 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Syphilis Among Men Who Have Sex With Men ---Southern California, 2000Syphilis is a sexually transmitted disease (STD) caused by infection with the spirochete Treponema pallidum, and like other genital ulcer diseases, syphilis enhances the transmission of human immunodeficiency virus (HIV) (1). During the 1990s, syphilis occurred predominantly among heterosexual blacks in the South and in large cities. However, recent outbreaks of syphilis have occurred among men who have sex with men (MSM) (2,3). A large syphilis outbreak occurred among MSM during January--July 2000 in southern California. During the outbreak period, the proportion of primary and secondary (P&S) syphilis cases among MSM increased to 51% from 26% for the same period in 1999. This report summarizes the findings of an investigation of this syphilis outbreak, which indicate a substantial increase in the number of syphilis cases among MSM, many of whom are HIV-positive. These data suggest that concern about HIV infection may be declining among MSM and emphasize the importance of strengthening efforts to prevent HIV infection in this population in the United States. California law requires that reactive syphilis serologic results and suspected cases of syphilis be reported to local health departments. Suspected and confirmed syphilis cases are then reported to the California Department of Health Services and CDC. Public health staff interview all persons with syphilis to collect clinical, demographic, and epidemiologic data and to assure that these persons receive appropriate treatment. The behavioral data collected include sex and number of sex partners, self-reported HIV serostatus, drug use, and location where the patient had met sex partners while the patient probably was infected. Because of the increase in the number of reported cases of syphilis in 2000, staff re-evaluated and reinterviewed syphilis case-patients reported during January 1999--July 2000. Case-patients were defined as persons with a reactive syphilis serologic test result and symptoms of P&S syphilis. Men were identified as MSM if they reported having had any male sex partners during the interview period. During January--July 2000, 130 case-patients were reported, 66 (51%) of whom were MSM compared with 26 (26%) of 100 for the same period in 1999 (Figure 1) (4). Of the 66 MSM case-patients, 15 (23%) had primary syphilis, and 51 (77%) had secondary syphilis. MSM case-patients were from the following health jurisdictions: Los Angeles County (41), Orange County (10), City of Long Beach (eight), San Diego County (six), and Riverside County (one). Overall, 47% of cases were diagnosed at private medical clinics, 18% at HIV early intervention programs, and 17% at STD clinics. The median age of MSM case-patients was 35 years (range: 20--54 years); 27 (41%) were white, 24 (36%) were Hispanic, 12 (18%) were black, and two (3%) were Asian/Pacific Islander; race/ethnicity was unknown for one (2%). Of the 57 who knew their HIV serostatus, 34 (60%) reported that they were HIV positive. The year of diagnosis was known for 27 of the 34 HIV-positive MSM; the median time since diagnosis of HIV infection was 4 years (range: 0--19 years). For those whose HIV diagnosis had been made <1 year before the diagnosis of syphilis, the number of months since HIV diagnosis was not available. Although data on behavioral risks were not collected systematically, interview records indicate that of the 66 MSM, 33 (50%) reported that they had had anonymous sex, 17 (26%) had met sex partners in bathhouses, two (3%) had met sex partners through the Internet, and four (6%) had had sex with a commercial sex worker. Overall, 13 (20%) MSM reported using a condom during the most recent sexual contact, and 26 (40%) reported using illicit drugs. Crystal methamphetamine, the drug reported most frequently, had been used by 18%. Local response to the outbreak included a media campaign, community education, outreach, and syphilis screening. The media campaign used radio, print, and Internet advertisements to raise awareness of the outbreak and to promote syphilis testing. Local health departments and community groups used mobile vans to conduct syphilis screening at bathhouses, gay bars, HIV treatment sites, and other locations (e.g., parks and selected street corners) that MSM case-patients had identified as places for meeting sex partners. Reported by: KT Bernstein, ScM, R Tulloch, J Montes, MA, G Bolan, MD, Sexually Transmitted Disease Control Br, California Dept of Health Svcs; IE Dyer, MPH, M Lawrence, MPA, AP Kaur, MPH, D Kodagoda, MPH, H Rotblatt, P Kerndt, MD, Los Angeles County Sexually Transmitted Disease Program, Los Angeles; R Gunn, MD, County of San Diego Sexually Transmitted Disease Program, San Diego; N DeAugustine, Preventive Health Bur, City of Long Beach Dept of Health and Human Svcs, Long Beach; P Weismuller, DrPH, Orange County Sexually Transmitted Disease Program, Orange County, California. Div of Sexually Transmitted Disease Prevention, National Center for HIV, STD, and TB Prevention; and EIS officers, CDC. Editorial Note:The results of this investigation and other similar outbreaks suggest that an increasing number of MSM are participating in high-risk sexual behavior that places them at risk for syphilis and HIV infection (5,6). Similar trends have been reported internationally (7). These data are consistent with reports from behavioral surveys that indicate some MSM are participating in activities that increase their risk for acquiring and transmitting HIV and other STDs (8). Several factors may have contributed to this change, including the availability of highly active antiretroviral therapy (HAART) (9). Since the introduction of HAART in 1996, acquired immunodeficiency syndrome incidence and deaths have declined substantially, decreasing the actual and perceived threat of HIV to MSM (8). Because syphilis increases the likelihood of acquiring and transmitting HIV infection, the increase in P&S syphilis among MSM may indicate an increase in the incidence of HIV infection. The findings in this report are subject to at least two limitations. First, information was abstracted from public health records for which data had not been collected systematically because of variations in interview style and documentation. Second, because behavioral risk data were available only for some case-patients, the proportion of case-patients with each reported behavioral risk may be inaccurate. A high proportion of cases was identified by private providers, and communication between public health officials and HIV care and local primary-care providers was crucial in responding to the outbreak. The standard of care for MSM, regardless of HIV status, should continue to include counseling about safer sex. For MSM who are HIV positive or are at risk for HIV, voluntary screening for syphilis and other STDs is an essential component of quality care. MSM who do not know their HIV serostatus and who have an STD should be offered HIV screening to facilitate early access to care for those who are HIV positive. Partnerships with clinicians and community organizations that serve MSM will continue to be critical for the development of targeted and effective prevention messages. In this outbreak, community organizations and state and local health departments facilitated rapid outreach and education in the community. The role of outreach efforts and the media campaign in arresting the outbreak is being evaluated. This outbreak, unlike other recent syphilis outbreaks (10), involved primarily white and Hispanic MSM with access to health care, most of whom were HIV positive. As syphilis rates decline and the epidemiology of syphilis changes, outbreak recognition through surveillance and the collection of enhanced behavioral risk data will be important in preventing syphilis and HIV transmission. State and local health departments should review HIV/STD and behavioral surveillance data on MSM and other at-risk populations to detect outbreaks and implement appropriate public health actions. Increased prevention efforts in MSM communities are critical in preventing STD and HIV transmission. References
Figure 1 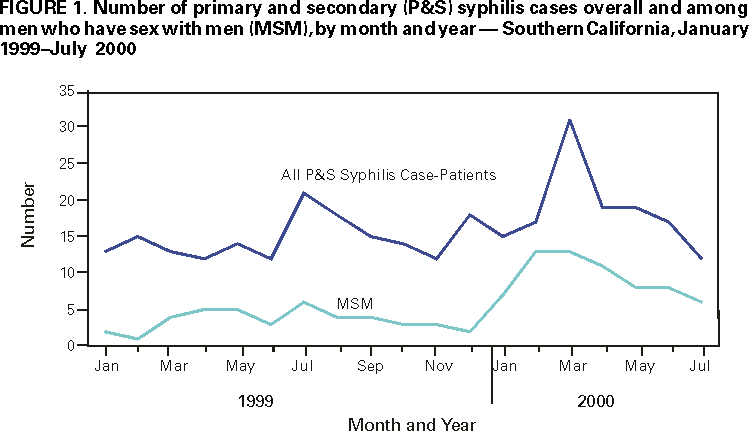 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 2/22/2001 |
|||||||||
This page last reviewed 5/2/01
|