 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Indicators for Chronic Disease SurveillancePrepared collaboratively by The material in this report originated in the National Center for Chronic Disease Prevention and Health Promotion, James S. Marks, M.D., M.P.H., Director, and the Division of Adult and Community Health, Virginia S. Bales Harris, M.P.H., Director. SummaryChronic diseases account for seven of the 10 leading causes of death in the United States, including the three leading causes of preventable death (tobacco use, improper diet and physical inactivity, and alcohol use). Seventy percent of health-care costs in the United States are for chronic diseases. In 1999, to allow public health officials to uniformly define, collect, and report chronic disease data, the Council of State and Territorial Epidemiologists released Indicators for Chronic Disease Surveillance. The report provided standard definitions for 73 indicators developed by epidemiologists and chronic disease program directors at the state and federal level. The indicators were selected because of their importance to public health and the availability of state-level data. This report describes the latest revisions to the chronic disease indicators. The revised set of 92 indicators includes 63 indicators that were unchanged from the first edition, six that have been revised, and 23 that are new. Four indicators from the first edition were deleted. Of the indicators, 24 are for cancer; 15 for cardiovascular disease; 11 for diabetes; seven for alcohol; five each for nutrition and tobacco; three each for oral health, physical activity, and renal disease; and two each for asthma, osteoporosis, and immunizations. The remaining 10 indicators cover such overarching conditions as poverty, education, life expectancy, and health insurance. Additional information regarding the indicators for chronic disease surveillance is available at http://www.cdc.gov/nccdphp/cdi. IntroductionDuring the 20th century, the leading causes of death in the United States shifted from infectious to chronic diseases. Chronic diseases (e.g., cardiovascular disease, cancer, and diabetes) are now among the most prevalent, costly, and preventable of all health problems. Seven of every 10 U.S. residents who die each year (>1.7 million persons) do so as a result of a chronic disease. Chronic diseases affect the quality of life of 90 million U.S. residents (1), and the cost of medical care for persons with these diseases accounts for 70% of total medical care expenditures (2). Although chronic diseases are among the most common and costly health problems, they are also among the most preventable. Adopting healthy behaviors (e.g., eating nutritious foods, being physically active, and avoiding tobacco use) can prevent or control the effects of these diseases. In addition, quality of life is enhanced when chronic diseases are detected and treated early. Regular screening can reduce morbidity and mortality from cancers of the breast, cervix, colon, and rectum. Clinical preventive services can prevent the debilitating complications of diabetes and cardiovascular disease. Increased chronic disease mortality and greater opportunities for primary and secondary prevention of chronic disease have resulted in an expansion of chronic disease programs in state public health agencies. Community intervention programs have proved to be effective, and certain ones have become model programs for public health (3,4). Within the past decade, each state has developed programs in tobacco control and breast and cervical cancer control. Comprehensive public health programs necessarily include monitoring of disease or risk factors through public health surveillance, which is defined as the ongoing systematic collection, analysis, and interpretation of outcome-specific data for use in planning, implementing, and evaluating public health practice (5). Multiple data systems form the foundation for chronic disease surveillance. Chronic disease surveillance initially focused on mortality data from the National Vital Statistics System, managed by CDC's National Center for Health Statistics. However, in the 1970s, morbidity from selected chronic diseases came under surveillance through disease registries. For example, the National Cancer Institute established the Surveillance, Epidemiology, and End Results cancer registry system to record and follow every new case of cancer among nine specific U.S. populations, four of which were states. In 1992, Congress authorized the National Program of Cancer Registries (NPCR) at CDC to monitor local trends in cancer incidence and mortality with statewide, population-based cancer registries. In the 1980s and 1990s, CDC and state health agencies collaboratively developed additional surveillance systems to monitor behavioral risk factors for chronic disease. In 1984, with CDC assistance, 15 state health agencies began to use the Behavioral Risk Factor Surveillance System (BRFSS) to monitor adult behaviors related to the leading causes of death. Recognizing the usefulness and flexibility of BRFSS, all 50 states, the District of Columbia, and three territories participated in the system by 1994. By 2003, a total of 43 states and 22 local areas (also supported with financial and technical assistance from CDC) used the Youth Risk Behavioral Surveillance System (YRBSS) to monitor health risk behaviors among high school students. Abbreviations Used in This Report
Chronic Disease Indicators In 1996, the Council of State and Territorial Epidemiologists (CSTE) voted to place the prevalence of cigarette smoking among adults, data for which were collected for each state by BRFSS, under nationwide surveillance. This was the first time that CSTE --- the professional organization that, in conjunction with CDC, has historically reviewed and recommended procedures for nationwide, state-based surveillance --- had placed a personal behavior associated with a chronic disease under nationwide surveillance. This action effectively defined the first indicator for chronic disease surveillance. In addition, this was the first time that a survey sample was designated as the mechanism by which surveillance data would be used for nationwide, state-level surveillance. Although conducting nationwide surveillance for prevalence of cigarette smoking among adults was important, it made CSTE, the chronic disease directors (CDD), and CDC more aware of the lack of a comprehensive and consistent approach to state-level chronic disease surveillance. For example, no guidelines existed for state-level surveillance of other behavioral risks (e.g., physical inactivity or unhealthy eating). Similarly, state-level epidemiologists did not necessarily employ consistent methods to report chronic diseases and risk factors. For example, epidemiologists from different states might have been using the 1940 U.S. population, the 1970 U.S. population, or a population of their own state for standardization of rates. To address the need for common definitions and methods for state-level chronic disease surveillance, CSTE, CDD, and CDC collaborated in a 2-year process that led CSTE to adopt 73 chronic disease indicators (CDI) (6). The 73 indicators were chosen because 1) the disease or condition being monitored by the indicator incurred a substantial public health burden, and 2) surveillance data were available for the majority of states. The indicators provided 1) a minimal set of chronic diseases, conditions, and risk factors that would be under state-level surveillance; 2) consistent methods for state-level analyses, results from which would provide comparable state-specific data; and 3) an operational measure of state-level capacity in chronic disease surveillance, with a state's successful use of the indicators being one benchmark of the state's efforts in chronic disease surveillance. In 2001, CSTE, CDD, and CDC began revising the chronic disease indicators. Chronic disease epidemiologists, program managers, subject matter experts, and partner organizations met to review existing indicators and to propose a revised set of indicators. Proposed indicators were evaluated for their relevance to chronic disease prevention and control at the state level and for the availability of data on an annual or biannual basis at the state level for the majority of states. In addition, an attempt was made to select indicators that were consistent with Healthy People 2010 objectives (7). At the 2002 annual meeting, CSTE membership approved a revised set of 92 chronic disease indicators (Table) (see Appendix). This report describes how each indicator is to be measured, why it is important, the limitations for both the indicator and its data source, and the relevant objective in Healthy People 2010 (7). Data SourcesData for surveillance of chronic disease indicators are derived from multiple sources.
Data ConcernsCertain concerns related to data analysis should be considered when using the chronic disease indicators. To be comparable, standardized chronic disease indicator rates should use the same standard population figures. In 1999, the U.S. Department of Health and Human Services began to adjust all mortality data to the year 2000 U.S. standard population to enhance the comparability of disease rates for different geographic areas and subpopulations. Whenever possible, rates for chronic disease indicators should be standardized to the year 2000 U.S. population. Because the age of the population being monitored is not the same for all indicators, each indicator that calls for an age-standardized measure has a particular age distribution to be used in the standardization process (15). Certain agencies and professional organizations have established thresholds for the quality of data. For example, NAACCR has calculated combined incidence rates only for data from cancer registries of the highest quality, as demonstrated by compliance with all requests and standards related to completeness and quality. Also, CDC only weights YRBSS data to produce state-specific estimates for surveys that have an overall response rate of >60% and have appropriate survey documentation. In addition, because surveillance that is based on a limited number of cases in a defined geographic area or demographic group might compromise a person's confidentiality, public health agencies often do not publish surveillance reports or summary information that is based on less than a specific number (e.g., five) of cases. The threshold for publishing data might also depend on the geographic level and size of the population for which the data are reported. Another concern is that rates based on limited numbers are inherently unstable. For example, if five persons among a population of 10,000 have a particular chronic disease and six persons among another population of 10,000 have the same disease, the rate among the second population is 1.2 times higher. However, the 20% increase is from only one additional case; such variations can be within the expected random fluctuation of disease occurrence. Finally, to partially adjust for potential nonresponse and sample selection bias, sample surveys (e.g., BRFSS and YRBSS) typically weight their data. The weights are estimates of the population by subgroup (e.g., age, race, or sex) from which the survey data were collected. Future NeedsThe indicators should be reviewed periodically because of changes in availability of data and public health priorities for chronic disease. Surveillance data sources at the state level should also be improved. For example, multiple states do not participate in YRBSS or have access to hospital discharge data. Finally, not all states have sufficient chronic disease epidemiology capacity to collect, analyze, and report on the data required for each indicator. Fifteen (30%) states and the District of Columbia do not report having a state chronic disease epidemiologist (16). References1. CDC. Chronic disease prevention. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for Chronic Disease Prevention and Health Promotion, 2004. Available at http://www.cdc.gov/nccdphp. 2. CDC. The burden of chronic diseases and their risk factors: national and state perspectives. Atlanta, GA: US Department of Health and Human Services, CDC, 2004. 3. American Cancer Society, Association for Healthcare Quality Research, CDC, National Cancer Institute, Substance Abuse and Mental Health Services Administration. Cancer control PLANET: links to resources for comprehensive cancer control. Available at http://cancercontrolplanet.cancer.gov. 4. Task Force on Community Preventive Services. Guide to community preventive services. Atlanta, GA: US Department of Health and Human Services, CDC, 2003. Available at http://www.thecommunityguide.org. 5. Thacker S. Historical development. In: Teutsch S, Churchill R, eds. Principles and practice of public health surveillance. 2nd ed. New York: Oxford University Press, 2000. 6. Lengerich EJ, ed. Indicators for chronic disease surveillance: consensus of CSTE, ASTCDPD, and CDC. Atlanta, GA: Council of State and Territorial Epidemiologists, 1999. 7. US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health (2 vols.). Washington DC: US Department of Health and Human Services, 2000. 8 CDC. Behavioral Risk Factor Surveillance System: turning information into health. Atlanta, GA: US Department of Health and Human Services, CDC, 2004. Available at http://www.cdc.gov/brfss. 9. CDC. National program of cancer registries. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for Chronic Disease Prevention and Health Promotion, 2004. Available at http://www.cdc.gov/cancer/npcr. 10. Bureau of Labor Statistics, Bureau of the Census. Current population survey. Washington, DC: US Department of Labor, US Census Bureau, 2001. Available at http://www.bls.census.gov/cps/cpsmain.htm. 11. CDC. Mortality data from the national vital statistics system. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics, 2004. Available at http://www.cdc.gov/nchs/about/major/dvs/desc.htm. 12. CDC. STATE: State Tobacco Activity Tracking & Evaluation System. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for Chronic Disease Prevention and Health Promotion. Available at http://www2.cdc.gov/nccdphp/osh/state. 13. USRDS Coordinating Center. USRDS: United States Renal Data System. Minneapolis, MN: USRDS Coordinating Center, 2004. Available at http://www.usrds.org. 14. CDC. Youth Risk Behavior Surveillance System. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for Chronic Disease Prevention and Health Promotion, 2004. Available at http://www.cdc.gov/yrbs. 15. Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics, 2001. Healthy people 2010 statistical notes, no. 20. 16. Council of State and Territorial Epidemiologists. Current state chronic disease epidemiologists. Atlanta, GA: Council of State and Territorial Epidemiologists, 2004. Available at http://www.cste.org/surveys/scdesurveyresultreviewList.asp.
Chronic Disease Indicators Working Group June 2004 Mark Baptiste, Ph.D., and Ursula Bauer, Ph.D., New York State Department of Health; Katrina Hedberg, M.D., Oregon Department of Human Services; Gary Hogelin (retired), M.P.H., Andrew Pelletier, M.D., and Paul Z. Siegel, M.D., CDC; Donna Kephart, M.H.A., and Eugene Lengerich, V.M.D., Pennsylvania State University; Donna Knutson, M.S.Ed., LaKesha Robinson, M.P.H., and Shah Roohi, Council of State and Territorial Epidemiologists; John Kurata, M.D., California State Department of Health Services; and Adeline Yerkes, M.P.H., Oklahoma State Health Department.
Table 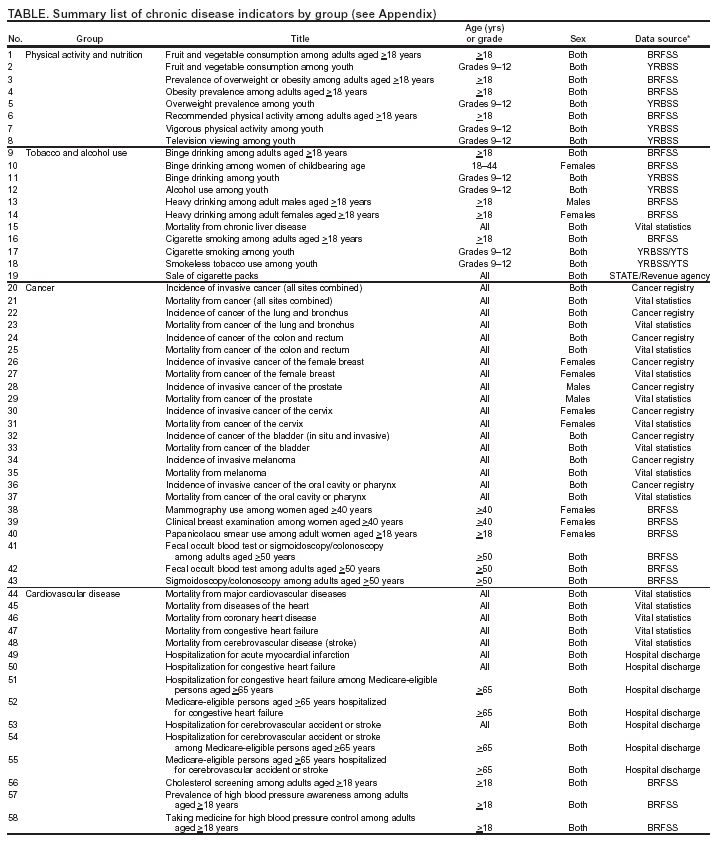 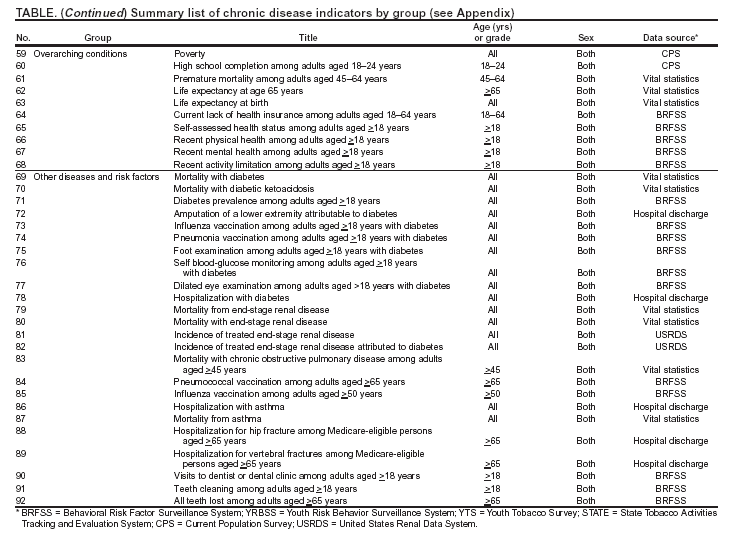 Return to top. Chronic Disease Indicators: Physical Activity and Nutrition
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 8/30/2004 |
|||||||||||||||||||||||||||||||||||||||||||||||
This page last reviewed 8/30/2004
|