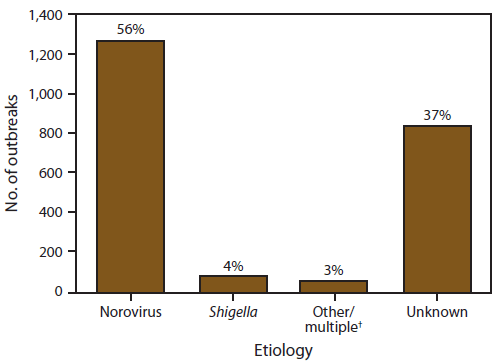
FIGURE 4. Number* and percentage of outbreaks of acute gastroenteritis transmitted by person-to-person contact, by confirmed etiology — National Outbreak Reporting System, United States, 2009–2010
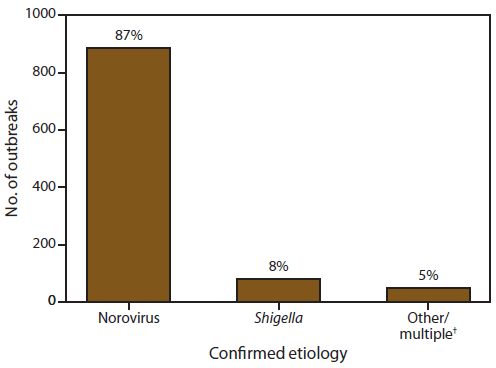
* N = 1,016.
† Includes Salmonella enterica (n = 16), STEC (n = 9), rotavirus (n = 7), Giardia lamblia (n = 4), Cryptosporidium spp. (n = 4), Clostridium difficile (n = 3), sapovirus (n = 2), Campylobacter jejuni (n = 1), norovirus and Clostridium difficile (n = 2), norovirus and Bacillus sp. (n = 1), and norovirus, rotavirus, and Clostridium difficile (n = 1).
Alternate Text: This figure is a bar graph that presents the number and percentage of confirmed etiologies of acute gastroenteritis transmitted by person-to-person contact.
 ShareCompartir
ShareCompartir