 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Pregnancy-Related Mortality Surveillance --- United States, 1991--1999Jeani Chang, M.P.H. Abstract Problem/Condition: The risk of death from complications of pregnancy has decreased approximately 99% during the twentieth century, from approximately 850 maternal deaths per 100,000 live births in 1900 to 7.5 in 1982. However, since 1982, no further decrease has occurred in maternal mortality in the United States. In addition, racial disparity in pregnancy-related mortality ratios persists; since 1940, mortality ratios among blacks have been at least three to four times higher than those for whites. The Healthy People 2000 objective for maternal mortality of no more than 3.3 maternal deaths per 100,000 live births was not achieved during the twentieth century; substantial improvements are needed to meet the same objective for Healthy People 2010. Reporting Period Covered: This report summarizes surveillance data for pregnancy-related deaths in the United States for 1991--1999. Description of System: The Pregnancy Mortality Surveillance System was initiated in 1987 by CDC in collaboration with state health departments and the American College of Obstetricians and Gynecologists Maternal Mortality Study Group. Health departments in the 50 states, the District of Columbia, and New York City provide CDC with copies of death certificates and available linked outcome records (i.e., birth certificates or fetal death certificates) of all deaths occurring during or within 1 year of pregnancy. State maternal mortality review committees, the media, and individual providers report a limited number of deaths not otherwise identified. Death certificates and relevant birth or fetal death certificates are reviewed by clinically experienced epidemiologists at CDC to determine whether they are pregnancy-related. Results: During 1991--1999, a total of 4,200 deaths were determined to be pregnancy-related. The overall pregnancy-related mortality ratio was 11.8 deaths per 100,000 live births and ranged from 10.3 in 1991 to 13.2 in 1999. The pregnancy-related mortality ratio for black women was consistently higher than that for white women for every characteristic examined. Older women, particularly women aged >35 years and women who received no prenatal care, were at increased risk for pregnancy-related death. The distribution of the causes of death differed by pregnancy outcome. Among women who died after a live birth (i.e., 60% of the deaths), the leading causes of death were embolism and pregnancy-induced hypertension. Interpretation: The reported pregnancy-related mortality ratio has substantially increased during 1991--1999, probably because of improved ascertainment of pregnancy-related deaths. Black women continued to have a 3--4 times higher pregnancy-related mortality ratio than white women. In addition, pregnancy-related mortality has the largest racial disparity among the maternal and child health indicators. Reasons for this difference could not be determined from the available data. Public Health Actions: Continued surveillance and additional studies should be conducted to monitor the magnitude of pregnancy-related mortality, to identify factors that contribute to the continuing racial disparity in pregnancy-related mortality, and to develop effective strategies to prevent pregnancy-related mortality for all women. In addition, CDC is working with state health departments, researchers, health-care providers, and other stakeholders to improve the ascertainment and classification of pregnancy-related deaths. IntroductionThe reduction of maternal mortality is one of the Healthy People 2010 objectives for the United States. This objective is a public health priority with the same goal as the Healthy People 2000 objective of no more than 3.3 maternal deaths per 100,000 live births (1--2). The risk of death from complications of pregnancy decreased substantially during the twentieth century, from 850 maternal deaths per 100,000 live births in 1900 to 7.5 in 1982, according to official U.S. vital statistics (3). However, this progress halted in 1982, and the mortality ratio has fluctuated between seven and eight maternal deaths per 100,000 live births since that time (4--5). In addition, a continuing disparity exists in the risk for pregnancy-related death between black women and white women. The pregnancy-related mortality ratios (pregnancy-related deaths per 100,000 live births) for black women are 3--4 times higher than for white women (6--10). Prevention of mortality attributable to pregnancy is a primary public health objective. Pregnancy complications remain an important concern for clinical medicine and for the health-care system. In 1987, CDC's Division of Reproductive Health, in collaboration with state health departments and the American College of Obstetricians and Gynecologists (ACOG) Maternal Mortality Study Group, established the Pregnancy Mortality Surveillance System (PMSS) (11). This system provides ongoing surveillance of all pregnancy-related deaths reported through individual state health departments, maternal mortality review committees, media, and individual providers. Therefore, PMSS permits increased precision in measuring the magnitude of pregnancy-related mortality and identifying the groups at increased risk of death than do systems relying on death certificate data alone. This report summarizes the analysis of identified pregnancy-related deaths in the United States during 1991--1999. MethodsPMSS collects data regarding all reported deaths that are causally related to pregnancy. The first step is to identify all deaths occurring during pregnancy or within 1 year of pregnancy. Methods used to establish this temporal relation between pregnancy and a death included 1) a pregnancy check box had been marked on the death certificate, 2) the death certificate had indicated that the woman was pregnant at the time of death, or 3) the death certificate of the reproductive-aged woman had been matched with a birth certificate or fetal death certificate for a delivery that occurred within 1 year before the woman's death. Health departments in the 50 states, the District of Columbia, and New York City voluntarily provided CDC with copies of death certificates that were causally related to pregnancy. For deaths that occurred after a live birth or stillbirth, the matching birth or fetal death certificates were also provided by the health departments. In addition to requesting certificates of deaths that are causally related to pregnancy, beginning with deaths occurring in 1991, states were asked to send certificates of all deaths that occurred during pregnancy or within 1 year of pregnancy, regardless of the cause of death or relation between pregnancy and the death. Pregnancy-related deaths occurring during 1991--1999 are reported because these are the most recent data available that have not been published previously in an MMWR Surveillance Summary. Data were coded after review of all available information from death certificates (including notes written on the margins of death certificates), maternal mortality review committee reports, autopsy reports, and matched birth and fetal death certificates. Matched birth certificates or fetal death certificates were available for the majority of women who delivered a live-born or stillborn infant. These certificates provided information not otherwise available on the death certificate (e.g., prenatal care and live birth order). Data concerning all deaths were reviewed and classified by clinically experienced medical epidemiologists at CDC regarding the immediate and underlying cause of death, associated obstetric conditions, and the outcome of pregnancy. In this report, a woman's death was classified as pregnancy-related if it occurred during pregnancy or within 1 year of pregnancy and resulted from 1) complications of the pregnancy, 2) a chain of events that was initiated by the pregnancy, or 3) the aggravation of an unrelated condition by the physiologic effects of the pregnancy or its management (11). Pregnancy-related mortality ratios were calculated by using the number of deaths obtained from the PMSS (numerator) and live-birth data (denominator) obtained from the 1991--1999 national natality files compiled by CDC's National Center for Health Statistics (12). This standard live-birth population included all women who delivered a live birth during 1991--1999. For both the numerator and the denominator of pregnancy-related mortality ratios, race was defined as the race of the mother and classified as white, black, or other. Other races included Asian/Pacific Islander, American Indian/Alaska Native, and those reported as other. All pregnancy-related deaths of women with unknown races (n = 19) were proportionally redistributed into known categories. Because of the limited number of pregnancy-related deaths in the other race category (n = 208), data regarding other race were not included for race-specific analyses. The women's ages at the time of death were grouped into standard 5-year intervals. Education information was obtained from either the death, birth, or fetal death certificates and was based on the total years of education completed at the time of death. The analysis of education was restricted to women aged >20 years, an age by which the majority of women would have had the opportunity to graduate from high school. The state of Georgia did not report maternal education during 3 years of the surveillance period (1997--1999); therefore, women who died in Georgia were excluded from analyses by education. Marital status was categorized as married (currently married) or unmarried (never married, divorced, separated, or widowed). Information concerning prenatal care and live-birth order were limited to women who delivered a live-born infant, because these data were not consistently available for women who had a stillbirth or abortion. Onset of prenatal care was categorized as initiation in the first, second, and third trimesters, or no prenatal care. Live birth order, defined as the number of live births including the index pregnancy in which the woman had delivered, was used as a proxy for parity. Time interval, defined as number of days between the end of pregnancy and maternal death, was calculated and used as a categorical variable. All analyses were performed by using SAS® software system (13). Logistic regression was based on maximum likelihood estimation methods and used to test the significance of the change in mortality ratios over time and to compute 95% confidence intervals and associated p values. However, because of the high number of live births in each year (approximately 4 million live births per year), a limited increase in the mortality ratio over time could lead to a statistically significant result. Ninety-five percent confidence intervals were provided for risk ratios by using the associated standard errors (14). Unless otherwise stated, all p values <0.05 were considered statistically significant. ResultsDuring 1991--1999, a total of 7,342 deaths were reported to PMSS. Of these, 2,919 deaths occurred during pregnancy or within 1 year of pregnancy but were not causally related to pregnancy. Although causally related to pregnancy, 106 deaths were excluded from this analysis because the time interval between the end of pregnancy and maternal death exceeded 1 year, and 117 deaths were excluded because whether the death was related to a pregnancy was unknown. The remaining 4,200 deaths were used as the basis for this analysis. A matched birth certificate was available for 93% of deaths that occurred after a live birth, and a matched fetal death certificate was available for 88% of deaths that occurred after a stillbirth. The overall pregnancy-related mortality ratio was 11.8 deaths per 100,000 live births for the 9-year surveillance period. The ratio significantly increased from 10.3 in 1991 to 13.2 in 1999 (p<0.001 for trend) (Figure 1). The pregnancy-related mortality ratio differed by maternal age; the risk for pregnancy-related death increased substantially among women aged >35 years (Table 1). Women aged >40 years had a pregnancy-related mortality ratio that was two times higher than that among women aged 35--39 years and approximately 4 times higher than women aged 30--34 years. Race was strongly associated with pregnancy-related mortality; black women were approximately four times more likely to die from pregnancy-related causes than were white women (Table 1). Race-specific pregnancy-related mortality ratios were higher for black women than for white women of all ages (Figure 2). In comparison with pregnancy-related mortality ratios for white women, excess risk for black women increased substantially with age and was most evident at aged >39 years (i.e., the ratio was 5.5 times higher for black women). Overall, the risk for pregnancy-related death among unmarried women was higher than that among married women (Figure 3). However, the pattern of this risk differed for black women and white women. The mortality ratio for black married women was higher than that for black unmarried women; the ratio was lower for white married women compared with white unmarried women. Overall, women who had >12 years of education had the lowest pregnancy-related mortality ratio. The risk for pregnancy-related death decreased with increasing levels of education among women aged 25--39 years (Figure 4). At all levels of education, pregnancy-related mortality ratios for black women were 3--4 times higher than ratios for white women. The most frequent pregnancy outcome associated with a pregnancy-related death was live birth (60%), followed by undelivered pregnancy (10%), and stillbirth (7%) (Figure 5). The outcome of pregnancy at the time of death was not known for 552 (13%) of the women. The only significant differences between black and white women in relation to pregnancy outcomes was the higher percentage of ectopic pregnancy (8%) among black women than among white women (4%) (p<0.001). Of women who died after a live birth, 4% had not received any prenatal care, and 24% had missing data regarding prenatal care. Mortality ratios for each trimester of prenatal-care initiation were 3--4 times higher for black women than for white women (Table 2). Overall, the pregnancy-related mortality ratio was 3--4 times higher among women who received no prenatal care compared with women who received any prenatal care. Women who received no prenatal care were more likely to have had >5 previous live births and have fewer years of education. Among women whose pregnancies resulted in a live birth, the risk for pregnancy-related death increased with increasing live-birth order (Table 2). For both white and black women, the pregnancy-related mortality ratios were approximately 2 times higher for women after the delivery of a fifth or higher live birth than for women after a first live birth. Overall, a three- to fourfold disparity exists in pregnancy-related deaths for black women compared with white women for each level of parity. The leading causes of pregnancy-related death were embolism (20%), hemorrhage (17%), and pregnancy-induced hypertension (16%) (Table 3). Although the percentages of all pregnancy-related deaths attributable to these causes have gradually decreased in the previous two decades, the percentage of deaths attributable to cardiomyopathy increased from 6% in 1991 to 9% in 1999. However, this increase was not statistically significant. Deaths attributable to other medical conditions have significantly increased from 14% in 1991 to 20% in 1999 (p<0.05). Deaths attributable to other medical conditions consist primarily of cardiovascular problems (34%), pulmonary problems (11%), and neurologic or neurovascular problems (7%). The leading causes of death differed by pregnancy outcome (Table 3). The leading causes of death among women who died after a live birth were embolism (21%), pregnancy-induced hypertension (19%), and other medical conditions (17%). Among women whose pregnancies ended in a stillbirth, the leading causes of death were hemorrhage (21%) (from abruptio placenta and uterine rupture), pregnancy-induced hypertension (20%), and infection (19%). Hemorrhage accounted for 221 (93%) of 237 deaths associated with ectopic pregnancies. Among women whose pregnancies ended in a spontaneous or induced abortion, infection was the cause of death for 34% of the women, followed by hemorrhage (22%) and other medical conditions (16%). Women who were still pregnant (undelivered) at the time of death most frequently died from other medical conditions (e.g. cardiovascular and neurologic problems) (34%) and embolism (25%), mostly thrombotic. Embolism, hemorrhage, and pregnancy-induced hypertension were the leading causes of death for both white and black women. The cause-specific, pregnancy-related mortality ratio was approximately 3--4 times higher for black women compared with white women for each cause of death. However, the risk for death as a result of cardiomyopathy and complications of anesthesia was 6 times higher for black women than for white women. Information regarding the time interval between the end of pregnancy and death was known for 3,378 (80%) of 4,200 maternal deaths. Of these, 1,160 (34%) women died within 24 hours after the end of their pregnancy; 1,845 (55%) deaths occurred during 1--42 days of pregnancy; and 11% died during 43--365 days. In addition, time interval varied by cause of death (Figure 6). Among women who died from embolism, the majority of deaths (52%) occurred within 24 hours after the pregnancy ended, and 68% of deaths attributed to hemorrhage occurred within 48 hours after the pregnancy ended. Of the 116 women who died as a result of cardiomyopathy, 45% died during 43--365 days after the end of pregnancy. DiscussionThe Healthy People 2000 and Healthy People 2010 objectives address the same goal for reducing maternal deaths to 3.3 maternal deaths per 100,000 live births (1--2). However, this goal was not met by the year 2000, and substantial improvement is needed to attain the goal by 2010. The pregnancy-related mortality ratios reported by the PMSS increased from 10.3 deaths per 100,000 live births in 1991 to 13.2 in 1999. This increase in the pregnancy-related mortality ratio probably reflects the enhanced ascertainment of cases for this surveillance system (e.g., increased use of linkages, pregnancy check boxes, and the new request to identify all deaths during pregnancy or within 1 year of pregnancy). Embolism, hemorrhage, and pregnancy-induced hypertension complications were the leading causes of pregnancy-related deaths during 1991--1999 (7). Although a substantial reduction in the percentage of deaths attributable to these causes has occurred during the previous two decades (9,15), the percentage of deaths attributable to cardiomyopathy and other medical conditions increased during the surveillance period (16). The increase in the number of cardiomyopathy-related deaths and deaths attributable to other medical conditions likely reflects improved ascertainment of pregnancy-related deaths by linking death certificates of women to live and stillbirths occurring within 1 year of the mother's death. The increasing number of deaths caused by other medical conditions might also be affected by changes in the age distribution of women giving birth. Women in the United States are becoming pregnant at older ages, and the prevalence of chronic medical conditions increases with age (17--18). In addition, older women are at increased risk for pregnancy-related death (7--10) and adverse reproductive health outcomes, particularly women aged >35 years (17,19). Pregnancy-related mortality ratios continued to be 3--4 times higher for black women than for white women (6--10). In addition, the pregnancy-related mortality ratios for black women aged >39 years were particularly high in comparison with white women in the same age group (7,19). The risk for pregnancy-related death resulting from cardiomyopathy and complications of anesthesia were both approximately 6 times higher for black women than for white women. Among women aged >20 years, higher levels of education were associated with decreasing pregnancy-related mortality ratios; however, pregnancy-related deaths for black women were 3--4 times higher than that for white women at any education level. Although the overall risk for pregnancy-related death was higher among unmarried women than among married women, this association varied by race. Black married women had a higher mortality ratio than black unmarried women, and the inverse was observed for white women. Of all maternal deaths that occurred after a live birth, 56% of the women received early prenatal care (i.e., during the first trimester) as recommended (20), but 4% received no prenatal care at all. Overall, women who received any prenatal care have a lower risk for pregnancy-related mortality in comparison with women who received no prenatal care. Pregnancy-related mortality ratios for black women were higher at each level of prenatal-care initiation than ratios for white women. In addition, the reduction in mortality ratios among women who received prenatal care compared with women who received no prenatal care was higher among white women than among black women. Differences exist, by race, in the content of prenatal care for black women and white women (21--24); black women often receive fewer services and insufficient health-promotion education during their prenatal visits (24--27). However, the relation between these prenatal care indicators (i.e., content of prenatal care and number of visits) and pregnancy-related mortality is not clear. The characteristics evaluated in this report confirmed the racial disparity in pregnancy-related deaths, but the reasons for disparities could not be determined from the available data. Whether the racial disparity might be related to differences in the seriousness of morbidity, differences in diagnosis and treatment of pregnancy-related complications, or a combination of these factors is unclear. These factors, although not measurable through routine surveillance, probably contributed to the increased risk for pregnancy-related death among black women. Race might also serve as a marker for other sociodemographic risk factors and cultural differences (28--30). However, the sources from which data were obtained for this surveillance system had limited information concerning sociodemographic indices, family and community conditions, and other factors that might be associated with the differences in pregnancy-related mortality between black and white women. LimitationsLimitations should be considered in the analysis of pregnancy-related mortality during 1991--1999. Although ascertainment methods have improved, pregnancy-related deaths were undetected (9,16,31--35). Because this report is based on data provided voluntarily by state health departments in the 50 states, the District of Columbia, and New York City (which registers births and deaths separately from New York state), methods used to identify death certificates differed by reporting area. For 1991--1998, the majority of reporting areas identified deaths by the International Classification of Diseases, Ninth Revision (ICD-9), codes 630--676 (36). Beginning in 1999, the International Classification of Diseases, Tenth Revision (ICD-10), was used; however, the use of ICD-10 has not been fully implemented by all reporting areas. Seventeen reporting areas include a check box on their death certificate to indicate whether pregnancy had recently occurred (37). The inclusive time interval (i.e., interval between the end of pregnancy and death) used in the check box is inconsistent and varies by state, from 42 days to 18 months. Using a check box has been helpful for health departments to identify additional deaths that occurred during a specified time frame (37). However, death certificates ascertained by check box alone did not contain enough information to establish that a causal relation also existed between pregnancy and death. In addition, the increased use of linkages of death certificates of women of reproductive age to live birth or fetal death records occurring within the year before death substantially improves ascertainment of pregnancy-related deaths associated with live-birth or fetal-death outcomes (16,31- -33,38). However, this linkage of vital records does not identify pregnancy-related deaths that do not generate a record of pregnancy outcome (e.g., ectopic pregnancies and undelivered events) (39). Although having the matched birth or fetal death certificates with maternal death certificates improved the quality and quantity of the available information regarding the pregnancy-related deaths, the assessment of circumstances leading to pregnancy-related death was limited by the absence of detailed clinical data. Pregnancy-related death encompasses a complex combination of etiologies and pregnancy outcomes, and the underlying risk factors associated with death vary with cause of death and pregnancy outcome. A more accurate classification can be made if the medical information (the lower section of the birth record) is included, but this information is not consistently provided. In addition, certain states are now providing to CDC computer-generated reports that do not include details needed to optimally classify deaths. However, CDC is working with state health departments, researchers, health-care providers, and other stakeholders to improve the ascertainment and classification of pregnancy-related deaths. Public Health MeasuresAlthough deaths attributable to pregnancy are rare, each death needs to be identified and carefully reviewed at the state level. To accurately identify causes of pregnancy-related mortality in the United States, complete and consistent reporting is needed (40). Additional sources of data, including review of the medical and social circumstances of the death, are necessary to understand the effects of medical care, socioeconomic status, access to and content of prenatal care, social environment, and lifestyle on the sequence of events that lead to pregnancy-related deaths. The continuing disparity in pregnancy-related mortality between white and black women indicates the need to identify the differences that contribute to excess mortality among black women. Specific interventions should be developed to reduce pregnancy-related mortality, especially among black women. Pregnancy-related deaths are underreported, and the true number of deaths related to pregnancy might increase from 30%--150% with active surveillance (16,31--33). Therefore, improved surveillance and additional research are needed to assess the magnitude of pregnancy-related deaths, further identify potential risk groups, and investigate the causal pathway that led to the death (41). The use of ICD-10 and the revised death certificate will assist in identifying additional maternal deaths. The proposed revision includes a pregnancy check box as a standard element with designated time intervals between the end of pregnancy and death to more effectively identify deaths that are potentially associated with pregnancy. This report provides results from a national population-based data set with sufficient numbers to examine trends and major risk factors for pregnancy-related mortality. It provides information that is needed to develop effective strategies to prevent pregnancy-related mortality for all women. Acknowledgments The authors acknowledge William Callaghan, M.D., for assisting with the review and classification of cases, Gary Jeng, Ph.D., for his statistical consultation, and Elizabeth Fitch for her graphic assistance, National Center for Chronic Disease Prevention and Health Promotion. In addition, the authors acknowledge state health departments, the District of Columbia, and New York City for reporting data to CDC. References
Table 1  Return to top. Figure 1 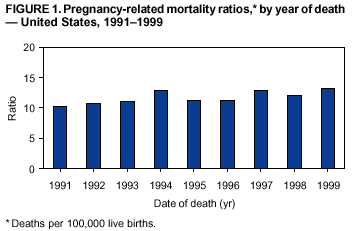 Return to top. Table 2 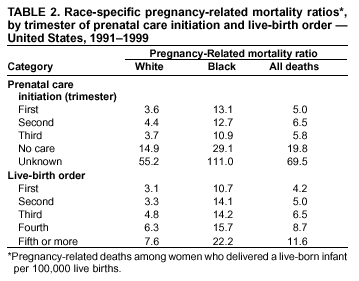 Return to top. Figure 2 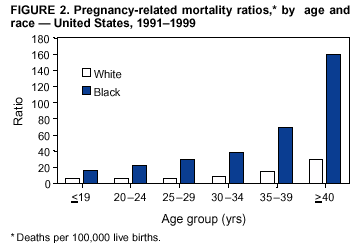 Return to top. Table 3 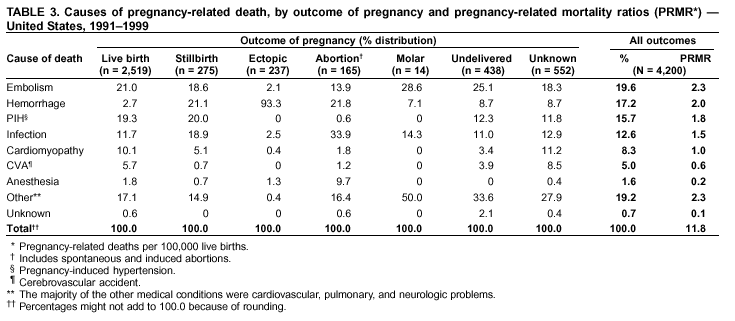 Return to top. Figure 3 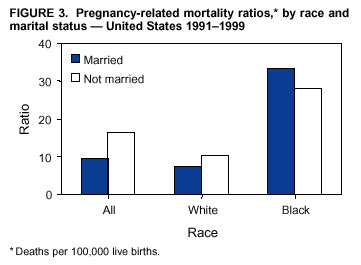 Return to top. Figure 4 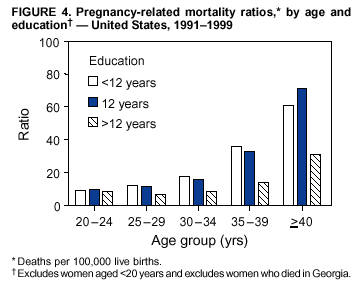 Return to top. Figure 5 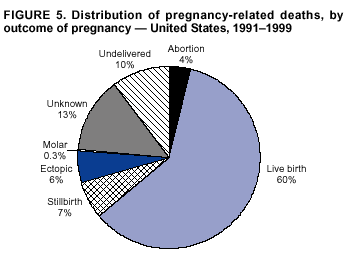 Return to top. Figure 6 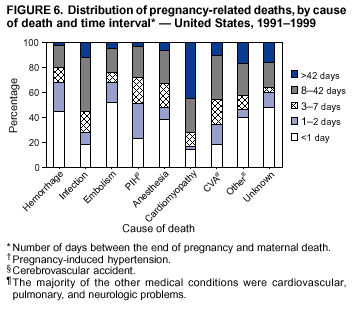 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 2/4/2003 |
|||||||||
This page last reviewed 2/4/2003
|