 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Guidelines for School Programs To Prevent Skin CancerPrepared by The material in this report was prepared for publication by the National Center for Chronic Disease Prevention and Health Promotion, James S. Marks, M.D., M.P.H., Director; the Division of Cancer Prevention and Control, Nancy C. Lee, M.D., Director; and the Division of Adolescent and School Health, Lloyd J. Kolbe, Ph.D., Director. SummarySkin cancer is the most common type of cancer in the United States. Since 1973, new cases of the most serious form of skin cancer, melanoma, have increased approximately 150%. During the same period, deaths from melanoma have increased approximately 44%. Approximately 65%--90% of melanomas are caused by ultraviolet (UV) radiation. More than one half of a person's lifetime UV exposure occurs during childhood and adolescence because of more opportunities and time for exposure. Exposure to UV radiation during childhood plays a role in the future development of skin cancer. Persons with a history of >1 blistering sunburns during childhood or adolescence are two times as likely to develop melanoma than those who did not have such exposures. Studies indicate that protection from UV exposure during childhood and adolescence reduces the risk for skin cancer. These studies support the need to protect young persons from the sun beginning at an early age. School staff can play a major role in protecting children and adolescents from UV exposure and the future development of skin cancer by instituting policies, environmental changes, and educational programs that can reduce skin cancer risks among young persons. This report reviews scientific literature regarding the rates, trends, causes, and prevention of skin cancer and presents guidelines for schools to implement a comprehensive approach to preventing skin cancer. Based on a review of research, theory, and current practice, these guidelines were developed by CDC in collaboration with specialists in dermatology, pediatrics, public health, and education; national, federal, state, and voluntary agencies; schools; and other organizations. Recommendations are included for schools to reduce skin cancer risks through policies; creation of physical, social, and organizational environments that facilitate protection from UV rays; education of young persons; professional development of staff; involvement of families; health services; and program evaluation. IntroductionSkin cancer is the most common type of cancer in the United States (1). Since 1973, the number of new cases of melanoma, the skin cancer with the highest risk for mortality and one of the most common cancers among young adults, has increased. The incidence of melanoma has increased 150%, and melanoma mortality rates have increased by 44% (1). Because a substantial percentage of lifetime sun exposure occurs before age 20 years (2,3) and because ultraviolet (UV) radiation exposure during childhood and adolescence plays an important role in the development of skin cancer (2,4), preventive behaviors can yield the most positive effects, if they are initiated early and established as healthy and consistent patterns throughout life. Children spend several hours at school on most weekdays, and some of that time is spent in outdoor activities. Schools, therefore, are in a position to teach and model healthy behaviors, and they can use health education activities involving families to encourage sun-safe behaviors at home. Thus, schools can play a vital role in preventing skin cancer. This report is one of a series of guidelines produced by CDC to help schools improve the health of young persons by promoting behaviors to prevent the leading causes of illness and death (5--8). The primary audience for this report includes state and local health and educational agencies and nongovernmental organizations concerned with improving the health of U.S. students. These agencies and organizations can translate the information in this report into materials and training programs for their constituents. In addition, CDC will develop and disseminate materials to help schools and school districts implement the guidelines. At the local level, teachers and other school personnel, community recreation program personnel, health service providers, community leaders, policymakers, and parents may use these guidelines and complementary materials to plan and implement skin cancer prevention policies and programs. In addition, faculty at institutions of higher education may use these guidelines to train professionals in education, public health, sports and recreation, school psychology, nursing, medicine, and other appropriate disciplines. Although these skin cancer prevention guidelines are intended for schools, they can also guide child care facilities and other organizations that provide opportunities for children and adolescents to spend time in outdoor settings (e.g., camps; sports fields; playgrounds; swimming, tennis, and boating clubs; farms; and recreation and park facilities). These guidelines address children and adolescents of primary- and secondary-school age (approximately 5--18 years). The recommendations are based on scientific evidence, medical and behavioral knowledge, and consensus among specialists in education and skin cancer prevention. In 2003, CDC will publish a chapter on cancer in its Community Guide to Preventive Services (9), which will summarize information regarding the effectiveness of community-based interventions geared toward preventing skin cancer. School-based programs can play an important role in achieving the following national Health Objectives for the Year 2010 related to skin cancer prevention: 1) increase the proportion of persons who use at least one of the following protective measures that might reduce the risk for skin cancer: avoid the sun between 10 a.m. and 4 p.m., wear sun-protective clothing when exposed to the sun, use sunscreen with a sun-protection factor (SPF) >15, and avoid artificial sources of UV light; and 2) reduce deaths from melanoma to <2.5 per 100,000 persons (10). Burden of Skin CancerSkin cancer is the most common type of cancer in the United States (11). The two most common kinds of skin cancer --- basal cell carcinoma and squamous cell carcinoma --- are highly curable. However, melanoma, the third most common type of skin cancer and one of the most common cancers among young adults, is more dangerous. In 2001, approximately 1.3 million new cases of basal cell or squamous cell carcinoma were diagnosed with approximately 2,000 deaths from basal cell and squamous cell carcinoma combined. Melanoma, by contrast, will be diagnosed in 53,600 persons and will account for 7,400 deaths, more than three fourths of all skin cancer deaths (12). Basal cell carcinoma, which accounts for 75% of all skin cancers (11), rarely metastasizes to other organs. Squamous cell carcinoma, which accounts for 20% of all skin cancers, has a higher likelihood of spreading to the lymph nodes and internal organs and causing death (13), but these outcomes are also rare. Melanoma is nearly always curable in its early stages, but it is most likely to spread to other parts of the body if detected late. Melanoma most often appears on the trunk of men and the lower legs of women, although it also might be found on the head, neck, or elsewhere (14,15). In the United States, diagnoses of new melanomas are increasing, whereas diagnoses of the majority of other cancers are decreasing (16). Since 1973, the annual incidence rate for melanoma (new cases diagnosed per 100,000 persons) has more than doubled, from 5.7 cases per 100,000 in that year to 14.3 per 100,000 in 1998 (1) (Figure). The rapid increase in annual incidence rates is likely a result of several factors, including increased exposure to UV radiation and possibly earlier detection of melanoma (17). Since 1973, annual deaths per 100,000 persons from melanoma have increased by approximately 44%, from 1.6 to 2.3 (Figure). However, over the course of the 1990s, mortality rates have remained stable, particularly among women (16,18--19). Although doctors must report other types of cancer (including melanomas) to cancer registries, they are not required to report squamous or basal cell cancer, which makes tracking trends in the incidence of these two cancers difficult. However, death rates for basal cell and squamous cell carcinoma have remained stable (12). Risk Factors for Skin CancerExcessive Exposure to UV Radiation Skin cancer is largely preventable by limiting exposure to the primary source of UV radiation, sunlight. Sunlamps and tanning beds are other sources. Persons with high levels of exposure to UV radiation are at an increased risk for all three major forms of skin cancer. Approximately 65%--90% of melanomas are caused by UV exposure (20). The epidemiology implicating UV exposure as a cause of melanoma is further supported by biologic evidence that damage caused by UV radiation, particularly damage to DNA, plays a central role in the development of melanoma (4). Total UV exposure depends on the intensity of the light, duration of skin exposure, and whether the skin was protected by sun-protective clothing and sunscreen. Severe, blistering sunburns are associated with an increased risk for both melanoma and basal cell carcinoma. For these cancers, intermittent intense exposures seem to carry higher risk than do lower level, chronic, or cumulative exposures, even if the total UV dose is the same. In contrast, the risk for squamous cell carcinoma is strongly associated with chronic UV exposure but not with intermittent exposure. The two most important types of UV radiation, UV-A and UV-B radiation, have both been linked to the development of skin cancer. UV-A rays are not absorbed by the ozone layer, penetrate deeply into the skin, and cause premature aging and possibly suppression of the immune system (4,21,22). Up to 90% of the visible changes commonly attributable to aging are caused by sun exposure. UV-B rays, which are partially absorbed by the ozone layer, tan and sometimes burn the skin. UV-B radiation has been linked to the development of cataracts (23--25) and skin cancer. Recommended skin cancer prevention measures protect against both UV-A and UV-B radiation. Childhood and Adolescent UV Exposure Exposure to UV radiation during childhood and adolescence plays a role in the future development of both melanoma and basal cell cancer (26--32). For example, the risk for developing melanoma is related strongly to a history of >1 sunburns (an indicator of intense UV exposure) in childhood or adolescence (27,28,33,34). Similarly, sunburns during these periods have been demonstrated to increase the risk for basal cell carcinoma (30,31). Childhood is the most important time for developing moles, which is an important risk factor for skin cancer. Sun exposure in childhood might increase the risk for melanoma by increasing the number of moles (33). A study supports the use of sun protection during childhood to reduce the risk for melanoma in adulthood (35). Children and adolescents have more opportunities and time than adults to be exposed to sunlight (36--38) and thus more opportunities for development of skin cancer (4,39,40). More than one half of a person's lifetime UV exposure occurs during childhood and adolescence (3,41). Skin Color and Ethnicity Although anyone can get skin cancer, persons with certain characteristics are particularly at risk. For example, the incidence of melanoma among whites is approximately 20 times higher than among blacks (1). Hispanics appear to be at less risk for melanoma than whites; a study conducted in Los Angeles, California, indicated that the incidence rates for Hispanics were 2--3 per 100,000, whereas the rate for non-Hispanic whites was 11 per 100,000 (42). For basal cell and squamous cell carcinoma, rates among blacks are 1/80 of the rates among whites (43). The ethnic differences in observed rates are attributable mostly to skin color. The color of the skin is determined by the amount of melanin produced by melanocytes, which also protect the skin from the damage produced by UV radiation. Although darkly pigmented persons develop skin cancer on sun-exposed sites at lower rates than lightly pigmented persons, UV exposure increases their risk for developing skin cancer (44). The risk for skin cancer is higher among persons who sunburn readily and tan poorly (45), namely those with red or blond hair, and fair skin that freckles or burns easily (14,46,47). Moles The most measurable predictors of melanoma are having large numbers and unusual types of moles (nevi) (48,49). Usually not present at birth, moles begin appearing during childhood and adolescence and are associated with sun exposure. Most moles are harmless but some undergo abnormal changes and become melanomas. A changing mole, particularly in an adult, is often indicative of the development of melanoma (45). Family History The risk for melanoma increases if a person has >1 first-degree relatives (i.e., mother, father, brother, and sister) with the disease. Depending on the number of affected relatives, the risk can be up to eight times that of persons without a family history of melanoma. Nonetheless, only approximately 10% of all persons with melanoma have a family history of melanoma (45,50). Age The incidence of skin cancer increases exponentially with age because older persons have had more opportunities to be exposed to UV radiation and they have diminished capacity to repair the damage from UV radiation (4,14,43). Approximately one half of all melanomas occur in persons aged <50 years. Melanoma is one of the most common cancers found in persons aged <30 years (14); it is the most common cancer occurring among persons in the 25--29 age group and the third most common in the 20--24 age group (51). Environmental Factors Affecting UV Radiation Environmental factors that increase the amount of UV radiation exposure received by humans include a latitude closer to the equator; higher altitude; light cloud coverage (allows 80% of UV rays to go through the clouds); the presence of materials that reflect the sun (e.g. pavement, water, snow, and sand); being outside near noontime (UV-B radiation is highest in the middle of the day and varies more by time of day than does UV-A); and being outside during the spring or summer (21,52). Ozone depletion could potentially increase levels of solar radiation at the earth's surface (53,54). Artificial UV Radiation In 2000, the National Institute of Environmental Health Sciences concluded that sunlamps and tanning beds are carcinogenic (55). Although limited, epidemiologic evidence suggests that a causal relation exists between artificial UV radiation and melanoma (55,56). The type and amount of UV radiation emitted from some sunbeds appear to be similar to that of noontime summer sun, and in some cases, the amount is even higher than the sun would emit (57). Artificial UV radiation can substantially damage the skin (i.e., cause sunburn) and has been linked to ocular melanoma (52,58). Sunlamps and tanning beds should be avoided. Protective BehaviorsOptions for skin cancer prevention (Box 1) include limiting or minimizing exposure to the sun during peak hours (10 a.m.--4 p.m.), especially the 1-hour period closest to the noon hour (11 a.m.--1:00 p.m. when the UV rays are the strongest), wearing sun-protective clothing, using sunscreens that have UV-A and UV-B protection, and avoiding sunlamps and tanning beds. Most medical and cancer organizations advocate the use of similar skin cancer prevention measures (59). The American Cancer Society (60), the American Academy of Dermatology (61,62), the American Academy of Pediatrics (63), the American Medical Association (64), and the National Cancer Institute (65) all recommend patient education on UV radiation avoidance and sunscreen use. The third U.S. Preventive Services Task Force is revising their guidelines on provider counseling for skin cancer prevention and sunscreen use. Avoiding the Sun and Wearing Proper Clothing and Sunglasses Some forms of protection (e.g., avoiding the sun, seeking shade, and wearing sun-protective clothing) are the first approach toward preventing skin cancer. One study has demonstrated that wearing sun-protective clothing can decrease the number of moles (66); another study demonstrated that the protective effect of clothing depends primarily on the construction of the fabric (a tighter weave permits less UV radiation to reach the skin) (67). Other important factors include fiber type (natural cotton or Lycra™ transmits less UV radiation than bleached cotton) and color (darker colors transmit less UV radiation); additional factors include whether the fabric is wet or stretched (transmission of UV radiation increases as the fabric becomes more wet and stretched) (68). Wide-brimmed hats (>3-inch brim) and Legionnaire hats (baseball type of hat with attached ear and neck flaps) provide the best protection for the head, ears, nose, and cheeks (69). In 2001, the Federal Trade Commission and the Consumer Safety Product Commission assisted in the development of voluntary industry standards in the United States for rating the UV protective value of different types of clothing and of shade structures (70). These standards should help the public make informed decisions concerning protection against UV radiation (68,71). Sunglasses protect the eyes and surrounding areas from UV damage and skin cancer. Although no federal regulations exist for sunglasses, the American Academy of Ophthalmology recommends that sunglasses block 99% of UV-A and UV-B radiation. A chemical coating applied to the surface of the lens is the protective mechanism; protection does not correlate with the color or darkness of the lens (72). Sunglasses can reduce UV radiation exposure to the eye by 80%, and when combined with a wide-brimmed hat or Legionnaire hat, UV exposure to the face is reduced by 65% (73). Shade structures and trees can reduce direct UV radiation, but the protection offered is dependent on the direct and indirect UV radiation from the surrounding surface (e.g., sand and concrete) (74,75). For example, umbrellas with more overhang provide more UV protection than those with less overhang. Sunscreens Sunscreens are an important adjunct to other types of protection against UV exposure. Using sunscreen is one of the most commonly practiced behaviors for preventing skin cancer. During the previous decade, new studies have contributed to an increased understanding of the role of sunscreen in possibly preventing skin cancer. The U.S. Preventive Services Task Force is revising their recommendations on sunscreen use, but the International Agency for Research on Cancer has concluded that topical use of sunscreens probably prevents squamous cell carcinoma of the skin. The group drew no conclusions regarding whether the use of sunscreens reduces the incidence of basal cell carcinoma or melanoma (76) (Appendix A). Clinical trials have demonstrated that sunscreens are effective in reducing the incidence of actinic keratoses, the precursors to squamous cell carcinoma (77,78). One randomized clinical trial demonstrated that sunscreens are effective in reducing squamous cell carcinoma itself (79). Another randomized trial demonstrated that, among children who are at high risk for developing melanoma, sunscreens are effective in reducing moles, the precursors and strongest risk factor for melanoma (80). Unfortunately, many persons use sunscreens if they intend to stay out in the sun longer, and they reduce the use of other forms of sun protection (e.g., clothing or hats), thereby, acquiring the same or even a higher amount of UV radiation exposure than they would have obtained with a shorter stay and no sunscreen (22,76,81). The guidelines in this report recommend 1) using various methods (e.g., avoiding the sun, seeking shade, or wearing protective clothing) that reduce exposure to the full spectrum of UV radiation as the first line of protection against skin cancer and 2) using sunscreen as a complementary measure. In some instances, sunscreens might be the only responsible option. However, to be effective, sunscreens must be applied correctly (Appendix B). For example, users should apply sunscreen and allow it to dry before going outdoors and getting any UV exposure (82,83). Similarly, users should reapply sunscreen after leaving the water, sweating, or drying off with a towel. Use of insufficient quantities of sunscreen (84,85) or use of a sunscreen with insufficient protection are other concerns. Manufacturers determine the SPF (a measure of protection from only UV-B radiation) by applying an adequate amount of sunscreen (1--2 ounces) on humans and testing under artificial light, which is usually not as strong as natural light (86). No government standards measure how much protection sunscreens provide against UV-A rays. Few studies have been conducted on sunscreens, despite their widespread use, which make it difficult to estimate the prevalence of allergies to sunscreens. Skin irritation, rather than an actual allergic reaction, is one of the more commonly reported adverse events (87). Because the majority of the commercially available sunscreens are a combination of agents from various chemical groups, persons who might experience adverse effects should be aware of the active ingredients and try sunscreens with different ingredients. In previous years, the most commonly reported allergen was para-aminobenzoic acid (PABA) (rarely used today), whereas the current two most frequently cited allergens are benzophenone-3 and dibenzoyl methanes (22). Prevalence of Behavioral Risk Factors, Sun-Safe Behaviors, and Attitudes Related to Sun Safety In the United States, sunbathing and tanning habits were established during the early to mid-1900s (88,89), most likely reflecting the increased availability of leisure time and fashion trends promoting tanned skin (89,90). In the late 1970s, the majority of the population had little knowledge concerning their personal susceptibility to skin cancer and believed that tanning enhanced appearance and was associated with better health (91). More recent reports indicate that many Americans feel healthier with a tan and believe that suntanned skin is more attractive (36,92,93). In 1992, 53% of U.S. adults were "very likely" to protect themselves from the sun by practicing at least one protective behavior (using sunscreen, seeking shade, or wearing sun-protective clothing) (94). Among white adults, approximately one third used sunscreen (32%), sought shade (30%), and wore protective clothing (28%). Among black adults, 45% sought shade, 28% wore sun-protective clothing, and 9% used sunscreen (95). Sun-protective behaviors were more common among the more sun sensitive, females, and older age groups among both whites and blacks. Sun-safety behaviors might be most difficult to change among preadolescents and adolescents (96). Teenagers spend a substantial amount of time outdoors, especially on weekends and during the summer (97,98). Many teenagers believe that a tan is desirable (92); only teenagers who know persons with skin cancer or who perceive an increased personal susceptibility to skin cancer are more likely to use sunscreen (98). However, teenagers who practice skin cancer prevention tend to only use sunscreen and to use it infrequently, inconsistently, and incorrectly (97,98). Girls tend to use sunscreen more than boys, but they also use tanning beds more frequently (97--101). Sunscreen use by children is correlated positively with use by their parents (87,102). Some parents know the risks of skin cancer but do not realize that children are at risk (103,104). Some parents believe that a suntan is a sign of good health; others use sunscreen on their children as their only or preferred skin cancer prevention measure (36,99,105--107), even though other measures (e.g., using shade structures and wearing sun-protective clothing) are available. Sometimes parents apply sunscreen on their children incorrectly and inconsistently (22) (e.g., only after a child has experienced a painful sunburn) (97,108). Concerns Regarding Promoting Protection from UV RadiationSun-safety measures should not reduce student participation in physical activity. Regular physical activity reduces morbidity and mortality for multiple chronic diseases. Promoting lifelong physical activity in schools is a critically important public health and educational priority (8). Schools might find it difficult to avoid scheduling outdoor physical activity programs around the midday hours. These schools can focus their efforts on other sun-safety measures (e.g., seeking shade; and wearing a hat, protective clothing, or sunscreen), which can be implemented without compromising physical activity while gradually making feasible scheduling changes. In addition, because UV radiation plays a role in the synthesis of vitamin D, the limitation of UV exposure might be of some concern. This limitation might lead to a decrease in levels of vitamin D and increase the likelihood that rickets, a disorder involving a weakening of the bones, will develop in susceptible infants and children. However, the average age for presentation of rickets is 18 months, and the age groups of concern are typically infants and toddlers, not school-aged children between 5 and 18 years. Although the major source of vitamin D is through skin exposure to sunlight, supplementing the diet with foods (e.g., flesh of fatty fish, eggs from hens fed vitamin D, and vitamin D-fortified milk and breakfast cereal) can provide enough vitamin D to meet adequate intake requirements (109,110). The American Academy of Pediatrics (111) recommends vitamin D supplementation for breast-fed infants whose mothers are vitamin D deficient or for infants who are not exposed to adequate sunlight. Infants consuming at least 500ml of vitamin D-fortified formula per day and older children consuming at least 16 ounces of vitamin D-fortified milk per day will meet the adequate intake of vitamin D. Guidelines for School Programs To Prevent Skin CancerSchools as Settings for Skin Cancer Prevention EffortsEpidemiologic data suggest that several skin cancers can be prevented if children and adolescents are protected from UV radiation (26--32). Schools can participate in reducing exposure of young persons to UV radiation from the sun during school-related activities by offering education and skill-building activities to reinforce the development of healthful behaviors. School-based efforts to prevent skin cancer can be more effective in the framework of a coordinated school health program (112,113) that includes family and community participation (114) and builds on the context and current practices in the school and community. Coordinated school health programs aim to create and support environments where young persons can gain the knowledge, attitudes, and skills required to make and maintain healthy choices and habits. These programs integrate health education, a healthy school environment, physical education, nutrition services, health services, mental health and counseling services, health promotion programs for faculty and staff, and efforts to integrate school activities with family and community life (113). Being aware of existing practices for sun exposure and sun protection among teachers, staff, and students might help define gaps in optimal sun-safety practices. Careful observations for a few days might also provide important information concerning students' use of shade areas and sunscreen at recess or lunch time, and staff's use of hats, shirts, and sunglasses. Discussions with students and staff who practice sun-safe behaviors might prove useful in planning and improving implementation of sun-safety practices. Skin cancer prevention measures vary in both their ease of adoption and relevance. Schools should not allow an "all or nothing" approach to undermine the effectiveness of their skin cancer prevention efforts. For sun-safety protection, a short-sleeve shirt and cap might be better than no hat and a sleeveless top. Being flexible is important while moving in the direction of optimal skin cancer prevention environments, policies, and programs. Skin Cancer Prevention GuidelinesThese guidelines provide recommendations for skin cancer prevention activities within a coordinated school health program. In addition, these guidelines are based on scientific literature, national policy documents, current practice, and theories and principles of health behavioral change (115). Schools and community organizations can work together to develop plans that are relevant and achievable. Sustained support from school staff, students, communities, state and local education and health agencies, families, institutions of higher education, and national organizations are necessary to ensure the effectiveness of school skin cancer prevention activities (116). In this report, seven broad guidelines are included that school programs can use to reduce the risk for skin cancer among students: 1) policy, 2) environmental change, 3) education, 4) families, 5) professional development, 6) health services, and 7) evaluation (Box 2). Each guideline includes suggestions regarding key elements, steps for implementation, and realistic expectations for change.
The recommendations represent the state-of-the-science in school-based skin cancer prevention. However, every recommendation is not appropriate or feasible for every school to implement nor should any school be expected to implement all recommendations. Schools should determine which recommendations have the highest priority based on the needs of the school and available resources. As more resources become available, schools could implement additional recommendations to support a coordinated approach to preventing skin cancer. Guideline 1: Policy --- Establish Policies that Reduce Exposure to UV Radiation.Policies can provide sun protection for all persons in a defined population (e.g., a school), not just those who are most motivated (117). In addition, policies can involve formal organizational rules and standards or legal requirements and restrictions related to skin cancer prevention measures. Policies may be developed by a school, school board, or by other legal entities (e.g., municipal, state, and federal governments). To be effective, policies need to be communicated to school personnel, announced to affected constituents (e.g., students and their parents), managed and implemented, enforced and monitored, and reviewed periodically (118,119). Before establishing healthy skin cancer prevention policies, identify any existing policies that might deter skin cancer prevention. These existing policies might include outdoor activity schedules, prohibitions on wearing sunglasses or caps and hats at school, and rules that limit the use or provision of sunscreen at school (e.g., requiring parental permission, defining sunscreen as "medicine", and restricting teachers from applying sunscreen on children). California enacted a law (effective January 2002) that requires their schools to allow students, when outdoors, to wear school-site approved sun-protective hats and clothing. This legislation was deemed necessary because several school districts had banned hats because some styles or colors are connected with gang affiliation. An effectively crafted skin cancer prevention policy provides a framework for implementing the other six guidelines. The policy demonstrates institutional commitment and guides school and community groups in planning, implementing, and evaluating skin cancer prevention activities. Such a policy creates a supportive environment for students to learn about and adopt sun-protection practices. Although a comprehensive policy is preferable, more limited policies addressing certain aspects of skin cancer prevention also can be useful. Developing the Policy or Policies Skin cancer prevention can be part of a larger school health policy. Although policies might be initiated by a person or small group, the most effective policies are developed with input from all relevant constituents. In schools, the constituents include students, teachers, parents, administrators, coaches, school nurses, health educators and other relevant personnel as well as community leaders and residents. Schools can also work with community partners (e.g., recreation and parks departments, health departments, after-school programs, camps, families, and youth advocacy groups) and others who organize outdoor activities for youth. Policies require time for development and implementation and might not be as visible as educational programs (120). Increased effort in the early stages of policy development might result in increased adoption (121). In Australia, health and cancer prevention specialists developed a sun-protection policy kit for schools and a related staff development module (120). Elementary schools were twice as likely to formally adopt a comprehensive sun-protection policy if they also received the staff development module (44% [kit and module] versus 21% [kit only]). However, few high schools adopted policies whether they received just the kit or the kit and the module (11% and 6%, respectively) (120). Policy development requires a long-term commitment and sustained efforts and cooperation among all concerned parties. Policy Options Components of skin cancer prevention policies for a school or community to consider include 1) statement of purpose and goals; 2) schedule and physical environment policies; 3) policies related to personal protective clothing and sunglasses; 4) sunscreen policies; 5) education policies; 6) policies on outreach to families; and 7) policies on resource allocation and evaluation. When implementing a comprehensive policy (which would include all of these components) is not feasible, schools can start with some of these components and add others over time. Policy 1: Statement of Purpose and Goals. Policies usually begin with a statement of purpose and goals that establish sun safety as a priority and highlight the importance of skin cancer prevention. In addition, the statement can 1) describe the influence of childhood sun exposure on the risk for developing skin cancer later in life; 2) identify actions that persons and institutions can take to reduce the risk for skin cancer; 3) highlight the importance of establishing a physical, social, and organizational environment that supports skin cancer prevention; and 4) specify dedicated financial and human resources for skin cancer prevention and for the other policy options described here. Policy 2: Schedule and Structure Policies. Policies can provide the basis for across-the-board reduction of UV radiation exposure for children and adults in schools and communities by establishing 1) rules that encourage the scheduling of outdoor activities (including athletic and sporting events) during times when the sun is not at its peak intensity and 2) building and grounds codes to increase the availability of shade in frequently used outdoor spaces. Eliminating the scheduling of outdoor activities during peak sun hours will be difficult, if not impossible, for many schools to do. For these schools, the best strategy might be to work toward a gradual shift in scheduling. School board policies could require architects to design new school buildings with adequate shade coverage adjacent to play and sports fields. Play and sports fields can be reviewed for existing and potential shade. School and community organization staff could evaluate frequently used spaces in the community for their UV protection status and add signs, reminders, or prompts to encourage sun safety. Finally, volunteer, business, health department, and political support can be secured by school and community organization staff to generate resources for improving the sun-safety environment, especially for providing sunscreen and shade. Policy 3: Policies for Personal Protective Clothing and Sunglasses. Schools can develop policies that encourage or require students to wear protective clothing, hats, and sunglasses to prevent excessive sun exposure. These measures could be employed during physical education classes, recess, field trips, outdoor sports or band events, and camping or field trips. Some schools, especially in Australia, have a "no hat/no play" policy stating that students cannot play outdoors if they are not wearing hats (119). Related policy initiatives could require the use of athletic, band, and physical education uniforms that reduce or minimize excessive sun exposure (e.g., long sleeves and broad-brimmed hats). Strategies that can be implemented to promote the adoption of these policies include gradually phasing-in new policies that involve students and sports teams designing new uniforms, securing business sponsorship for sun-safe uniforms, and conducting discussions that promote the use of hats and sunglasses. Some schools might have policies that prohibit or discourage students and staff from wearing hats and sunglasses on school grounds (e.g., because they are associated with contraband or gang-related items). Possible transmission of head lice among younger children who share hats might also be a concern; however, policies can be implemented that address these concerns (e.g., prohibiting both sharing hats and wearing gang-related symbols). Policy 4: Sunscreen Policies. Policies on sunscreen use at school or for after-school activities can range from encouraging parents to include sunscreen in required school-supply kits, using permission slips for students to be able to apply sunscreen at school (122), and establishing a sunscreen use routine before going outside. Policies also might require teachers and coaches to use sunscreen for outside activities and require that sunscreen be provided at official school-sponsored events that occur during midday. Necessary steps that might be implemented include modifying existing policies that restrict school-based sunscreen application (123), seeking support for purchasing sunscreen supplies, and supervising sunscreen use. Policy 5: Education Policies. The ideal education policy should support planned and sequential health education to provide students with the knowledge, attitudes, and behavioral skills needed for skin cancer prevention (Guideline 3). Policies that require teaching skin cancer prevention within health education courses will need to be balanced with the overall educational mission of the school. Policy 6: Policies for Outreach to Families. Schools and other organizations that serve youth have established methods of communicating with parents and other caregivers. Policies can ensure that these organizations routinely provide to their youth advice and information concerning skin cancer prevention. For example, information concerning skin cancer prevention might be distributed along with other health forms to parents at the beginning of the year or at parent and teacher visits. Policy 7: Resource Allocation and Evaluation. Skin cancer prevention efforts will most likely be sustained if policies exist to guide the allocation of resources for skin cancer prevention. A funding policy usually includes accountability and ongoing evaluation, thus providing for periodic review and reconsideration of how effective the resources dedicated to skin cancer prevention are being used. Guideline 2: Environmental Change --- Provide and Maintain Physical and Social Environments that Support Sun Safety and that are Consistent with the Development of Other Healthful Habits.Policies can promote the provision of supportive resources for skin cancer prevention (e.g., shade, protective clothing and hats, sunscreen at a reduced price or free, and highly visible information and prompts for sun protection) in the physical and social environment. These policies help establish routine personal behaviors and social norms that promote skin cancer prevention in the context of organized group activities. Physical Environments The majority of schools in the United States were not designed with sun safety in mind. Sun protection should be considered in the design of new schools. The design of school buildings and adjacent grounds, and the availability of natural shade (e.g., trees and mountains) or constructed shade (e.g., awnings, pavilions, and tall buildings that cast a shadow) influence potential sun exposure. Students, teachers, and families can identify opportunities to extend or create new shaded areas. These areas can be temporary or permanent, natural or constructed. Students might participate in planting trees as part of their science instruction, in which they learn which trees provide good shade cover, how and where to plant them, and how long they will need to yield valuable protection. Existing structures can be modified by constructing roofs on dugouts, installing covers for bleachers, and using awnings and tarps. An increasing selection of portable or add-on shade structures are available that school groups can purchase and install. Major construction projects to build permanent pavilions and play areas can require substantial funding, but they might be the best option in some settings. School and community partnerships can support these endeavors. School and community partnerships can facilitate provision of sunscreen that is at a reduced price or free for staff and students (through sunscreen manufacturers, pharmaceutical companies, local dermatologist offices, or hospitals) and can make sun safety more accessible during the school day or recreation period. An alternative school policy could encourage parents to apply sunscreen to their children in the morning and include it in their children's supply kits. In addition, schools and community organizations can provide hats and protective clothing (e.g., jackets) for persons who forget to bring their own on days with midday outdoor activity or field trips. Both hygiene, size, and acceptability are important considerations. However, if the school has a laundry facility for band and sports uniforms, a laundering system for emergency sun-safe protective clothing could be instituted. Information and prompts or reminders can reinforce sun-safety awareness and serve as reminders to engage in skin cancer preventive practices. Both visual and audio messages (e.g., sun-safe posters or public address system announcements) can serve as cues to action for students as well as for families, teachers, and other professionals. After students have learned about the UV index (an indicator of the intensity of the sun's rays on a given day) (124), schools can post and announce the daily UV index to encourage students to practice sun-protection measures. Some schools and recreation settings also use signs that indicate the number of minutes a person can be in the sun before sustaining a sunburn. Social Environments A supportive social environment involves establishing social norms favoring skin cancer prevention and including personal preventive behaviors as a part of organized group activities. Program planners and advocates for skin cancer prevention should serve as role models, and adults should be invited to lead by example. Schools can also create a social environment that encourages sun-safety practices through existing peer education groups by having peer educators teach other students about sun safety and by using periodic recognition or a special designation to reward teachers, staff, or students who practice sun safety. Guideline 3: Education --- Provide Health Education To Teach Students the Knowledge, Attitudes, and Behavioral Skills They Need To Prevent Skin Cancer. The Education Should be Age-Appropriate and Linked to Opportunities for Practicing Sun-Safety Behaviors.Health education that is designed effectively and implemented for youth can increase their health-related knowledge and contribute to the development of healthy changes in attitudes and behaviors (125). Skin cancer prevention is likely to be most effective when it is taught as part of a comprehensive health education curriculum that focuses on understanding the relations between personal behavior and health (126) and that provides students with the knowledge and skills outlined by the National Health Education Standards (112). The yearly timing of skin cancer prevention education can be tailored to the climate and linked with opportunities for sun exposure and sun protection. Therefore, in an area with high altitude where outdoor winter sports are common (e.g., Colorado), skin cancer prevention could be introduced before winter vacation. In northeastern coastal areas, skin cancer prevention might be most relevant before summer break. And during the school day, sun-safety lessons could directly precede recess or outdoor physical education, allowing the class session to be followed by an opportunity to practice positive sun-safety habits. Skin cancer prevention can be included as part of a comprehensive health education curriculum because of the following characteristics:
In addition to health education classes, skin cancer prevention can be integrated into other subject areas. For example, a math exercise for students could be to calculate the length of safe-sun exposure when sunscreen is used at a certain SPF. In history or social studies classes, students could discuss the social value placed on tanning and fair skin and media portrayal of tanning. Science classes could explore the light spectrum and discuss how it relates to the risk for skin cancer, or discuss depletion of the ozone and its effect on UV exposure. This type of integrated approach requires collaborative planning and curriculum development among teachers to optimize skin cancer prevention education and to ensure consistency of messages and practices. Scope and Sequence Health education is most effective in promoting positive behavioral changes when it is repeated and reinforced over time (114). Short-duration or single-presentation efforts can increase students' knowledge regarding sun safety and, in some cases, improve attitudes and sun-protection behavior immediately after the program. However, these changes are likely to be short-lived and cannot be expected to translate into sustained positive health behaviors (125). Multiunit presentations have been more effective in achieving higher increases in knowledge and skill acquisition (125). School-based health education to promote skin cancer prevention is most effective when it is provided consistently and sequentially and included periodically in every grade, from prekindergarten through 12th grade. Sequential instruction can build on information and skills learned previously. Resources for skin cancer prevention programs targeting youth are included in this report (Appendix C). Active Learning and Behavioral Focus In the previous decade, educational programs to encourage children to adopt sun-safety habits have been implemented and evaluated. Among the school-based studies reported, interventions have included one-time didactic formats and special events (97,127,128); skin cancer prevention that is integrated into classroom curricula over time (126,129,130); and peer-education programs (131,132). A majority of these studies have demonstrated that these interventions increased knowledge and favorable attitudes toward preventive behaviors. In addition, some of the programs that have multiple lessons and that occur over a longer period (e.g., 1 year) have yielded improvements in sun-protection behaviors (125). Actively engaging children and adolescents in the learning process increases the likelihood for a positive effect. Youth are more likely to consider and adopt new or improved behaviors when they learn about them through fun, participatory activities rather than through lectures. For example, a recent study demonstrated increased improvement in knowledge of the effects of UV radiation among elementary school students who used an interactive computer-based program than among those who received the same information in a didactic format led by a teacher (133). The students who completed the interactive CD-ROM program also exhibited significant positive changes in attitudes and a trend toward improvements in sun-safety behavioral scores (133). The U.S. Environmental Protection Agency offers an Internet learning site where students can report and interpret daily measurements of UV radiation, relate the UV index information to their own community, and correspond with other participating schools (124,134). Health education activities should be tailored to the cognitive and behavioral level of the students (135). For example, students in kindergarten through third grades might learn effectively through repetitious rhyming and learning the ABCs of skin cancer prevention. Games, puzzles, and contests make learning fun for students of most ages. More intellectually challenging activities might appeal to high school students, ranging from understanding the scientific basis of solar radiation and global climates, to making their own video to communicate sun-protection messages to their peers and communities. Teenagers can learn about media literacy and different cultures by analyzing images of models in popular magazines and discussing what sun exposure and a tan means to both white and non-white racial groups in the United States and worldwide. School Programs in a Broader Context The most important long-term objective of skin cancer prevention education in schools is the adoption and maintenance of sun-protection practices. Therefore, the transmission of detailed, factual information to students is the foundation of sun-safety practices. In addition, educational programs and curricula in schools are part of the broader mix of skin cancer prevention efforts and should not be expected to solely prevent skin cancer. Skin cancer prevention interventions in recreation, sports, and community settings can complement and reinforce efforts in the schools (120,136--140). Supportive policies, environments, teachers, and families are essential adjuncts to effectively planned and consistently implemented health education to prevent skin cancer. Guideline 4: Family Involvement --- Involve Family Members in Skin Cancer Prevention Efforts.The sun-safety practices of parents are the single most important determinant of the sun-protection behaviors of children (121,141). For younger children, adult family members can assist and provide sun-protection resources. For adolescents, the direct influence of parents might decrease and be subordinated by peer influence. Nonetheless, family support plays a key role in extending the desirable effects of school skin cancer prevention efforts. Involving family members in skin cancer prevention efforts increases the likelihood that they will adopt and thus model healthful sun-protection behaviors, and also appears to favorably influence the sun-protection behaviors of students (122). At a minimum, parents or guardians can be informed concerning school initiatives and policies and knowledgeable regarding how their cooperation is needed to ensure child health. Parents and guardians also can be encouraged to provide children with sun-protective clothing and sunglasses for outdoor activities. In addition, parents and guardians can serve as advocates for sun-protective policies and practices in schools and can also provide volunteer labor for health and recreation events. Their input and direct assistance can provide support for funding needed for environmental improvements and educational materials. Guideline 5: Professional Development --- Include Skin Cancer Prevention Knowledge and Skills in Preservice and Inservice Education for School Administrators, Teachers, Physical Education Teachers and Coaches, School Nurses, and Others Who Work with Students.Even effectively designed skin cancer prevention programs cannot succeed if they are not implemented as designed. Therefore, appropriate and effective professional development efforts should be conducted for decision makers and caregivers at all levels. Professional development activities, including certification programs and inservice education, are provided routinely for teachers and other school staff (e.g., coaches and school nurses). Skin cancer prevention can be integrated into these activities. All school staff should receive basic information concerning the importance of sun safety and key strategies for skin cancer prevention. The type of additional professional development needed will vary, depending on the responsibilities of the various caregivers. Inservice education for principals might address policy implementation and monitoring, whereas school nurses might highlight proper sunscreen use. Classroom teachers who implement curricula should receive training that addresses both content areas and teaching strategies. As principals, teachers, and other school staff adopt sun-protection behaviors, they can serve as role models for students. A brief training program, along with participation in conducting skin cancer prevention activities for children, can result in improved sun-protection practices among recreation leaders (142). Guideline 6: Health Services --- Complement and Support Skin Cancer Prevention Education and Sun-Safety Environments and Policies with School Health Services.School health services provide an opportunity for nurses, health educators, and school health resource specialists to promote and reinforce skin cancer prevention practices. A child's school health record can include parental permission for the child to use sunscreen provided by the school as well as a list of possible allergies to sunscreens or their ingredients. School health services staff also may conduct physical examinations for sports team eligibility, assist in managing and notifying parents concerning the long-term dangers of a severe sunburn, and prepare students for field trips. Each of these situations provides an opportunity to educate and remind students about skin cancer prevention. Health professionals in the community, including pediatricians, primary care providers, nurses, pharmacists, and dermatologists are credible sources of information and guidance for skin cancer prevention. They can be advocates for skin cancer prevention policies, environmental changes, and programs, and support school programs through presentations, professional training, demonstrations, and classroom visits. During their consultation with children and parents, these health-care professionals can also assess sun-exposure patterns, reinforce sun-protective behaviors, and provide counseling to persons with sunburns (138,143). Guideline 7: Evaluation --- Periodically Evaluate Whether Schools are Implementing the Guidelines on Policies, Environmental Change, Education, Families, Professional Development, and Health Services.Local school boards and administrators can use evaluation questions to determine whether their programs are consistent with CDC's Guidelines for School Programs To Prevent Skin Cancer. Personnel in federal, state, and local education and health agencies also can use these questions to 1) assess whether schools in their jurisdiction are providing effective education to prevent skin cancer and 2) identify schools that would benefit from additional training, resources, or technical assistance. The following questions can serve as a guide for assessing program effectiveness:
ConclusionSchools can play a substantial role in protecting students from unnecessary exposure to UV, thereby reducing their future risk for skin cancer. A comprehensive school approach to skin cancer prevention includes policies, environmental change, educational curricula, family involvement, professional development, integration with health services, and evaluation. The exposure of youth to harmful UV radiation today contributes to their risk for skin cancer later in life. Unlike many diseases, skin cancer is primarily preventable. Schools, in partnership with community groups and other national, federal, state, and voluntary agencies, can develop, implement, and promote initiatives that help protect youth from UV exposure (144,145). These guidelines serve as a framework for such initiatives. References
Figure 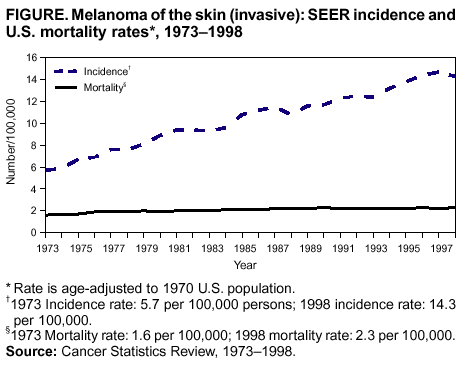 Return to top. Box 1 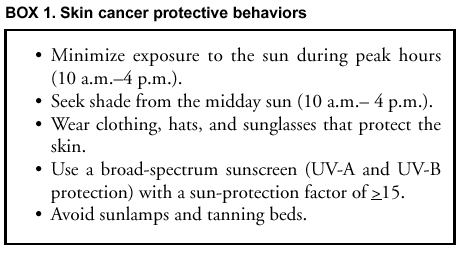 Return to top. Box 2 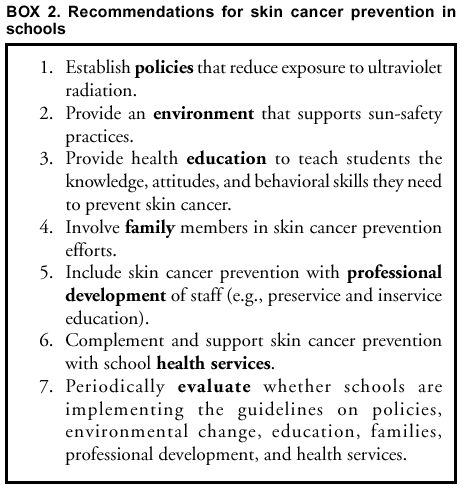 Return to top. Participating Agencies and OrganizationsAmerican Academy of Dermatology;* American Academy of Pediatrics,* American Association for Health Education;* American Cancer Society;* AMC Cancer Research Center and Foundation;* American Optometric Association;* American Pharmaceutical Association;* American School Health Association;* Council of Chief State School Officers; Dermatology Nursesí Association;* Environmental Protection Agency;* Melanoma Research Foundation;* National Association for Sport and Physical Education; National Association of School Nurses, Inc.;* National Association of State Boards of Education; National Cancer Institute;* National Education Association; National Safety Council;* National School Boards Association; Presidentís Council on Physical Fitness and Sports; Skin Cancer Foundation;* Skin Cancer Prevention Program, California Department of Health Services;* Society of State Directors of Health, Physical Education and Recreation; Society for Public Health Education;* U.S. Department of Education. Participants Melissa Galvin, Ph.D., M.P.H., University of Alabama; Kim Reynolds, Ph.D., University of Alabama; Barbara Bewerse, M.N., M.P.H., University of North Carolina; Corinne Graffunder, M.P.H., CDC; Rebeca Lee-Pethel, M.P.A., CDC. * Members of the National Council for Skin Cancer Prevention who independently have endorsed the Guidelines for School Programs To Prevent Skin Cancer.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 4/11/2002 |
|||||||||
This page last reviewed 4/11/2002
|