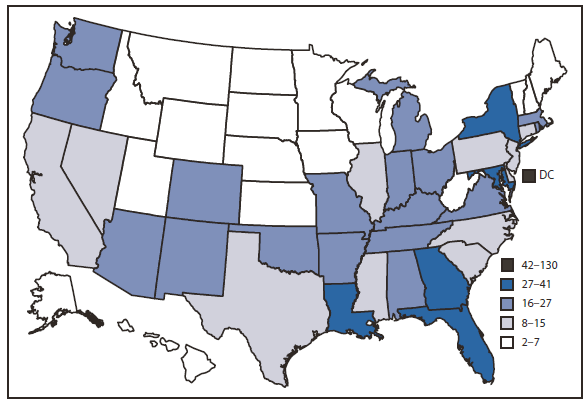
* Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Idaho, Indiana, Iowa, Kansas, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming.
† Alabama, Alaska, Arizona, Arkansas, Colorado, Connecticut, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming.
§ Persons were asked if any of the following statements were true for them, but not which specific statement(s) applied to them. "You have hemophilia and have received clotting factor concentrations. You are a man who has had sex with other men, even just one time. You have taken street drugs by needle, even just one time. You have traded sex for money or drugs, even just one time. You have tested positive for HIV (the virus that causes AIDS). You have had sex (even just one time) with someone who would answer 'yes' to any of these statements."
 ShareCompartir
ShareCompartir