDC has collaborated with a diverse group of public and private partners to build the public health infrastructure, implement screening services, and conduct research activities. CDC will continue to foster these relationships to achieve goals set in the following four priority areas of screening initiatives, case-management services, professional education and training, and partnerships: Screening Initiatives
Case-Management Services
Professional Education and Training
Partnerships
RESEARCH AGENDATo support the recommended priority activities for NBCCEDP, CDC has developed a research agenda comprising six priorities. This research will assist in improving cancer screening services provided to women enrolled in NBCCEDP and in developing new methods to recruit eligible women who have rarely or have never received breast or cervical cancer screening.
CONCLUSIONBreast and cervical cancer continue to be major health problems in the United States. Preventive measures are available to reduce morbidity and mortality associated with these diseases. The NBCCEDP, through federal, state, territorial, and tribal governments, in collaboration with national and community-based organizations, has increased access to breast and cervical cancer screening among low-income and uninsured women. In addition, NBCCEDP-sponsored programs have increased the staff working in cancer control and the expertise of these persons, implemented professional education programs for health-care providers, and developed innovative public education and outreach strategies to encourage medically underserved women to seek screening services. This national effort enabled the United States to make substantial progress toward achieving the Healthy People 2000 objectives for breast and cervical cancer control, particularly among racial/ethnic minorities and the medically underserved. However, NBCCEDP still reaches only 12%-15% of uninsured women aged 50-64 years who are eligible for screening services. A continuing challenge for the future is to increase national commitment to providing screening services for all eligible uninsured women to ultimately reduce morbidity and mortality from breast and cervical cancer. References
* Defined as up to 250% of poverty level depending, on family size. † In 1996, the SEER program comprised cases from 11 population-based cancer registries throughout the United States that represent an estimated 13.9% of the U.S. population. The SEER program also publishes death rates based on a public-use data tape from CDC's National Center for Health Statistics. During 1988-1996, the 11 locations were Connecticut; Hawaii; Iowa; New Mexico; Utah; and Atlanta, Detroit, San Francisco/Oakland, San Jose/Monterey, Los Angeles, and Seattle/Puget Sound. Figure 1 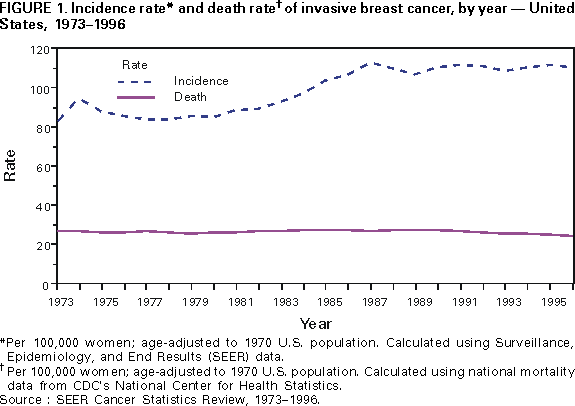 Return to top. Figure 2 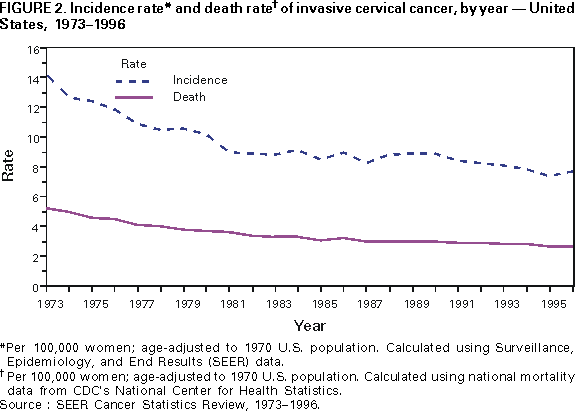 Return to top. Figure 3 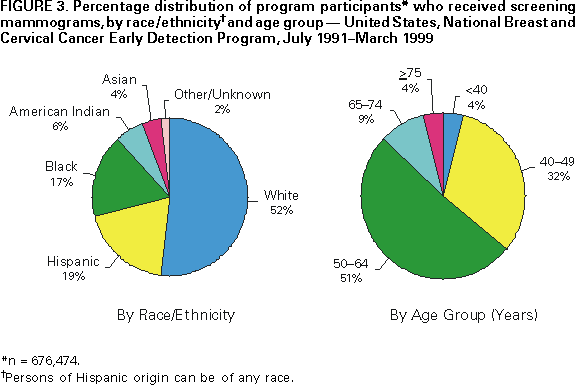 Return to top. Figure 4 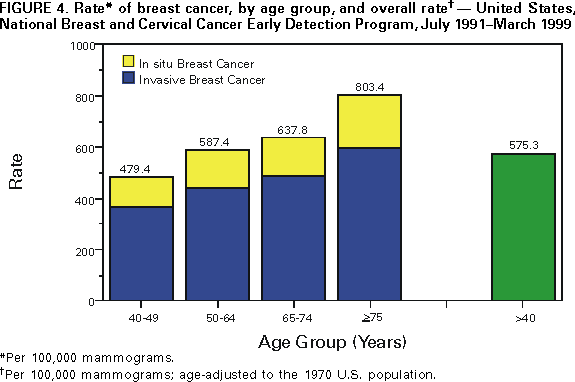 Return to top. Figure 5 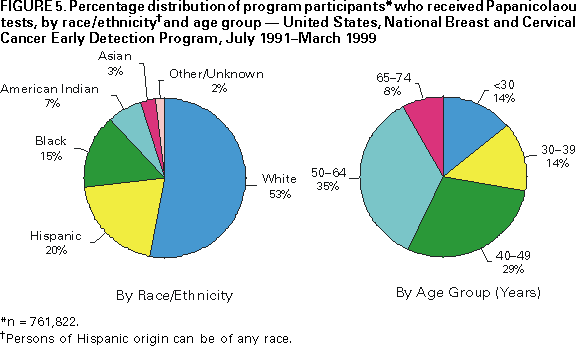 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 3/28/2000 |
|||||||||
This page last reviewed 5/2/01
|