 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. National Plan for Reliable Tuberculosis Laboratory Services Using a Systems ApproachRecommendations from CDC and the Association of Public Health Laboratories Task Force on Tuberculosis Laboratory Services Prepared by The material in this report originated in the National Center for HIV, STD, and TB Prevention, Janet L. Collins, PhD, Acting Director; the Division of Tuberculosis Elimination, Kenneth G. Castro, MD, Director; the Public Health Practice Program Office, Suzanne M. Smith, MD, Acting Director, and the Division of Laboratory Systems, Robert Martin, DrPH, Director. Corresponding preparer: Thomas M. Shinnick, PhD, Chief, Mycobacteriology Laboratory Branch, Division of Tuberculosis Elimination, National Center for HIV, STD, and TB Prevention, CDC, 1600 Clifton Rd., NE, MS G-35, Atlanta, GA 30333; Telephone: 404-639-1474; Fax: 404-639-1287; E-mail: [email protected]. Summary Since the mid-1990s, public health laboratories have improved tuberculosis (TB) test performance, which has contributed to the resumption of the decline in TB incidence in the United States. However, to eliminate TB in the United States, further improvements are needed in laboratory services to support TB treatment, prevention, and control. A critical step is the development of an integrated system that ensures prompt and reliable laboratory testing and flow of information among laboratorians, clinicians, and TB-control officials. Challenges to developing such a system include 1) establishing lines of communication among laboratorians, clinicians, and TB-control officials; 2) expediting reporting of laboratory results, which can avoid delayed or inappropriate treatment and missed opportunities to prevent transmission; 3) developing evidence-based recommendations for use of new laboratory technologies; 4) maintaining staff proficiency in light of declining numbers of specimens to test, workforce shortages, and loss of laboratory expertise; and 5) upgrading laboratory information systems and connecting all partners. The report of the Association of Public Health Laboratories Task Force presents a framework to improve the future of TB laboratory services and describes the role of the laboratory in TB treatment and control, Task Force processes, general principles and benchmarks, and steps for the dissemination of the Task Force recommendations. This MMWR expands on the Task Force report by describing specific actions and performance measures to guide development and implementation of an integrated system for providing TB laboratory services. CDC and the Association of Public Health Laboratories have developed these guidelines so that laboratorians, clinicians, public health officials, administrators, and funding entities can work together to ensure that health-care providers and TB-control officials have the information needed to treat TB patients, prevent TB transmission, and ultimately eliminate TB in the United States. IntroductionApproximately one third of the world's population is infected with Mycobacterium tuberculosis (1), and despite an overall decline in tuberculosis (TB) cases in the United States, TB continues to pose substantial social, public health, and economic costs. In 2003, approximately 15,000 new cases of TB were reported in the United States (2), and an estimated 9--14 million persons have latent TB infection with attendant risk of future disease (3). The laboratory is an essential part of the diagnosis, treatment, prevention, and control of TB (4). Delays in laboratory confirmation of TB and reporting of drug-susceptibility results can lead to delays in initiation of therapy, prolonged infectiousness, inappropriate therapy, and missed opportunities to prevent transmission (5,6). In the early 1990s, such delays contributed to the resurgence of TB and the emergence of multidrug-resistant TB (MDR TB) in the United States (5,6). In response to the threat of MDR TB, CDC increased funding to strengthen public health laboratories and placed emphasis on providing prompt and reliable laboratory results (5,7). Since the early 1990s, public health laboratories have made substantial strides in improving test performance (7--9). These improvements contributed to the resumption of the decline of the incidence of TB in the United States and a decrease in MDR TB cases (10,11) since the mid-1990s. Nevertheless, TB outbreaks still occur and MDR TB continues to spread. For TB to be eliminated in the United States, further improvements in laboratory services are needed, and these advances need to be translated into improvements in the treatment, prevention, and control of TB (11). Prompted by an Institute of Medicine (IOM) report (4) and by the growing need for high-quality, cost-effective TB laboratory services in a time of declining case rates and shifting public health priorities, the Association of Public Health Laboratories (APHL) and CDC commissioned the APHL Task Force on the Future of TB Laboratory Services in 2002. The Task Force includes representatives from APHL, CDC, public health laboratories, clinical laboratories, and the National Tuberculosis Controllers Association (NTCA). The Task Force's primary goal was to develop a framework to improve TB control by promoting optimal use of laboratory services and effective information tracking and reporting. The Task Force defined concerns critical to laboratorians performing TB testing, public health officials, TB-control officials, and health-care providers and created benchmarks and outcome measures to promote delivery of prompt, high-quality, state-of-the-art laboratory services. This report summarizes the recommendations of the Task Force and describes in greater detail specific actions and performance measures to guide development and implementation of an integrated system for providing TB laboratory services. This report also provides information on the scientific basis of the recommendations. BackgroundThe increased incidence in TB cases during the mid-1980s--early 1990s prompted an acceleration of TB-control efforts and focused attention on the role of the mycobacteriology laboratory in supporting patient management and TB-control efforts (4--6). Altogether, TB-related costs approach $1 billion each year in the United States (12). In addition, human immunodeficiency virus (HIV) infection is one of the greatest risk factors for development of TB (13). Prompt and reliable laboratory test results are critical for HIV-infected TB patients because of differences in the clinical analysis and more rapid course of the disease (14). Since 1995, CDC has provided approximately $8 million/year to state and local public health laboratories to improve TB laboratory services (7) and has placed increased emphasis on reliable and prompt results (5,7). The latter included efforts to reduce the delays associated with laboratory testing for M. tuberculosis, to improve communication between laboratorians and health-care providers, and to maintain a trained workforce. Recommendations developed during the mid-1990s for TB laboratory services (9,15,16) remain valid and include
Reports demonstrate that during the 1990s, the emphasis on rapid diagnosis and other improvements in laboratory services contributed substantially to the resumption in the decline of the incidence of TB and the decrease in MDR TB cases nationwide (4,10). TB incidence is limited in certain areas of the United States, but other regions, especially those with substantial immigrant populations, still have high caseloads (4,17). Regardless of caseloads and incidence, effective TB treatment and control require prompt and reliable laboratory services. Laboratory confirmation of a TB case often depends on a network of laboratories providing testing for diagnosis, treatment, and monitoring of therapy outcomes (18--20). However, information is limited regarding the capabilities, capacities, and interactions of the approximately 2,000 TB laboratories at state and local levels and in the private and public sectors. For example, all 50 state public health laboratories perform a level of TB testing and usually serve as the major referral and reference laboratories for culture identification and M. tuberculosis drug-susceptibility testing (7,8); in addition, certain medical centers and commercial laboratories provide advanced TB testing services (21,22). However, the precise contribution of each to TB laboratory services within a jurisdiction is unknown. Approximately 80% of initial TB laboratory testing (e.g., smear and culture inoculation) is performed in the private sector, whereas >50% of species identification and drug-susceptibility testing is conducted in public health laboratories (21). Within a network of laboratories, referring specimens or isolates to other laboratories for testing is common and often involves both the private and public sectors (18--20,22--26). Referral of specimens and cultures can lead to delays in testing, reporting, and treatment initiation for TB patients with smear-positive or smear-negative/culture-positive results (24). Reimbursement models also complicate this process because they might contradict the common practice in which a specimen from a patient with a smear-positive result identified at a local site is referred to a full-service laboratory for culture. The complexities of TB testing and referral underscores the need for an integrated system that emphasizes efficient flow of specimens and information between public health and private-sector laboratorians, clinicians, and TB-control officials. ChallengesImproving TB laboratory services and developing a new, integrated approach is complicated by concerns regarding funding, communication, turnaround times, technology, workforce competence, information management systems, and maintaining proficiency standards. FundingBecause TB laboratory services are provided by both public and private laboratories and supported through a combination of private-sector dollars, Medicare and Medicaid payments, and local, state, and federal funds (4,7,12), the actual cost of providing these services is difficult to estimate. Levels of local, state, and federal funding for TB laboratories have remained constant or have decreased during recent years, and federal funding levels for state public health laboratories to improve TB testing have remained constant at approximately $8 million/year since 1995 (5,7). CommunicationDelays in referring specimens and reporting information can lead to delays in diagnosis, disease treatment and control, and surveillance activities (7,24--26). To optimize TB diagnostic, treatment, and control activities, the flow of specimens and information among laboratorians, clinicians, and TB-control officials should be efficient and well-coordinated. This will require increased communication and coordination among state public health laboratories, clinical laboratories, clinicians, and TB-control programs. Advances in information technology promise to speed the flow of information among key persons, thereby enhancing disease reporting and epidemiologic analysis of disease trends. However, resources to develop and install modern, integrated, compatible, electronic information systems are limited (27). Turnaround TimesRapid detection, species identification, and testing for drug resistance are necessary to control TB among patients and populations. After CDC recommendations were published in 1993 (15), the majority of public and private laboratories began using the recommended rapid methods (7--9,22,23,28). However, approximately one third of laboratories have had difficulty meeting the recommended turnaround times, particularly for drug-susceptibility testing (7,28). A recent California study determined that 1) lengthy specimen transport times and the practice of conducting periodic, as opposed to daily, TB testing were major causes of delay in TB reporting; 2) delays varied by test type and by the type of laboratory performing testing; and 3) laboratory TB-test reporting often failed to conform to national guidelines and California regulations (24). A direct correlation existed between reporting delays and treatment initiation (24). TechnologyCertain technologic advances (e.g., nucleic acid amplification testing [NAAT], fluorescence in situ hybridization, or fluorescence high-performance liquid chromatography [HPLC] of mycolic acids) can contribute substantially to TB treatment and control by providing faster laboratory results (29,30). Such rapid methods will be needed to meet the Healthy People 2010 objective 14-14 of 2 days of average turnaround time for laboratories to confirm and report 75% of culture-confirmed TB cases (31). However, no well-validated testing algorithms are available to guide programs in adopting or using these new technologies in laboratory and program settings with varying TB incidence, although general recommendations exist for use of NAAT to detect M. tuberculosis (32). Workforce CompetenceThe United States is experiencing laboratory workforce shortages ranging from 8% to >20% in different parts of the country, and expertise is being lost as increasing numbers of experienced staff reach retirement age (33). Multiple training programs for clinical laboratory scientists have closed. In the face of worker shortages, vacant positions are sometimes filled by staff who lack training in complex laboratory science. Information Management SystemsOperation of a modern laboratory requires integrating an information management system into the majority of laboratory activities, including inventory management, specimen tracking, test-result reporting, and information sharing with clinicians and public health officials. State-of-the-art laboratory information management systems are available that can improve the quality and organization of laboratory data and speed the flow of information to those who have a need to know. However, the majority of laboratories have either not yet implemented such systems, or they use systems that are not fully compatible with information management programs of TB-control officials or clinicians. Maintaining Proficiency StandardsAs TB incidence declines and as correspondingly fewer cases are detected and fewer specimens tested, maintaining proficiency in TB-control activities will become more difficult (19,20). In addition, TB-control activities will become more expensive because of the loss of economies of scale. Recognizing this, IOM recommended that TB elimination activities be regionalized to provide better access to and more efficient use of clinical, epidemiologic, and other technical services (4). The concept of regionalizing laboratory services was further developed in a consultant's report (7), included as an appendix in the IOM report (4), which recommended that these matters be considered by a special committee of APHL. During initial deliberations, the Task Force made three observations: 1) regionalization was too simplistic as a generic solution to meet the TB-testing needs of diverse populations across the United States; 2) service models emphasizing coordination and collaboration among laboratories within and between jurisdictions were needed; and 3) principles, benchmarks, and outcome measures were required to guide development of TB laboratory systems. ProcessAPHL convened the Task Force in October 2002. Members represented public health programs from states with different population sizes and TB incidence, hospital and commercial laboratories, and CDC. The Task Force crafted a set of principles to guide development of benchmarks, which were specific actions considered essential to improving laboratory TB services and capable of being assessed by outcome measures. An overview of Task Force activities was presented in December 2002 at the National Conference on Laboratory Aspects of Tuberculosis in San Francisco, California. Conference attendees, including laboratory administrators, bench laboratorians, clinicians, and TB-control officials, expressed support for the Task Force and its mission, as evidenced by discussion questions and conference evaluations. In February 2003, a summary of Task Force activities and preliminary benchmarks were presented to the federal Advisory Council for the Elimination of Tuberculosis (ACET). During a subsequent meeting, Task Force members evaluated models of network collaboration to further develop and refine the benchmarks and outcome indicators. Preliminary Task Force recommendations were presented to APHL and NTCA members at their respective annual meetings in June 2003. In February 2004, ACET voted to formally endorse and support the APHL Task Force report, and in May 2004, APHL published the report (34). The recommendations are being presented also to other key stakeholders (e.g., the American Society for Microbiology [ASM] and the American Thoracic Society [ATS]) to garner their input and support. RecommendationsOverall GoalThe Task Force recommendations are intended to improve TB control through the optimal use of laboratory services and effective reporting and tracking of information. Guiding Principles
According to these principles, the laboratory has more active and integral responsibilities in treatment and control efforts through coordinated testing and prompt communication of information to providers and public health agencies to ensure appropriate patient management. Organization of Laboratory ServicesProvision of laboratory services is a jurisdictional concern because of reporting requirements and legal, programmatic, and financial factors, and because the need for laboratory services varies substantially among the diverse state and local treatment and control programs. Within each jurisdiction, laboratorians and TB-control officials should work together to determine how to maximize resources to obtain prompt, reliable test results. Recommended Benchmarks To Improve Laboratory TB Services and TB ControlImplementation of the following actions and base performance measures will require new, more effective partnerships among clinicians, TB-control officials, and public health and clinical laboratorians. Capacity and Capability Assessment Ongoing assessment of available TB laboratory services should be performed to determine the status and capacity of services and to identify unmet needs, obstacles to obtaining laboratory services, and opportunities for improvement. Although data are intended primarily for local use, they might also improve understanding of laboratory capacity and capability for TB testing nationally. A standardized assessment tool should be developed to ensure data are collected consistently. A list of key information to be collected is provided (Box 1). Cost Analysis An assessment of the actual costs of providing TB laboratory services should be performed. Because the cost of identifying individual cases increases as the number of cases declines, the cost of services probably will vary from one jurisdiction to another. A standardized cost-assessment tool should be developed to facilitate comparison of data nationally and across regions. Cost assessment should include expenditures incurred by laboratories, public and private health-care providers, and TB-control programs to 1) provide optimal specimen transport and referral systems; 2) obtain laboratory testing services that meet recommended turnaround times; 3) implement new TB-test technologies in public and private laboratories, as appropriate; 4) provide training for laboratorians and health-care providers; and 5) optimize use of conventional and electronic communication systems, including computers and laboratory information management systems, to facilitate prompt flow of information among laboratorians, clinicians, and TB-control officials. Strategic Planning A strategic plan for implementing and maintaining a systems approach to TB control should be developed. Resources, recommended testing algorithms for different patient populations, and guidelines should be developed to help each jurisdiction select the appropriate level of services for each public health system. The strategic plan should define action steps and assign responsibility for action item completion. The strategic plan should use a systems approach and involve all partners to ensure development, implementation, and ongoing assessment and improvement of a laboratory network that provides critical capabilities (Box 2). Outcome MeasuresThe following outcome measures should be used to assess improvements in laboratory services and in overall TB-control programs. A checklist of key performance indicators is included (Box 3). TB Incidence Improvements in laboratory services should facilitate progress toward elimination of TB and the accomplishment of Healthy People 2010 objective 14-11, which calls for a rate of less than one case per 100,000 persons (31). The laboratory contribution should be evaluated by monitoring 1) the percentage of TB cases for whom microbiology laboratory test results are entered in the Report of a Verified Case of Tuberculosis (RVCT); 2) the percentage of pulmonary or laryngeal TB cases among persons aged >12 years for whom a sputum culture was done and the data entered in the RVCT; and 3) the percentage of culture-positive TB cases with drug-susceptibility results entered in the RVCT. Treatment Initiation All patients with newly diagnosed, highly infectious TB (i.e., patients with positive acid-fast bacilli [AFB] smear test results) should be started on appropriate treatment within 2 days of specimen collection. Progress toward this goal should be evaluated by monitoring 1) the percentage of initial diagnostic specimens for which the date of the report of positive results of AFB-smear microscopy to the health-care provider is within 1 day of the date of specimen collection (35), and 2) the average time to report the results. AFB-Smear, Culture, and Drug-Susceptibility Testing Progress toward the goal of having all laboratories performing and reporting TB testing within the network in accordance with CDC recommendations (15,16) should be evaluated. Evaluation should include, at a minimum, monitoring the percentage of laboratories using recommended methods for their level of service and the percentage of laboratories meeting expedited turnaround times for reporting results and referring specimens or isolates for additional testing. Specimen and Isolate Referral Written procedures for referring specimens and cultures and for reporting results should be available. Performance of the referral system should be monitored for time of specimen transport, tracking of specimens and information, and time of reporting results to submitting laboratories and health-care providers. Incorporation of Rapid-Testing Methods Progress toward accomplishing Healthy People 2010 objective 14-14 (31), which sets a 2-day target for average laboratory turnaround time to confirm and report >75% of culture-confirmed TB cases, should be evaluated by monitoring the percentage of suspected TB patients for whom a rapid test is performed, the average turnaround time for reporting the results of a rapid test, and the percentage of newly diagnosed, culture-positive TB patients for whom the objective is met. Written Procedures for Interaction with TB-Control Partners The laboratory should have a document of understanding that includes written procedures for service provision and communication between the laboratory and TB-control partners, including public health agencies, health-care providers, and state TB-control officials. The document should be monitored for completeness and should include detailed standard operating procedures for
Efficient and Complete Flow of Information To monitor development of an integrated system that ensures prompt, complete, and accurate communication, the following factors should be evaluated:
Isolate Recovery The TB-control program should monitor the percentage of TB patients with culture-positive results for whom the program has obtained and archived an isolate. Measurement of Training Outcomes The program should conduct periodic training needs assessments for laboratorians, clinicians, and TB-control officials, and should develop a plan for providing needed training. Training activities should be evaluated to determine which modifications in operations and performance improvements resulted from training. Models of Network CollaborationBecause the provision of laboratory services is a local concern, laboratorians and TB-control officials should work together to design a system to prioritize testing and maximize resources to obtain prompt, reliable test results. The following are examples of successful models for addressing certain aspects of a successful laboratory network:
California's MGIT By-Mail ModelTo address the need for rapid culture results while maintaining rapid turnaround times for smear microscopy, the California State Public Health Laboratory (CSPHL) implemented a program in which CSPHL provides Bactec MGIT tubes by mail to 10 rural public health laboratories. The laboratories process specimens for mycobacterial smear and culture on-site, decreasing the turnaround time for reporting of smear results. Processed specimens are inoculated onto solid and MGIT culture media. Solid media are incubated and examined locally, but the MGIT tubes are mailed to CSPHL for incubation. For positive MGIT cultures, identification is performed by rapid methods, including DNA probes and HPLC. Drug-susceptibility testing is performed by using the radiometric Bactec method. Advantages of this system include rapid availability of smear results locally, as well as access to state-of-the-art rapid methods for culture identification and drug-susceptibility testing that could not be made available at every local laboratory. Michigan's National Laboratory System ModelThe National Laboratory System (NLS) model (36), originally created for biologic and chemical terrorism preparedness, is based on an integrated public-private laboratory system that uses standard methods and engages in joint planning and training activities. As one of four NLS pilot sites, Michigan applied this model to multiple public health concerns, including TB control. As part of the NLS process, Michigan's state laboratory convened partners (e.g., clinical microbiology laboratory staff, regional public health laboratory directors, county health department surveillance staff, infection-control specialists, physicians, physician assistants, and proficiency-testing providers) in focus groups to identify the steps necessary to build a statewide laboratory system to support response activities for public health emergencies. Two critical concerns were improving specimen transport and improving communications among partners. In response to focus group discussions, the Michigan state laboratory is pilot-testing a statewide courier system for overnight delivery of specimens and AFB-positive broth cultures to the state TB facility for rapid testing. The goals are to provide 1) 24-hour turnaround times for AFB-smear results and rapid culture testing for laboratories that do not perform their own testing and 2) rapid AFB identification and susceptibility testing to laboratories that perform rapid culture but do not perform rapid identification tests. In addition, the state public health laboratory is 1) developing a statewide, Internet-based communication system, the Michigan Disease Surveillance System, to provide epidemiologic and laboratory information to health-care providers engaged in TB-related work; 2) providing training in the standardized epidemiologic and laboratory methods recommended by Healthy People 2010, APHL, CDC, and ACET; and 3) partnering with commercial laboratories and private health-care providers to expedite submission of first isolates from new TB patients for rapid susceptibility testing and molecular typing. New York State Fast Track Referral ModelThe Fast Track model program for TB was initiated by the New York State Department of Health's Wadsworth Laboratory in 1993 to expedite testing for highly infectious TB patients (37). Approximately 165 laboratories within institutions in New York are enrolled in the program. These laboratories process specimens for AFB smear and culture at the local level to provide rapid smear results. Specimens from patients whose smear is AFB-positive, who have a negative smear but radiologic indications and clinical TB symptoms, or who are suspected of having infection with MDR TB are fast-tracked to the state public health laboratory for rapid NAAT, liquid- and solid-media culture, and drug-susceptibility testing. The Fast Track system provides equal access statewide to the latest rapid technology for detection and identification of TB, even for facilities that routinely see no or limited numbers of TB cases. Additionally, this system helps ensure that TB cases are reported rapidly by state laboratorians to health department TB-control programs and that isolates are captured into the public health system for fingerprinting analysis and outbreak investigation. North Dakota Consolidation ModelThe incidence of TB in North Dakota has declined to less than one case per 100,000 state residents per year (2). Since 1993, the number of specimens sent to the state public health laboratory for testing has declined steadily; by 2000, the state laboratory received approximately 29 specimens per week --- a number low enough to generate concerns about staff proficiency (19,20). In 2001, to address these concerns, the state public health laboratory developed a strategic plan for TB laboratory services (38). Elements of the plan included identifying medical centers that were using out-of-state commercial laboratories for TB testing, determining what services the state laboratory needed to provide to compete with private laboratories, and improving relations with private clinical laboratories in the state. Beginning in 2001, state laboratorians implemented amplified direct testing with results available within 24 hours of specimen receipt, modified their processing and testing schedules to improve turnaround time, and met with staff in all North Dakota medical centers to improve communication. By educating partners in the state about the needs of the TB-control program and the services the state laboratory could provide, and by delivering reliable test results with rapid turnaround times, the state laboratory centralized all North Dakota TB testing and increased its specimen volume to >45 specimens/week. Moreover, consolidating testing at the state level made test results readily available to TB program staff. Washington State Core Laboratory ModelThe Washington state core laboratory model, which debuted in 1999, derived from an effort to coordinate delivery of laboratory services within the state in the midst of health-care--system reforms (39). The model ensures that all laboratories have access to state-of-the-art TB testing by consolidating TB diagnostic testing in three specialty laboratories --- the state public health laboratory and two urban hospital laboratories. All three have access to up-to-date technology, and they adhere to recommended safety and reporting requirements. Hospital and clinical laboratories are encouraged to submit clinical TB specimens to one of the two core hospital laboratories. The state public health laboratory examines all clinical specimens submitted by county health departments, serves as the state TB reference laboratory, and maintains capacity to conduct molecular epidemiology studies of TB isolates. It also works with hospital and clinical laboratories that choose to provide limited, on-site TB diagnostic services to ensure that these laboratories meet national TB standards and are integrated into the new delivery system. This model has reduced the clinical workload at the state public health laboratory and simultaneously reduced turnaround times for reporting smear, culture, and drug-susceptibility test results (39). Before initiating this system, state laboratorians evaluated the TB diagnostic capacity and expertise in the state and also examined alternative laboratory delivery systems for providing these services. The state public health laboratory 1) assembled a working group to evaluate possible causes of delays in reporting positive test results, 2) surveyed laboratories that provided TB testing to document the level of service provided and technology being used, 3) conducted on-site reviews of potential core specialty laboratories, and 4) hosted meetings throughout the state to gather input and buy-in from the laboratory community on the new approaches being considered. Wisconsin Mycobacteriology Laboratory Network ModelThe Wisconsin Mycobacteriology Laboratory Network (WMLN) (40), sponsored by the Wisconsin State Laboratory of Hygiene (WSLH) and the state TB-control program, links clinical laboratories with the public health system. WMLN provides data sharing so that all TB-control partners receive regular reports on case counts, outbreaks, and resistance trends. Certain services (i.e., NAAT, HPLC, and TB identification and molecular genotyping) are centralized at WSLH. State laboratorians provide technical training to clinical laboratories, as well as serve as a repository for all TB isolates. The TB network also enhances preparedness for biologic terrorism, because clinical laboratories are prepared to process the TB testing provided by state laboratorians and provide personnel trained in Biosafety Level 3 practices for biologic-specimen processing in the event of a terrorist attack. Development of the network began in 1997 with a survey of laboratorians, clinicians, and public health professionals to evaluate the role of all state laboratories in TB prevention and control. In 1998, a position paper was written by staff from the Wisconsin Tuberculosis Control Program to describe practices and make recommendations to achieve consistent, high-quality testing in all laboratories performing TB testing. The recommendations addressed appropriate use of NAAT, laboratory safety, staff proficiency, problems with cross-contamination, and quality assurance. Beginning in 1999, network members promoted compliance with these recommendations through a series of site visits by WSLH staff and annual meetings with laboratory representatives from across Wisconsin. Dissemination and ImplementationThe recommendations of the APHL Task Force on the Future of TB Laboratory Services have been approved by the APHL Board of Directors and endorsed by ACET. To ensure their widespread dissemination and implementation, key TB-control partners should take the following steps:
--- recommendations for levels of service; Research NeedsContinual improvement in the quality of laboratory services requires investment in and conduct of public health-related research, including 1) operational research to support science- and experience-based recommendations for laboratory services that provide for effective patient management and population-based TB control, 2) cost-benefit analysis for various types of services and technologies, and 3) collaborative technical research to develop and drive the implementation of innovative technologies. ConclusionTo eliminate TB in the United States, clinicians, TB-control officials, and public health officials need access to prompt and reliable TB laboratory services. Delayed laboratory confirmation of TB leads to delays in initiation of therapy, potentially inappropriate therapy, and missed opportunities to prevent transmission. Although provision of laboratory services is a jurisdictional matter and can be organized at the local, state, or regional level, any successful effort to provide prompt, reliable laboratory services should involve assessment and understanding of the structure, performance, and cost of the network of laboratory service providers and users; development of a referral and information network to ensure reliable testing and prompt flow of specimens and information; and use of quality-improvement principles to continually evaluate and improve the performance of the laboratory service network. A systems approach is necessary to optimize laboratory TB testing and information exchange and to ensure that appropriate services are available in every program. Laboratorians, clinicians, public health officials, administrators, and funders should collaborate to ensure that health-care providers and TB-control officials have the information they need to treat TB patients, prevent TB transmission, and ultimately eliminate the disease in the United States. The full report of the APHL Task Force on the Future of TB Laboratory Services (34) provides additional information on the role of the public health laboratory in TB treatment and control, additional background on the Task Force processes, further guidance on developing a system for providing TB laboratory services, and steps for dissemination and implementation of the Task Force recommendations. References
APHL Task Force on the Future of TB Laboratory Services Kathleen G. Beavis, MD, Cook County Hospital, Chicago, Illinois; John Bernardo, MD, Massachusetts Tuberculosis Control Program, Boston, Massachusetts; Eric Blank, DrPH, Missouri State Public Health Laboratory, Jefferson City, Missouri; Ed Desmond, PhD, California State Public Health Laboratory, Richmond, California; Richard Harris, PhD, Wyoming State Public Health Laboratory, Cheyenne, Wyoming; Rosemary Humes, MS, Association of Public Health Laboratories, Washington, D.C.; Michael F. Iademarco, MD, Division of TB Elimination, National Center for HIV, STD, and TB Prevention, CDC; John Ridderhof, DrPH, Division of Laboratory Systems, Public Health Program Practice Office, CDC; Thomas M. Shinnick, PhD, Division of TB Elimination, National Center for HIV, STD, and TB Prevention, CDC; Nancy Warren, PhD, Laboratory Corporation of America, Burlington, North Carolina. Box 1 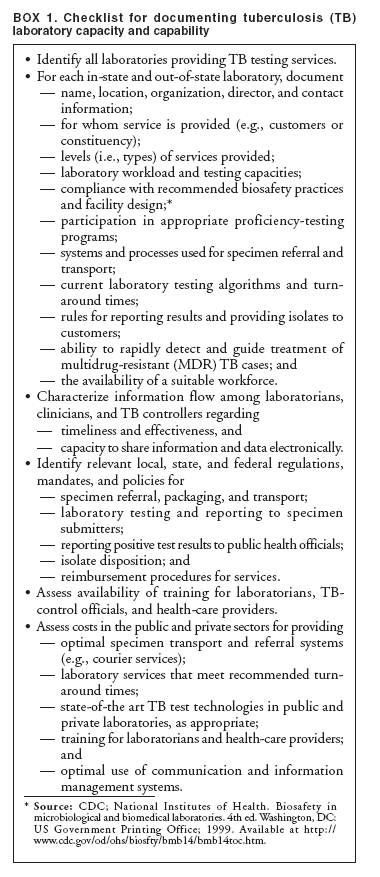 Return to top. Box 2 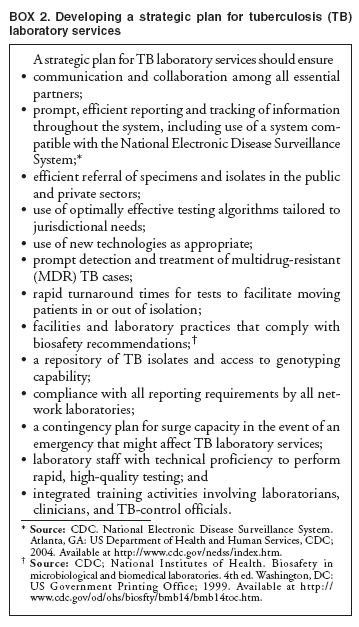 Return to top. Box 3 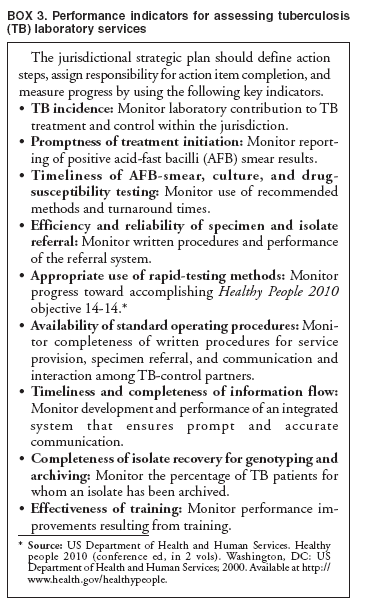 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Page converted: 3/28/2005 |
|||||||||
This page last reviewed 3/28/2005
|