 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Internet Use and Early Syphilis Infection Among Men Who Have Sex with Men --- San Francisco, California, 1999--2003During the summer of 1999, an outbreak of early syphilis among men who have sex with men (MSM) who met their sex partners on the Internet (1) presaged a rapidly expanding syphilis epidemic in San Francisco. By 2002, San Francisco had the highest rates of primary and secondary syphilis of any metropolitan area in the United States (2). During 1998--2002, the number of early syphilis cases increased, from 41 cases in 1998 to 495 cases in 2002 (3). Concomitant with the increase in early syphilis was an increase in the proportion of cases among MSM, from 22% in 1998 to 88% in 2002 (Figure 1) (3). To assess the association between early syphilis infection and use of the Internet by MSM to meet sex partners, the San Francisco Department of Public Health (SFDPH) analyzed surveillance data and case reports. This report summarizes the results of that analysis, which suggest that public health officials might find the Internet to be an important tool for 1) promoting disease awareness, prevention, and control and 2) accessing sex partners of syphilis patients to conduct appropriate partner notification, evaluation, and management. The findings underscore the need for public health officials to understand the role of the Internet in facilitating the spread of sexually transmitted diseases (STDs), including the human immunodeficiency virus (HIV). With the assistance of community partners, other jurisdictions can examine the online social/sexual networks that are used commonly in their gay and bisexual communities and develop an effective means of communicating prevention and control messages online. In accordance with California law, cases of syphilis are reported to SFDPH by laboratories and public and private health-care providers. A case of early (i.e., <1-year duration) syphilis was defined as a case of primary, secondary, or early latent syphilis diagnosed in a San Francisco resident. Early syphilis cases had darkfield-positive lesions, reactive serologic tests for syphilis and accompanying symptoms, or reactive serologic tests with evidence of syphilis infection occurring during the preceding year. Persons with early syphilis were interviewed by SFDPH staff. Interviewers obtained demographic data (e.g., sex, age, race/ethnicity, address, and sexual orientation) and risk-behavior information (e.g., sexual behavior, condom use, number and sex of partners, venues for meeting partners, alcohol and recreational drug use, and self-reported HIV status) for the period when syphilis might have been acquired or transmitted. This period was determined on the basis of stage of disease at the time of treatment (i.e., 3 months before treatment for primary syphilis, 6 months for secondary syphilis, or 12 months for early latent syphilis). Interviews were accompanied by disease-intervention counseling, which assisted in locating and treating sex partners. Surveillance DataDuring 2002, a total of 434 cases of early syphilis among MSM were reported to SFDPH. The median age of MSM with early syphilis was 38 years (range: 14--66 years). Of these 434 patients, 289 (66.6%) were white, 69 (16.0%) were Hispanic, 34 (7.8%) were Asian/Pacific Islander, 31 (7.1%) were black, and 11 (2.5%) were from other racial/ethnic populations; 293 (67.5%) were HIV seropositive. Information about sexual behavior and sex partners was obtained from 415 MSM. These men reported a total of 6,482 sex partners during the period when syphilis might have been acquired or transmitted (median: six partners; range: zero to 500 partners). The most common venues for meeting sex partners reported by the 415 patients with early syphilis were the Internet (32.6%), bars (20.6%), bathhouses (13.3%), sex clubs (12.6%), and adult bookstores (5.5%). During January 2000--December 2002, the proportion of MSM with early syphilis who reported meeting sex partners on the Internet increased significantly (p<0.0001), from 12.2% during the first half of 2000 to 37.4% during the second half of 2002 (Figure 2). In a review of 151 early syphilis cases among MSM interviewed for partner management during January--April 2003, a total of 67 (44.4%) men reported meeting sex partners over the Internet; 14 (20.9%) provided information about 44 sex partners for whom the only locating information was an Internet e-mail* address. Eleven (25%) of the 44 Internet partners lived outside of the San Francisco Bay Area. SFDPH staff located 15 (34%) of the Internet partners and ensured that they were evaluated and treated appropriately. The following two case reports are illustrative of successful online partner notification, evaluation, and management. Case ReportsCase 1. In February 2003, a Hispanic man aged 36 years had early latent syphilis diagnosed by his private health-care provider. He reported meeting male sex partners through the Internet but not through sex clubs or at bathhouses. In December 2002, he traveled to Los Angeles, California, where he had sex with three different partners. He did not know his total number of partners during the 12-month interview period, but mentioned 16 (i.e., three met in Los Angeles, for whom he had no additional information; five Internet partners; and eight met elsewhere). For the five Internet partners, the patient had only their Internet e-mail addresses, which he provided to SFDPH staff; four lived in San Francisco, and one lived in Minneapolis, Minnesota. All five responded to SFDPH staff e-mail messages and were evaluated and treated preventively for possible incubating syphilis. In addition, the other eight partners were evaluated and treated preventively, including one who lived in Phoenix, Arizona. None of the 13 located partners (Internet and non-Internet) had syphilis at the time of their evaluation. Case 2. In April 2003, a white man aged 43 years had primary syphilis diagnosed at the San Francisco municipal STD clinic. He did not travel outside of the San Francisco Bay Area during the 3-month interview period. He reported meeting male sex partners through the Internet and at bathhouses. Of the 13 partners that the index patient reported during the interview period, he had information about three (i.e., an Internet e-mail address for two partners and a telephone number for one partner). These three partners lived in the San Francisco Bay Area, and two were evaluated and treated appropriately. As a result of being contacted through Internet e-mail, one of the partners (partner A) had early latent syphilis diagnosed in late April 2003. He had traveled to Chicago, Illinois, in December 2002, during the 12-month interview period when he might have been infectious. He reported 50 partners during the interview period and provided only Internet e-mail addresses for four partners and more complete locating information for two other partners. One of these four Internet partners was the index patient. No other Internet partners were located; however, the other two partners were located and evaluated, including one (partner B) who lived in San Jose, California, and had secondary syphilis diagnosed earlier in April 2003. Partner B named the index patient as his only locatable partner; the index patient did not provide any information about partner B. Reported by: CK Kent, MPH, W Wolf, MPA, G Nieri, W Wong, MD, JD Klausner, MD, San Francisco Dept of Public Health, San Francisco, California. TA Peterman, MD, Div of STD Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:This report describes the increasing association between early syphilis infection and use of the Internet as a means for MSM to meet sex partners. Often the only link that these men have to their Internet partners is an e-mail address. This report demonstrates how an Internet e-mail address can be used successfully to notify persons that they have been exposed to syphilis. The findings also suggest that the Internet facilitates MSM meeting sex partners when they travel. Meeting new sex partners while traveling might explain, in part, the rapid dissemination of syphilis among MSM throughout the United States and western Europe (4--7). Health departments should learn how the Internet is used to meet sex partners and how health agencies can use the Internet to contact partners for disease intervention. Concerns about the notification of sex partners through the Internet include protecting confidentiality and ensuring that notification messages are not discarded as junk mail or "spam." To respond to these concerns, SFDPH developed interim practices for performing partner notification online (Box). SFDPH is continuing to refine its online partner management program. The findings in this report are subject to at least three limitations. First, the findings are largely descriptive. Second, not all MSM with early syphilis infection in San Francisco were interviewed; the observations described in this report might not reflect all MSM with early syphilis. Finally, the findings might not be representative of all MSM with early syphilis in the United States. Local health departments in other cities that have had large increases in early syphilis cases among MSM should consider using the Internet for partner notification and management. Internet partner management might serve as a useful new tool in addressing this epidemic, even though it might reach only a small number of partners. In contrast to anonymous partners met in sex clubs, bathhouses, and adult bookstores, effective disease intervention is possible for Internet partners. Online prevention activities can include individual outreach, banner ads with links to sexual health promotion sites, and other social marketing activities (8). CDC is coordinating local and national efforts to engage the gay and bisexual community, Internet service providers, and public health officials in developing effective Internet-based prevention strategies. As has been observed in other cities (4--6), a high proportion of MSM with early syphilis in San Francisco also were co-infected with HIV. Because STDs increase the risk for HIV transmission (9) and MSM are among persons at highest risk for HIV infection (10), controlling syphilis among MSM also might be important for preventing further HIV transmission. The findings in this report underscore the importance of coordinated STD- and HIV-prevention efforts among the gay and bisexual community, public health officials, and health-care providers. Acknowledgments This report is based on contributions by the Syphilis Team; R Kohn, MPH, San Francisco Dept of Public Health, San Francisco, California. Syphilis Rapid Response Team, Div of STD Prevention, National Center for HIV, STD, and TB Prevention, CDC. References
* E-mail service provided by an Internet service provider or an Internet-based e-mail account.
Figure 1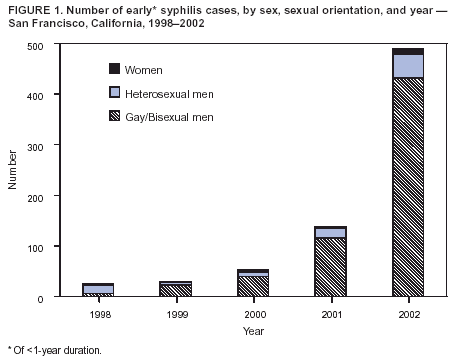 Return to top. Figure 2 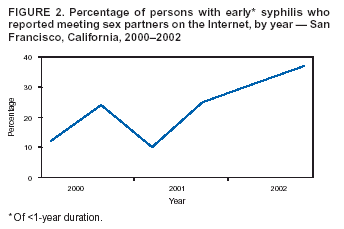 Return to top. Box 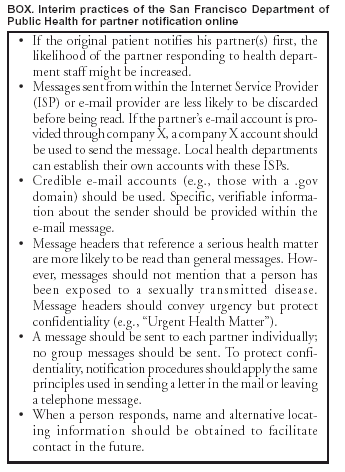 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 12/18/2003 |
|||||||||
This page last reviewed 12/18/2003
|