 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Methicillin-Resistant Staphylococcus aureus Infections in Correctional Facilities --- Georgia, California, and Texas, 2001--2003Infections caused by methicillin-resistant Staphylococcus aureus (MRSA) (Figure) are common in hospitals and nursing homes. Because MRSA is resistant to all commonly prescribed beta-lactam antibiotics (e.g., penicillins and cephalosporins), these infections require treatment with alternative antimicrobial drugs. In addition, because antimicrobial drugs usually must be selected before identifying MRSA as the cause of infection, treatment presents a challenge for clinicians. MRSA has emerged recently as a more frequent cause of skin and soft tissue infections in the community, particularly in correctional facilities such as prisons, jails, and detention centers (1--3). This report summarizes recent investigations of MRSA transmission among inmates of correctional facilities in Georgia, California, and Texas. Inadequate personal hygiene, barriers to medical care, and other factors contributed to transmission. Information from these investigations has been used in the development of recently released Federal Bureau of Prisons guidance for control of MRSA (4), which recommends improvements in inmate hygiene, infection control, and targeted antimicrobial treatment. Case DefinitionFor the investigations described in this report, a confirmed case of MRSA infection was defined as illness, compatible with staphylococcal disease, in an inmate with laboratory evidence of MRSA from culture of tissue or blood. A possible case of MRSA was defined as an illness, compatible with staphylococcal infection, in an inmate who had an epidemiologic link to a laboratory-confirmed case but did not have cultures performed. A case of MRSA infection was defined as invasive if MRSA was isolated from cultures of a normally sterile site such as blood or cerebrospinal fluid. GeorgiaSince 2001, the Georgia Division of Public Health has assisted the Georgia Department of Corrections (GDC) and local health departments with three investigations of MRSA skin infection outbreaks in three different types of correctional facilities. These investigations are described below. Investigation 1. During June--September 2001, a total of 11 cases of MRSA skin infections were identified in an all-male, 200-bed, minimum-security state detention center with an average incarceration duration of 90 days. Of the 11 inmates, five had repeated MRSA skin infection occurring after the initial lesion (i.e., recurrent disease). A case-control study identified prolonged (>36 days) incarceration and outdoor work duty as risk factors for MRSA infection. Other possible risk factors included inadequate wound care by medical staff and limited access to soap for hand washing and general bathing (soap was locked in inmate cells away from sinks and showers). In response to this outbreak, the detention center implemented facility-wide screening for skin disease, standardized antimicrobial treatment recommendations, inmate education, and introduction of alcohol-based hand rubs. During December 2001--May 2002, no MRSA cases occurred; however, during June--November 2002, a total of 14 cases were reported. Staff reviewed previous recommendations for hygiene education with inmates and reinforced proper wound care and antimicrobial use. Chlorhexidine-containing soap was provided daily for 3 days among the entire inmate population. During December 2002--April 2003, five cases of MRSA occurred. Investigation 2. During April--July 2002, a total of 11 cases of MRSA were reported from a 1,500-bed, maximum-security state prison with an average incarceration duration of 591 days. Infections ranged from small furuncles to deeper abscesses; no deaths or bacteremias occurred, and no inmates were hospitalized. A case-control study identified risk factors, including previous antimicrobial use, self-draining of boils, skin laceration (intentional or accidental), washing clothes by hand, sharing soap, and recent arrival at the prison (since 2001). On the basis of these findings, the prison implemented appropriate laundering, improved access to wound care, increased availability and quantity of soap, and began inmate hygiene education. Monitoring of MRSA infections from the beginning of the outbreak in April 2002 until February 2003 identified 73 inmates with infection, 10 of whom had recurrent disease. During July--August 2002, a total of 23 cases of MRSA occurred in 19 inmates. Interventions were implemented during late July--August; however, six cases of MRSA occurred among inmates during September--October. In response, in February 2003, the prison housed a cohort of MRSA-infected inmates separately and provided a 5-day supply of chlorhexidine-containing soap for personal hygiene. Despite these measures, during March--May 2003, an additional 29 cases of MRSA were reported. GDC and prison staff are working to improve implementation of recommended interventions for preventing additional cases of MRSA among inmates. Investigation 3. During June--October 2002, a 2,800-bed county jail with an average incarceration duration of 25 days identified 13 cases of skin lesions, initially thought to be spider bites, from which MRSA was isolated. Three inmates were hospitalized for wound care. A retrospective chart review identified 16 cases and 29 possible cases of MRSA skin infections that had occurred during this period. Infections included folliculitis, furunculosis, and abscess. In December, the jail implemented screening for active skin lesions among the inmates, standardized treatment protocols including treatment with non--beta-lactam antibiotics for suspected S. aureus infections, hygiene education for inmates, and changes in laundry practices. Through increased use of bacterial cultures to evaluate skin infections, 59 additional MRSA cases were identified during February--April 2003. A review of medical records of 50 patients who received antimicrobials identified 13 (26%) instances in which beta-lactam antimicrobials were used inappropriately for nine (18%) inmates treated before culture results and for four (8%) inmates treated after results indicated culture-confirmed MRSA. Los Angeles County, CaliforniaThe Los Angeles (LA) County jail system, the largest in the country, houses an estimated 20,000 inmates daily and has an average duration of incarceration of 44 days. After an increase in reports of spider bites, the jail developed a protocol in September 2001 that included culture of any lesions suspected to be spider bites. The LA County Department of Health Services (LACDHS) was notified after MRSA was found as the cause of many "spider bite" lesions (2). In 2002, a total of 921 MRSA skin infections were identified; 726 (79%) inmates had data available for review. The median time from incarceration to MRSA culture was 45 days (range: 1--1,160 days); 65 (9%) MRSA cases were identified within 5 days after incarceration. During January--June 2003, a total of 776 inmates with MRSA infections were identified (14% identified within 5 days after incarceration), yielding 1,697 cases reported since the jail began surveillance for skin lesions. Investigators observed inadequate infection-control measures in the clinic area; enhanced administrative controls were necessary to ensure frequent showering and appropriate personal hygiene for inmates. LACDHS recommended improvements for skin lesion surveillance, standardized treatment protocols including empiric treatment with non--beta-lactam antimicrobials for all wound infections, hygiene education for inmates, environmental cleaning, and increased frequency of laundry changes. Improvements in antimicrobial treatment of MRSA infections have occurred; however, other recommendations have yet to be implemented fully. TexasThe Texas Department of Criminal Justice (TDCJ) operates 105 facilities housing 145,000 inmates. In 1996, TDCJ implemented a comprehensive set of treatment and prevention guidelines for MRSA skin infections that included six components: 1) surveillance, 2) hygiene education for inmates, 3) access to proper wound care, 4) standardized antimicrobial therapy based on drug susceptibility data (including directly observed therapy), 5) early treatment of skin disease, and 6) eradication of MRSA from asymptomatic carriers who have recurrent MRSA infections. Since 1998, TDCJ has required culturing of all draining skin lesions and reporting of results to the TDCJ Office of Preventive Medicine. The proportion of S. aureus infections that were methicillin-resistant increased from 24% (864 of 3,520) in 1998 to 66% (5,684 of 8,633) in 2002. In December 2000, a case-control study (16 cases and 32 controls) was performed for all cases of MRSA identified during November 2000 at the correctional system's largest intake facility. The study identified previous skin infections and recent close contact with an MRSA-infected inmate as risk factors for infection. Of 10,942 cases of MRSA reported from the beginning of surveillance during January 1996--July 2002, a total of 189 (1.7%) were invasive. The remainder were either unknown site (397 [3.6%]) or skin and soft tissue infections (10,356 [94.6%]). During 1999--2001, three deaths were attributed to MRSA infections. Skin infection screening at the time of incarceration was added to the guidelines in 2003. Implementation of guidelines and a continued multidisciplinary approach to MRSA infections has not led to substantial decreases in the incidence of MRSA. Additional interventions and their effects on infection and carriage are being evaluated, and barriers to efficient implementation of the guidelines are being investigated. Reported by: M Tobin-D'Angelo, MD, K Arnold, MD, S Lance-Parker, DVM, Georgia Div of Public Health; M LaMarre, Office of Health Svcs, Georgia Dept of Corrections. E Bancroft, MD, A Jones, MPH, A Itano, MPH, M Chambers, MD, L Mascola, MD, Los Angeles County Dept of Health Svcs; J Clark, MD, M Tadesse, Los Angeles County Jail, Los Angeles, California; M Kelley, MD, Texas Dept of Criminal Justice; N Pascoe, Texas Dept of Health. M Kuehnert, MD, S Fridkin, MD, D Jernigan, MD, Div of Healthcare Quality Promotion, National Center for Infectious Diseases; E Beltrami, MD, Epidemiology Program Office; SH Wootton, MD, B Coignard, MD, EIS officers, CDC. Editorial Note:The investigations described in this report identified four factors that contributed to spread of MRSA among inmates. First, investigators identified barriers to routine inmate hygiene. Access to soap often was limited or was restricted for security reasons, and new alcohol-based hand rubs were difficult to introduce because of misuse of these products. Mental health and behavior problems among inmates might have contributed to poor adherence and hindered efforts to improve hygiene. Inmates' clothing was washed by hand or in bulk loads, and potentially contaminated laundry might not have undergone sufficiently high water temperatures or drying to eliminate bacteria. Second, proper access to medical care was hindered by co-payments required for acute care visits and by inadequate supplies and staff for wound care. Third, frequent medical staff turnover was a challenge to providing education on proper infection-control procedures. Finally, MRSA might have been an unrecognized cause of skin infections among inmates; wounds often were attributed to spider bites, and cultures might have been collected infrequently even in cases in which antimicrobial treatment failed. The emergence of MRSA as a cause of inmate skin and soft tissue infections presents a challenge to correctional facilities, health-care providers, and public health agencies. The potential public health impact of MRSA disease transmission in correctional facilities is substantial; during 2002, approximately 2 million prisoners in the United States were incarcerated at any given time, and one in every 142 U.S. residents was in prison or jail (5). Barriers to control of communicable diseases such as viral hepatitis and tuberculosis in correctional facilities are well known (3,6--8). Because of these barriers, prisons and jails can serve as amplifiers of MRSA skin disease. In areas where community-associated MRSA appears to be increasing (e.g., LA County), correctional facilities with shorter durations of incarceration might represent settings in which MRSA is imported from the community and exported back to the community via released inmates. A strategy to improve hygiene and infection-control practices in correctional facilities will likely be the most effective approach for long-term success. Such a strategy should include 1) skin infection screening and monitoring (e.g., maintaining a log of skin infections and visual skin screening on intake), 2) culturing suspect lesions and providing targeted antimicrobial therapy, 3) efforts to improve inmate hygiene (e.g., education about appropriate hand and body hygiene, appropriate laundering techniques, measures to limit use of shared items, and greater availability of soap), and 4) improved access to wound care and trained health-care staff. Adapting traditional hospital-based approaches to preventing MRSA transmission (e.g., placing infected persons in a separate area or eradicating nasal colonization) might not be feasible in most correctional facilities. Some state public health agencies have developed their own approaches for addressing MRSA in correctional settings. In July 2003, the Federal Bureau of Prisons issued guidelines to prevent and control MRSA in correctional facilities (4). Facilities detecting a substantial number of MRSA infections should implement improved hygiene, infection-control, and treatment practices. Correctional facilities experiencing outbreaks of MRSA should seek assistance from their local and state health departments. Preventing MRSA disease in inmates might be an important measure for preventing MRSA in the community outside the correctional facility. Additional information about MRSA is available at http://www.cdc.gov/ncidod/hip/aresist/mrsa.htm References
Figure 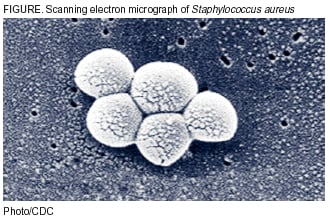 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 10/16/2003 |
|||||||||
This page last reviewed 10/16/2003
|