 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Lower Extremity Amputation Episodes Among Persons with Diabetes --- New Mexico, 2000Lower extremity amputation (LEA) is one of the most disabling complications of diabetes (1). Lower extremity problems tend to recur among persons because of underlying complications, including the loss of "protective" sensation (2,3). To define the burden of LEA among persons with diabetes in New Mexico, the New Mexico Diabetes Prevention and Control Program (DPCP) analyzed data from the Hospital Inpatient Discharge Database (HIDD) and the Santa Fe Indian Hospital (SFIH) from 2000 by linking hospital discharges to persons to create "episodes" of LEA. This report summarizes the findings of that analysis, which indicated that the age-adjusted rate of LEA by episode was approximately 3.5 times higher for American Indians (AIs) (11.4 per 1,000 persons with diabetes) than for non-Hispanic whites (3.3). To address this disparity, DPCP is collaborating with the Indian Health Service (IHS) to determine the needs for foot-care resources and education in AI communities. HIDD is maintained by the New Mexico Health Policy Commission and includes data on discharges from all nonfederal licensed hospitals in the state. Persons with at least one discharge from a hospital in which a nontraumatic LEA (International Classification of Diseases, Ninth Revision, Clinical Modifications [ICD-9-CM] codes 84.10--84.19) was performed during 2000 were identified; traumatic LEA codes 895--897 were excluded. Diabetes-related LEA discharges were identified by ICD-9-CM codes 250.0--250.9 listed at the time of LEA or any other hospitalization during the calendar year. Discharges were linked by unique identifiers, allowing analyses at the individual level to distinguish between persons who had LEA hospitalizations for treatment of the same lesion and persons who had a new and potentially preventable lesion. For multiple discharges, an interval between discharge and readmission of <14 days was considered a single episode; an interval of >14 days was considered a separate episode. For persons with multiple LEAs within an episode, the highest level of amputation was used; LEAs were categorized as minor (i.e., at or below the foot) or major (i.e., above the foot). These same methods were used with discharge data provided by SFIH, a federal hospital operated by IHS, to supplement HIDD data. HIDD does not include LEAs performed at IHS hospitals. Race/ethnicity of patients in HIDD was self-reported to hospitals. All patients from SFIH were classified as AIs. The number of persons with diabetes at risk for LEA in 2000 was estimated by multiplying race/ethnicity-specific prevalence rates from the Behavioral Risk Factor Surveillance System (BRFSS) by the appropriate New Mexico adult population for that year according to the U.S. Bureau of the Census. BRFSS is a state-based, random-digit--dialed telephone survey of the noninstitutionalized U.S. population aged >18 years. Because the sample size of AIs in BRFSS is small, estimates of AIs with diabetes were based on IHS outpatient data for the same year. The IHS outpatient database contains clinical and demographic information from IHS and tribal health-care facilities in New Mexico. Unique patient identifiers were used to exclude duplicate records, and geographic location was determined according to where patients received services most recently. BRFSS data for 1998--2000 were aggregated to estimate the age-specific diabetes prevalence for non-Hispanic whites and Hispanics. Age adjustment was performed by using the direct method and the 2000 U.S. standard population (4). In 2000, a total of 307 persons with diabetes had 354 LEA episodes; 265 persons had a single episode and 42 had two or more episodes. The median age of persons was 66 years (range: 28--92 years) (95% confidence interval [CI] = 64.6--67.4). Among the episodes, 193 (55%) were minor, and 161 (45%) were major. The incidence of LEA was twice as high for men as for women (4.5 episodes per 1,000 persons with diabetes versus 2.1; p<0.05) and increased with age (Table). The age-adjusted LEA rate was 3.5 times higher for AIs than for non-Hispanic whites (11.4 versus 3.3; p<0.05). The difference in rates was not statistically significant for non-Hispanic whites and Hispanics (3.3 versus 2.6). Overall, the age-adjusted LEA rate was 3.4 per 1,000 persons with diabetes (95% CI = 2.9--3.9). Reported by: H Krapfl, MS, D Gohdes, MD, New Mexico Dept of Health. NR Burrows, MPH, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:Approximately one third of persons with diabetes are at high risk for LEA (2,3). Risk factors for LEA include having had a previous ulcer or amputation. Foot ulcers usually precede amputation and are caused by several underlying problems, including neuropathy and reduced circulation, which lead to injury and poor healing (1). LEA surveillance is conducted typically by analyzing hospital discharges without knowing how many persons are represented (5--8). Conducting surveillance of LEAs at the individual level helps to monitor the success of LEA prevention efforts. Similar to other studies of LEA among persons with diabetes, the findings in this report indicate that the rate of LEA is higher among men than among women (5--8) and higher among non-Hispanic whites than among Hispanics (5). AIs had the highest rate of LEAs among the groups analyzed. Age-adjusted rates of LEA found in this analysis were lower than those reported previously in other areas (5,6,8) because persons with multiple discharges were counted only once. The findings in this report are subject to at least six limitations. First, the number of LEA discharges and persons undergoing LEAs probably were underestimated because Veterans Health Administration data, which contain a high percentage of persons aged >65 years with a high prevalence of diabetes, and complete IHS data could not be obtained. However, only two additional IHS facilities exist that perform LEAs in New Mexico. Second, race/ethnicity for 24 persons in HIDD were classified as "unknown" or "other", which could influence LEA rates among racial/ethnic groups. Third, the number of procedures that occurred among persons with diabetes might have been underestimated because coexisting diabetes was not always coded on hospital discharge records. Fourth, denominator data were based on a self-reported diagnosis of diabetes; however, diagnosis of diabetes has been reported accurately in BRFSS (9). Because this denominator data were based on telephone surveys and some areas in New Mexico have low telephone coverage, these areas were underrepresented in BRFSS. Fifth, because of the small sample size of AIs in BRFSS, IHS outpatient data were used to determine diabetes prevalence among AIs. Using survey and outpatient data might introduce some bias; however, this bias does not account completely for the large difference in rates between AIs and other racial/ethnic groups because of the likely underestimation of LEAs among AIs. Finally, the definition of an episode for a person readmitted <14 days of the initial hospitalization might be arbitrary because surgical philosophies differ regarding how much healing time should be allowed before further amputation. However, in the absence of data, 14 days was considered a conservative time interval for a lesion to heal, and the majority of repeat hospitalizations within 14 days probably were related to the original lesion. Regular comprehensive foot examinations are important for early detection of foot problems, and efforts to prevent recurring problems can be effective in reducing the number of persons with diabetes who undergo LEA (1). The New Mexico DPCP collaborates with health-care providers and professionals to provide standardized practice guidelines and provider education in several areas related to diabetes, including foot care. During this process, DPCP has become a key partner in "New Mexico Healthcare Takes on Diabetes," a broad collaborative effort of New Mexico's health-care professionals, health plans, and the New Mexico Medical Review Association. Radio messages on foot care also are broadcast in English, Spanish, and Navajo. As a result of the findings of this study, DPCP is collaborating with the Albuquerque Area IHS. A survey of AI communities was conducted on various topics, including 1) level of knowledge about foot care among health-care providers, community health representatives, and patients; 2) access to a podiatrist; and 3) barriers encountered in providing foot care. As part of this process, DPCP is exploring surveillance at other IHS facilities. Continued surveillance of LEA episodes will be useful in expanding and tailoring future interventions and in tracking the success of prevention efforts. References
Table 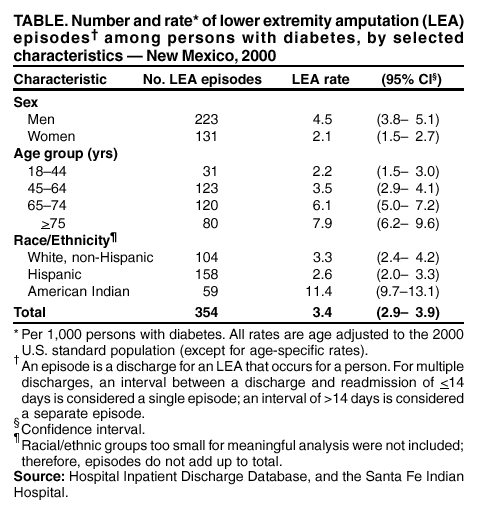 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 1/30/2003 |
|||||||||
This page last reviewed 1/30/2003
|