 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Chronic Obstructive Pulmonary Disease Surveillance --- United States, 1971--2000David M. Mannino, M.D.1 1Division of Environmental Hazards and Health Effects Abstract Problem/Condition: Chronic obstructive pulmonary disease (COPD) includes chronic bronchitis and emphysema but has been defined recently as the physiologic finding of nonreversible pulmonary function impairment. This surveillance summary reports trends in different measures of COPD during 1971--2000. Reporting Period Covered: This report presents national data regarding objectively determined COPD (1971--1994); COPD-associated activity and functional limitations (1980--1996); self-reported COPD prevalence, COPD physician office and hospital outpatient department visits, COPD hospitalizations, and COPD deaths (1980--2000); and COPD emergency department visits (1992--2000). Description of Systems: CDC's National Center for Health Statistics (NCHS) conducts the National Health Interview Survey annually, which includes questions concerning COPD and activity limitations. NCHS collects physician office-visit data in the National Ambulatory Medical Care Survey, emergency department and hospital outpatient department data in the National Hospital Ambulatory Medical Care Survey, hospitalization data in the National Hospital Discharge Survey, and death data in the Mortality Component of the National Vital Statistics System. Data regarding pulmonary function were obtained from the National Health and Nutrition Examination Surveys (NHANES) I (1971--1975) and III (1988--1994), and data regarding functional limitation were obtained from NHANES III, Phase 2 (1991--1994). Results: During 2000, an estimated 10 million U.S. adults reported physician-diagnosed COPD. However, data from NHANES III estimate that approximately 24 million U.S. adults have evidence of impaired lung function, indicating that COPD is underdiagnosed. During 2000, COPD was responsible for 8 million physician office and hospital outpatient visits, 1.5 million emergency department visits, 726,000 hospitalizations, and 119,000 deaths. During the period analyzed, the most substantial change was the increase in the COPD death rate for women, from 20.1/100,000 in 1980 to 56.7/100,000 in 2000, compared with the more modest increase in the death rate for men, from 73.0/100,000 in 1980 to 82.6/100,000 in 2000. In 2000, for the first time, the number of women dying from COPD surpassed the number of men dying from COPD (59,936 versus 59,118). Another substantial change observed is that the proportion of the population aged <55 years with mild or moderate COPD, on the basis of pulmonary function testing, decreased from 1971--1975 to 1988--1994, possibly indicating that the upward trends in COPD hospitalizations and mortality might not continue. Interpretation: COPD is a major cause of morbidity, mortality, and disability in the United States. Despite its ease of diagnosis, COPD remains an underdiagnosed disease, chiefly in its milder and more treatable form. IntroductionChronic obstructive pulmonary disease (COPD) is a group of diseases characterized by airflow obstruction that can be associated with breathing-related symptoms (e.g., chronic cough, exertional dyspnea, expectoration, and wheeze) (1). COPD can be present with or without substantial physical impairment or symptoms, and it is the fourth leading cause of death in the United States (2). However, COPD is often a silent and unrecognized disease, chiefly in its early phases (3). During 1993, the estimated direct medical costs of COPD were $14.7 billion (4). Also during 1993, the estimated indirect cost related to morbidity (e.g., loss of work time and productivity) and premature mortality was an additional $9.2 billion, for a total of $23.9 billion. Healthy People 2010 includes two objectives related to COPD: to reduce the proportion of adults whose activity is limited because of chronic lung and breathing problems to 1.5% (Objective 24-9) and to reduce deaths from COPD among adults aged >45 years to 60 deaths/100,000 (Object 24-10) (5). Traditionally, COPD has been diagnosed on the basis of patient-reported symptoms (6,7). The recently published definition from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) has classified COPD as "a disease state characterized by airflow limitation that is not fully reversible" (8) and recommends measurement of lung function both to diagnose disease and categorize disease severity. Airflow limitation is the slowing of expiratory airflow as measured by spirometry, with a persistently low forced expiratory volume in 1 second (FEV1) and a low FEV1/forced vital capacity (FVC) ratio despite treatment (7). The GOLD criteria for mild COPD (stage 1) is an FEV1/FVC ratio of <70% and FEV1 of >80% predicted, and the criteria for moderate COPD (stage 2 or 3) is an FEV1/FVC ratio of <70% and an FEV1 <80% predicted (8,9). This report presents national data regarding objectively determined (i.e., by spirometry) COPD (1971--1994); COPD-associated activity and functional limitations (1980--1996); self-reported COPD prevalence, COPD physician office and hospital outpatient department visits, COPD hospitalizations, and COPD deaths (1980--2000); and COPD emergency department visits (1992--2000). MethodsFor this report, we defined COPD as including chronic bronchitis and emphysema when we used survey data based on clinical diagnosis. In doing so, asthma and bronchiectasis were excluded, but they are often included in other definitions of COPD and related conditions. Asthma was excluded because its etiology and treatment differs from that for COPD, although clinical similarities exist between these conditions. CDC recently published surveillance data for asthma (10). Bronchiectasis was excluded because it typically is caused by infection and has a different treatment and prognosis than COPD. Data from national health surveys conducted by CDC's National Center for Health Statistics (NCHS) were used to report these measures. In addition, the resident population estimates from the U.S. Bureau of the Census were used as denominators for rates of COPD office visits, COPD emergency department visits, COPD hospitalizations, and COPD deaths. These denominators vary slightly from those typically used with these databases because we wanted a consistent denominator for these measures. The National Health and Nutrition Examination Surveys (NHANES) and National Health Interview Survey (NHIS) weights (corresponding to the civilian, noninstitionalized population of the United States) were used to estimate the population when those data sets were analyzed. When calculating rates that used pulmonary function data, we limited the denominator to subjects who had pulmonary function testing performed. In the tables for this report, annual estimates are listed for selected years (1980, 1985, 1990, and 1995--2000), and in the figures, annual estimates are listed for 1980--2000 for the majority of measures. Measures that were only available for limited years included 1) activity limitation, for which years are grouped because the denominator (persons with COPD) was smaller; 2) objectively determined COPD, for which two samples (1971--1975 and 1988--1994) were available; and 3) functional limitation, for which one sample (1991--1994) was available. Our results were age-adjusted to the 2000 U.S. population by using five age groups (i.e., 25--44 years, 45--54 years, 55--64 years, 65--74 years, and >75 years). Data were stratified by sex, race (i.e., white, black, and other), and age group (i.e., 25--44 years, 45--54 years, 55--64 years, 65--74 years, and >75 years) for subgroup analyses. Persons of other races (e.g., Asians and American Indians) were grouped together because their numbers in individual racial groups were too limited to yield statistically stable estimates. We analyzed all data by using SAS (11) and SUDAAN (12). Two-tailed, weighted, least-squares regression (by using the inverse of the relative standard error of the estimate as the weight) was used to determine whether linear trends were statistically significant. Trend testing was performed only when >5 years of continuous data were available for analysis. Two-tailed t-tests were used to compare measures between racial groups, age groups, and males and females. By using the Bonferroni adjustment for multiple comparison among <5 groups, we considered a familywide p-value of 0.05 as statistically significant. Self-Reported PrevalenceNCHS conducts NHIS annually among a probability sample of the civilian, noninstitutionalized population of the United States (13). Before 1997, for one-sixth of the NHIS-sampled households (approximately 20,000 of 120,000 persons), respondents were asked whether anyone in the household had any of 17 chronic respiratory conditions, including chronic bronchitis or emphysema, during the preceding 12 months. Under this design, information related to COPD among adults might have been reported by the respondents themselves or by a household respondent. A COPD diagnosis was determined if the response was positive to either of the following questions: "During the past 12 months did [you] have bronchitis," if the condition was listed as chronic, or "During the past 12 months did [you] have emphysema?" Beginning in 1997, NHIS collected information concerning COPD for a randomly selected adult in each household. COPD prevalence was determined if participants responded positively to either of the following questions: "Have you ever been told by a doctor or other health professional that you had emphysema," or "During the past 12 months, have you been told by a doctor or other health professional that you had chronic bronchitis?" (13). NHANES III was conducted during 1988--1994 (12). Subjects were asked, "Has a doctor ever told you that you had chronic bronchitis;" "Has a doctor ever told you that you had emphysema;" and "Do you still have chronic bronchitis?" Subjects were regarded as having COPD if they reported a diagnosis of emphysema or current chronic bronchitis. SUDAAN was used to determine relative standard errors (RSEs) of the estimates and to indicate which estimates were reliable (i.e., RSE < 30%) (14). Objectively Determined PrevalenceDuring 1971--1975, NCHS conducted the first National Health and Nutrition Examination Survey (NHANES I) (15,16). Both NHANES I and NHANES III were probability samples of the civilian, noninstitutionalized U.S. population. Spirometry was obtained on a subset of survey participants (5,080 adults in NHANES I and 13,869 adults in NHANES III). The procedures used have been documented previously (12,16). Values used in this analysis included FVC, FEV1, and the FEV1/FVC ratio. Predicted values of FEV1 and FVC were identified by performing linear regression (stratified by sex and by using age and height as predictors) on a subgroup of participants who were white and who had never smoked and did not report respiratory symptoms or physician-diagnosed lung disease. Results from these regression models were applied to the data from all participants to obtain predicted values of FEV1 and FVC. An adjustment factor of 0.88 was used to estimate predicted values for black participants (17). Participants were classified as having moderate obstructive lung disease if both the FEV1/FVC ratio was <70% and the FEV1 was <80% of the predicted value (8). Participants were classified as having mild obstructive lung disease if the FEV1/FVC ratio was <70% and the FEV1 was >80% of the predicted value. Activity and Functional LimitationsThrough 1996, NHIS provided data related to activity limitations overall and resulting from specific conditions. Activity limitations were classified into one of four groups: unable to perform major activity, certain limitation in major activity, limitation in other activities, or no activity was limited. Major activity was defined as working or keeping house for adults aged 18--69 years, and ability to execute activities of independent living for those aged >70 years. The percentage of persons with and without COPD who reported activity limitation (including unable to perform major activities, limited in major activities, and limited in other activities) was calculated for all adults aged >25 years. The percentage of persons who reported having COPD and who also reported COPD-associated activity limitation was also calculated. Respondents were categorized as limited because of COPD if they reported that COPD was the primary or secondary cause of the limitation. Because of the relatively low number of persons reporting limited activity, multiple years of data were used to obtain stable estimates. Data from NHANES III, Phase 2 (1991--1994), were used to determine physical functional limitation. During the home interview, participants aged >17 years were asked a series of questions regarding their physical functioning. From these questions, the following three items were selected: difficulty walking ¼ mile; lifting or carrying something weighing 10 pounds; and need of help from other persons in handling routine tasks (e.g., doing everyday household chores, conducting necessary business, shopping, or getting around for other purposes). For the first two items (difficulty walking or lifting), respondents could answer "no difficulty," "some difficulty," "much difficulty," and "unable to do." These responses were dichotomized into no difficulty and any difficulty. For the last item (handling routine needs), respondents could respond yes or no. The age-adjusted proportion of functional limitation among participants with current reported COPD (chronic bronchitis or emphysema) and no reported COPD were identified (3), and this was repeated for the same group of participants stratified by level of pulmonary function impairment. SUDAAN was used to determine RSEs of the estimates (14). Physician Office Visits, Hospital Outpatient Department Visits, and Emergency Department VisitsAmbulatory medical care is the predominant means of providing health-care services in the United States. We considered both physician office visits and hospital outpatient department visits, which are collected, by using different surveys, as office visits and emergency department visits separately. Physician office-visit data were collected through the National Ambulatory Medical Care Survey (NAMCS), which NCHS conducted during 1973--1981, 1985, and annually since 1989 (18). Approximately 2,000 physicians participated each year, reporting data concerning approximately 30,000 patient encounters. Hospital outpatient-visit data and emergency department-visit data were collected by using the National Hospital Ambulatory Medical Care Survey (NHAMCS), which has been conducted annually since 1992 (19). Approximately 500 hospitals are sampled each year, resulting in approximately 30,000 outpatient department encounters and 30,000 emergency department encounters. By using both data sets, we identified all patient visits for which COPD (International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM), codes 490--492, 496) (20) was the first-listed diagnosis. Sample weights were used to obtain national estimates of annual outpatient visits (physician office and hospital outpatient department visits were combined beginning in 1992) and emergency department visits for COPD. RSEs, which are listed with the database documentation, were used to determine which estimates were reliable (i.e., RSE < 30%) (21). HospitalizationsThe National Hospital Discharge Survey (NHDS), conducted annually by NCHS since 1965, is a national survey of approximately 275,000 patient records from approximately 500 nonfederal general and short-stay specialty hospitals. A hospitalization for COPD was defined as a primary discharge diagnosis of COPD (ICD-9-CM codes 490--492, 496) (20). In addition, a hospitalization was considered as a result of COPD if it had a first-listed diagnosis of acute bronchitis (ICD-9-CM code 466--466.1) accompanied by another listed diagnosis of COPD. During 1980--1982, approximately 15%--24% of all first-listed diagnoses of acute bronchitis were accompanied by another listed diagnosis of COPD (chronic bronchitis, emphysema or COPD, not specified); however, during 1983--1991, this proportion ranged from 39% to 58%. During 1992, a new ICD-9-CM code, 491.21, was introduced to categorize obstructive chronic bronchitis with acute exacerbation. After the introduction of this new code, 3%--10% of all first-listed diagnoses of acute bronchitis were accompanied by another listed diagnosis of COPD during 1992--2000. During any selected year, race was missing for 5%--20% of the sample (22). These persons were excluded from the race-specific rate calculations but were included in all other rate calculations. Published relative standard errors (21) were used to indicate which estimates were reliable (i.e., RSE < 30%). MortalityThe Mortality Component of the National Vital Statistics System includes medical conditions and reported demographic characteristics regarding death (23). We searched for deaths for which COPD was the underlying cause (ICD-9 codes 490--492, 496, for 1980--1998; ICD-10 codes J40--J44 for 1999--2000) (24,25). In ICD-10, the term chronic lower respiratory disease is used to describe the diseases encompassed by the term COPD. Comparability ratios for ICD-10 relative to ICD-9 for COPD are as follows: 0.97 for emphysema, 1.10 for other chronic lower respiratory diseases, 0.39 for chronic and unspecified bronchitis, and 1.05 for all chronic lower respiratory diseases, which includes asthma (26). Standard errors were calculated as the square root of the inverse of the number of deaths (23). ResultsPrevalenceThe estimated number and rates of persons reporting COPD are included in this report (Tables 1 and 2) (Figures 1--3). Whites had statistically significant higher rates than blacks for certain years examined (Figure 2). Since 1987, women have had higher rates of self-reported COPD than men, and during 1980--1996, the trend for COPD increased for women but not for men (Figure 3). The 1997 redesign of NHIS might have had an effect on COPD prevalence, although the observed year-to-date variation in COPD prevalence makes this difficult to discern (Figures 2 and 3). Data from NHANES I and NHANES III estimating the prevalence of COPD on the basis of spirometric definitions are presented (Tables 3 and 4) (Figure 1). For both mild and moderate COPD, the prevalence was higher among men than women and increased with increasing age. From NHANES I to NHANES III, prevalence of moderate COPD decreased among men but not among women (Table 4). When stratified by age group, a statistically significant decrease occurred in moderate COPD among persons aged 25--54 years, but not among other groups; and, when stratified by race, a similar decrease occurred among blacks, but not whites. Activity and Functional LimitationsThe age-adjusted employment rate is lower among persons who report they have COPD (Table 5). During the period analyzed, only limited change occurred in prevalence of activity limitation among adults with self-reported COPD (Table 5). Adults with COPD have a prevalence of any activity limitation approximately twice as high as adults without COPD. During 1994--1996, 8.0% of persons with COPD reported activity limitation caused by their COPD. Respondents with self-reported COPD had a higher proportion of functional limitation than did persons without self-reported COPD (Table 6). Among subjects with spirometrically determined COPD, no measures of functional impairment were substantially increased, compared with subjects with normal lung function (Table 6). Physician Office and Hospital Outpatient Department VisitsData for physician office and hospital outpatient department visits for COPD are presented in this report (Tables 7 and 8). No statistically significant trend during 1989--2000 was identified (Figure 4). Whites had a significantly higher rate of visits than did blacks during certain years examined, although estimates for blacks were unreliable for the majority of years. No consistent differences were identified between men and women for physician office and hospital outpatient department visits for COPD, but visit rates increased with increasing age. Emergency Department VisitsData for emergency department visits for COPD are presented (Tables 9 and 10). During the study period, a significant upward trend occurred in emergency department visits for COPD. Blacks had consistently higher rates than whites for the majority of years examined (Figure 5). No consistent pattern for sex was observed. Within age groups, the highest rates were observed among older age groups. HospitalizationsData for hospitalizations for COPD are presented (Tables 11 and 12). During 1984--1989, hospitalization rates for COPD decreased, but during 1990--1999, hospitalization rates increased (Figures 6 and 7). Hospitalization rates for COPD among whites were greater than those among blacks during 1980--1987, after which rates have been similar (Figure 7). However, approximately <20% of hospitalizations did not have race listed (22). Hospitalization rates for men were greater than those for women through the 1980s; however, since 1995, these rates have been similar (Figure 6). Since 1990, hospitalizations for COPD have increased among all age groups, with the largest increases observed for those persons aged 65--74 years (62%) and those aged >75 years (52%). DeathsDuring 1980--2000, the overall death rate for COPD increased 67% (Tables 13 and 14). During this period, rates among whites increased 67%, and rates among blacks increased 87%. However, deaths rates for whites remained higher than those for blacks throughout the 21-year period. During 1980--2000, death rates for COPD among men increased 13%; however, death rates among men remained steady since 1985. During 1980--2000, death rates for COPD among women approximately tripled and increased steadily throughout the period (Figure 8). During 2000, the number of women who died from COPD was, for the first time, higher than the number of men who died from COPD. During 1999--2000, death rates for COPD were higher, compared with 1998. Because the comparability ratio for coding COPD under ICD-10 compared with ICD-9 is >1, which results in a higher number of COPD deaths under ICD-10, increases observed for 1999 reflect in part the impact of a new disease classification system. DiscussionThese data identified certain trends in COPD-related morbidity and mortality in the United States. First, COPD-related deaths among women continued to increase. By 2000, the number of COPD deaths among women surpassed the number among men, although the population-based mortality rates remain higher among men. Second, since 1989, COPD hospitalizations have also increased, combined with an elimination of the difference in hospitalization rates between men and women. Third, the proportion of the population aged <55 years with mild or moderate COPD, on the basis of pulmonary function testing, decreased from 1971--1975 to 1988--1994, whereas this proportion did not change substantially among other age groups. The increasing trends in COPD hospitalizations and mortality among women reported here probably reflect the increase in smoking by women since the 1940s, relative to men, in the United States (27). The natural history of COPD among smokers is that smoking behaviors start during youth, lung function decline becomes apparent when smokers reach age 40--50 years, hospitalizations begin when smokers reach age 50--69, and deaths occur when they reach age 60--79 (1). The data in this report support this natural history with regard to different trends among men and women: That is, since the late 1980s, women have had a similar hospitalization rate for COPD (Figure 6); and since 1980, the COPD mortality gap between women and men has narrowed. However, the decreasing proportion of adults aged 25--54 years with objective evidence of COPD (Table 4) is most likely related to lower smoking prevalence among the U.S. population since the 1960s (27). Objective measures are critical in determining whether COPD is present. Historically, COPD has been defined by the presence of certain symptoms (e.g., cough and sputum production). Compared with COPD defined by using pulmonary function testing, this historic method results in underdiagnosis of this condition, chiefly among older populations and among persons with mild disease (3). The GOLD criteria (9) allow clinicians to diagnose and classify COPD on the basis of pulmonary function testing. These criteria recognize that symptoms might be present or absent, even among persons with substantial degrees of impairment. For example, the data demonstrate that a higher proportion of men had evidence of obstructive lung disease than women (Table 4), which is supported by the consistent finding of a higher COPD death rate among men (Table 14). This can be contrasted with the higher proportion of women reporting COPD on the basis of physician diagnosis, which is not necessarily based on objective criteria. During 1994--1996, approximately 8.0% of adults with COPD reported activity limitation caused by COPD (Table 5). Whether this measure captured completely the degree of disability associated with COPD is unclear because participants might not have accurately classified the cause of their disabilities or they might have comorbid conditions that cause disability also. For example, during 1994--1996, a total of 38.6% of participants with COPD and 18.4% of those without COPD reported activity limitation, indicating that COPD-associated activity limitation might be higher than the 8.0% reported or that other comorbid diseases, which are possibly smoking-related, occur more frequently among persons with COPD. The data regarding reported functional limitation indicated a higher prevalence of limitation among participants with COPD (Table 6). Actual testing of functional capabilities relevant to COPD (e.g., a 6-minute walk) could not be performed in NHANES III because of time limitations. The dramatic drop in COPD hospitalizations during 1983--1989 is probably related to systematic changes in U.S. health care at that time (e.g., introduction of diagnosis-related groups for compensation, overall pressures within the health-care system to decrease hospitalizations, or other unknown factors). Our observation that COPD mortality steadily increased throughout this period would indicate that the observed decrease was not related to a lower prevalence of severe COPD among the population. Since 1989, COPD hospitalization rates have steadily increased, with the rate among women now similar to that among men and the rate among blacks similar to that among whites. Tobacco use is the key risk factor in COPD development and progression, and trends in COPD mortality among women reported here reflect the recent increase in smoking by women, relative to men, in the United States (27). Although tobacco smoking is the most critical risk factor for both development and progression of COPD, asthma (28), exposure to ambient pollutants in the home and workplace (29), and respiratory infections (30,31) are also key factors. In addition, COPD is a risk factor for other outcomes (e.g., lung cancer or early death) (32,33). Early detection of COPD might alter its course and prognosis. The National Lung Health Education Program (NLHEP) is a new health-care initiative aimed at involving primary-care physicians in early identification and treatment of obstructive lung disease (34). NLHEP is promoting widespread use of simple office spirometry to measure pulmonary function among current and former smokers aged >45 years and anyone with respiratory symptoms. Although spirometry is a relatively easy test to perform, it does require training of both the test administrator and the patient to obtain an accurate result. Two Healthy People 2010 objectives relate to COPD: Reduce proportion of adults whose activity is limited because of chronic lung and breathing problems among adults aged >45 years to 1.5% in 2010 (Objective 24-9), compared with 2.2% in 1997, and reduce deaths from COPD among adults aged >45 years to 60 deaths/100,000 in 2010, compared with 119.4 deaths/100,000 in 1998 (Object 24-10) (5) (the 1998 estimate of 61.3 deaths/100,000 in this report is for adults aged >25 years, and a 50% decrease would result in a goal of 30 deaths/100,000). The first goal, which is related both to the prevalence of COPD among adults and the proportion of those with activity limitation, seems achievable, although, as noted previously, persons with COPD might underestimate the amount of their activity limitation that is related to COPD. The second goal, given the continued high rates of COPD mortality in 1999 and 2000 and the aging of the population, will likely not be achieved if the current trends continue. The greatest challenge in COPD surveillance is related to the case definition for COPD. If one assumes that persons with moderate obstructive lung disease have clinically significant COPD, using chronic bronchitis in addition to emphysema to define COPD in surveys probably overestimates COPD among younger populations and underestimates it among older ones (Figure 1). Although the term COPD is increasingly being used by both patients and physicians, it is not typically used in health surveys. In addition, depending on physician diagnosis is problematic because COPD is frequently silent and, in the absence of spirometry, often undiagnosed (3). Even using spirometry, as in NHANES I and III, might result in the misclassification of conditions among certain persons who have short-term reversibility in their airway obstruction, because reversibility testing has not been done in national surveys in the United States. Finally, although we did not include asthma in this report, asthma and COPD can coexist and can be difficult to differentiate, chiefly among older populations (3). The continuing increase in COPD hospitalizations among men and women and the increase in COPD deaths among women is problematic and highlights the need for both clinical and public health interventions. Conversely, the decrease in COPD, as determined by pulmonary function testing, among persons aged <55 years, might indicate that tobacco-control efforts and other efforts to improve respiratory protection in recent years might be having a positive effect that will ultimately result in less COPD morbidity and mortality. References
Table 1 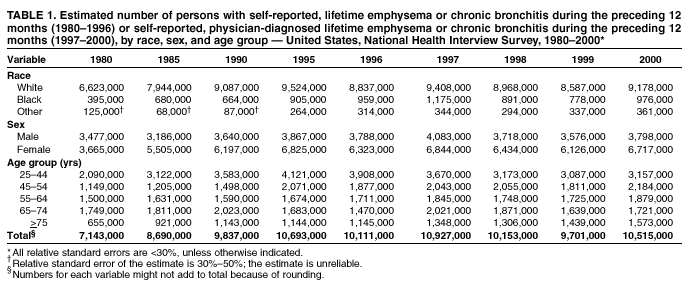 Return to top. Figure 1 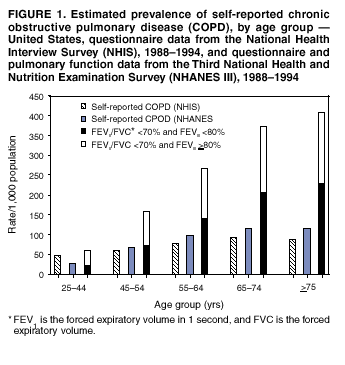 Return to top. Table 2  Return to top. Figure 2  Return to top. Table 3  Return to top. Figure 3 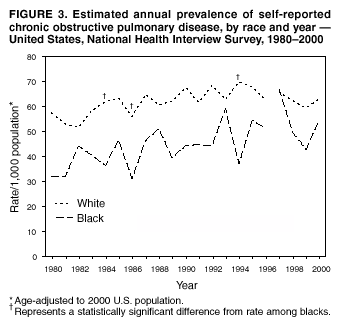 Return to top. Table 4  Return to top. Figure 4  Return to top. Table 5 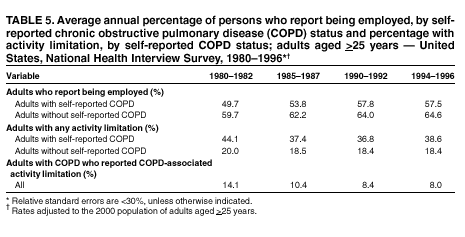 Return to top. Figure 5 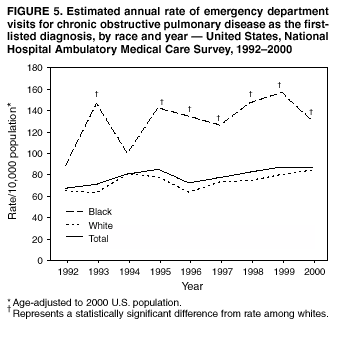 Return to top. Table 6  Return to top. Figure 6  Return to top. Table 7 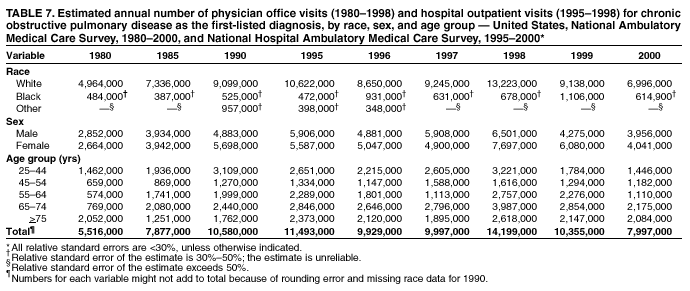 Return to top. Figure 7  Return to top. Table 8 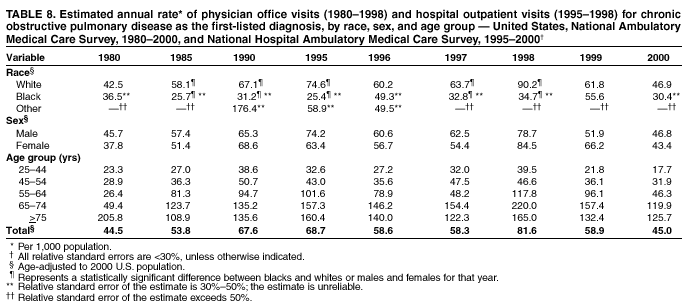 Return to top. Figure 8 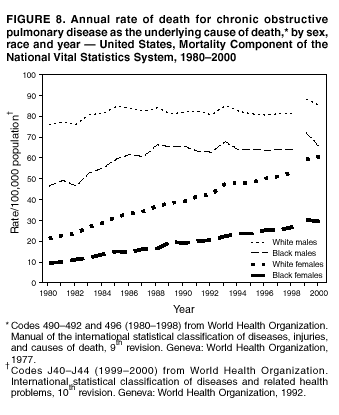 Return to top. Table 9 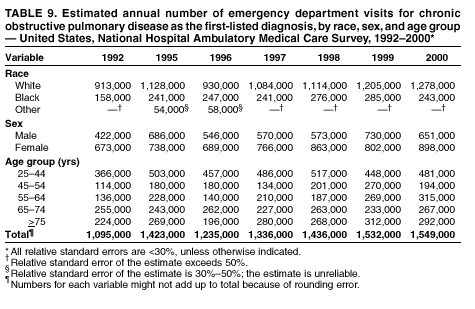 Return to top. Table 10 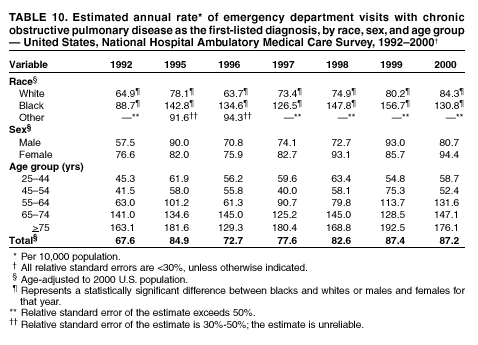 Return to top. Table 11 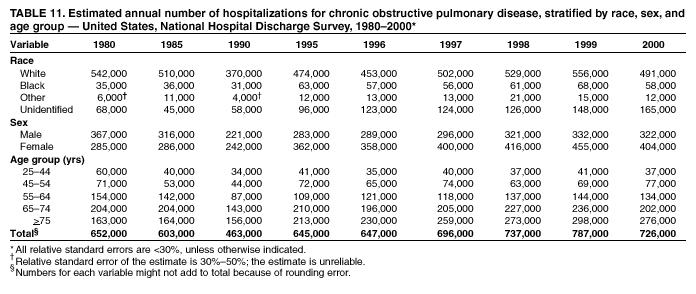 Return to top. Table 12  Return to top. Table 13  Return to top. Table 14 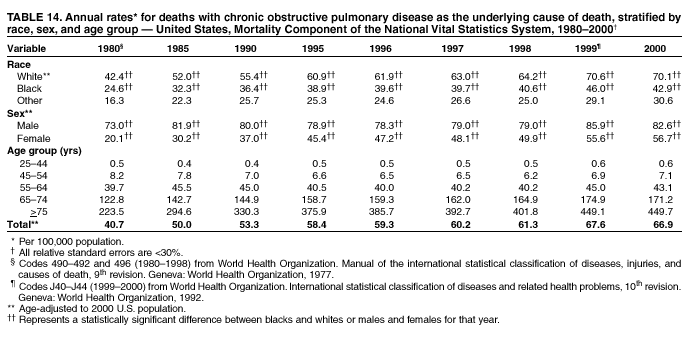 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 7/19/2002 |
|||||||||
This page last reviewed 7/19/2002
|