 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. Surveillance for Acute Viral Hepatitis --- United States, 2006Annemarie Wasley, ScD
Corresponding author: Annemarie Wasley, ScD, Division of Viral Hepatitis, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, 1600 Clifton Rd., N.E., MS G-37, Atlanta, GA 30333. Telephone: 404-718-8500; Fax: 404-718-8585; E-mail: [email protected]. AbstractProblem/Condition: In the United States, acute viral hepatitis most frequently is caused by infection with three viruses: hepatitis A virus (HAV), hepatitis B virus (HBV), and hepatitis C virus (HCV). These unrelated viruses are transmitted through different routes and have different epidemiologic profiles. Safe and effective vaccines have been available for hepatitis B since 1981 and for hepatitis A since 1995. No vaccine exists against hepatitis C. Reporting Period Covered: Cases in 2006, the most recent year for which data are available, are compared with those from previous years. Description of System: Cases of acute viral hepatitis are reported voluntarily to CDC by state and territorial epidemiologists via CDC's National Notifiable Disease Surveillance System (NNDSS). Reports are received electronically via CDC's National Electronic Telecommunications System for Surveillance (NETSS). Results: During 1995--2006, hepatitis A incidence declined 90% to the lowest rate ever recorded (1.2 cases per 100,000 population). Declines were greatest among children and in those states where routine vaccination of children was recommended beginning in 1999. An increasing proportion of cases occurred in adults. During 1990--2006, acute hepatitis B incidence declined 81% to the lowest rate ever recorded (1.6 cases per 100,000 population). Declines occurred among all age groups but were greatest among children aged <15 years. Following a peak in the late 1980s, incidence of acute hepatitis C declined through the 1990s; however, since 2003, rates have plateaued, with a slight increas in reported cases in 2006. In 2006, as in previous years, the majority of these cases occurred among adults, and injection-drug use was the most common risk factor. Interpretation: The results documented in this report suggest that implementation of the 1999 recommendations for routine childhood hepatitis A vaccination in the United States has reduced rates of infection and that universal vaccination of children against hepatitis B has reduced disease incidence substantially among younger age groups. Higher rates of hepatitis B continue among adults, particularly males aged 25--44 years, reflecting the need to vaccinate adults at risk for HBV infection. The decline in hepatitis C incidence that occurred in the 1990s was attributable primarily to a decrease in incidence among injection-drug users. The reasons for this decrease were unknown but likely reflected changes in behavior and practices among injection-drug users. Public Health Actions: The expansion in 2006 of recommendations for routine hepatitis A vaccination to include all children in the United States aged 12--23 months is expected to reduce hepatitis A rates further. Ongoing hepatitis B vaccination programs ultimately will eliminate domestic HBV transmission, and increased vaccination of adults with risk factors will accelerate progress toward elimination. Prevention of hepatitis C relies on identifying and counseling uninfected persons at risk for hepatitis C (e.g., injection-drug users) regarding ways to protect themselves from infection and on identifying and preventing transmission of HCV in health-care settings. IntroductionViral hepatitis is caused by infection with any of at least five distinct viruses, of which the three most commonly identified in the United States are hepatitis A virus (HAV), hepatitis B virus (HBV), and hepatitis C virus (HCV). All three of these unrelated viruses can produce an acute illness characterized by nausea, malaise, abdominal pain, and jaundice. HBV and HCV also can produce a chronic infection that is associated with an increased risk for chronic liver disease and hepatocellular carcinoma. This report describes the burden of acute disease attributed to infection with HAV, HBV, and HCV and describes acute disease trends in recent years. These data can be used to develop and evaluate prevention strategies and identifies persons in need of postexposure prophylaxis. The data on acute illness presented in this report do not include the burden of disease caused by chronic infection with HBV or HCV, both of which remain a substantial public health problem. Hepatitis A VirusHAV is transmitted through the fecal-oral route, spreading primarily through close personal contact. During 1987--1997, an average of 28,000 cases of hepatitis A occurred per year in the United States (range: 23,112--35,821), making hepatitis A one of the country's most frequently reported notifiable diseases. However, effective vaccines to prevent HAV infection have been available in the United States since 1995. These vaccines have provided public health authorities with the opportunity to reduce disease incidence in the United States substantially and potentially to eliminate indigenous transmission. In 1996, CDC's Advisory Committee on Immunization Practices (ACIP) recommended administration of hepatitis A vaccine for persons at increased risk, including international travelers, men who have sex with men (MSM), injection- and noninjection-drug users, and children living in communities with high rates of disease (1). In 1999, ACIP also recommended that routine vaccination be implemented for children living in 11 states with average hepatitis A rates during 1987--1997 of >20 cases per 100,000 population and also be considered for children in six states with rates of 10--20 cases per 100,000 population (2). In 2005, ACIP expanded these recommendations to include routine vaccination of children in all 50 states (3). Hepatitis B VirusHBV is transmitted by percutaneous or mucosal exposure to the blood or body fluids of an infected person, most often through injection-drug use [IDU], sexual contact with an infected person, or contact from an infected mother to her infant during delivery. Transmission of HBV also can occur in settings involving nonsexual interpersonal contact for an extended period (e.g., among household contacts of a person with chronic HBV infection). In 1991, a comprehensive strategy was recommended for the elimination of HBV transmission in the United States (4,5). The four elements of this strategy are 1) universal vaccination of infants beginning at birth, 2) prevention of perinatal HBV infection through routine screening of all pregnant women for HBV infection and the provision of immunoprophylaxis to infants born to infected women or to women of unknown infection status, 3) routine vaccination of previously unvaccinated children and adolescents, and 4) vaccination of adults at increased risk for infection (including health care workers, dialysis patients, household contacts and sex partners of persons with chronic HBV infection, recipients of certain blood products, persons with a recent history of multiple sex partners or an STD, MSM, and injection-drug users). Hepatitis C VirusHCV also is transmitted percutaneously. With an estimated 3.2 million chronically infected persons nationwide, HCV infection is the most common bloodborne infection in the United States (6). No vaccine against HCV infection exists. National recommendations for prevention and control of HCV infection (7), issued in 1998, emphasize primary prevention activities to reduce the risk for HCV transmission. These activities include screening and testing of blood donors, viral inactivation of plasma-derived products, risk-reduction counseling and screening of persons at risk for HCV infection, and routine practice of infection control in health-care settings. MethodsConditions for Which Surveillance is ConductedNational surveillance is conducted for acute hepatitis A, B, and C. The case definitions for these conditions are approved by the Council of State and Territorial Epidemiologists (CSTE) and are provided in this report. Data SourcesCases of acute viral hepatitis are reported to CDC weekly by state and territorial health departments to CDC's National Notifiable Diseases Surveillance System (NNDSS). Since January 1, 2002, all reports have been submitted electronically to CDC via the National Electronic Telecommunications System for Surveillance (NETSS). States' participation in reporting nationally notifiable diseases, including acute viral hepatitis, to CDC is voluntary. All states collect and report basic information (e.g., event date, source of report, and demographic characteristics) regarding cases of acute viral hepatitis that are identified in their states. States also are asked to report additional information (e.g., laboratory test results, clinical information, and exposure history) regarding investigated cases, but completeness of reporting of these additional data varies. As in previous years, approximately 40% of case reports received by CDC include any of these additional data. Information regarding state-specific reporting profiles is provided in this report (Table 1). Case Definitions for Acute Viral HepatitisIn 2006, cases were required to meet the clinical definition for acute hepatitis and virus-specific laboratory criteria for diagnosis specified in the following CSTE-approved case definitions. Clinical Case Definition Acute hepatitis was defined as acute illness with 1) discrete onset of symptoms (e.g., nausea, anorexia, fever, malaise, or abdominal pain) and 2) jaundice or elevated serum aminotransferase levels. Laboratory Criteria for Diagnosis of Hepatitis Because the clinical characteristics are the same for all types of acute viral hepatitis, laboratory testing is needed to identify the specific viral cause of illness. The laboratory criteria for confirming each type of acute viral hepatitis are as follows:
Case Classification For this analysis, a confirmed case was one that met the clinical case definition and was laboratory-confirmed. For hepatitis A, a case also was considered confirmed that met the clinical case definition and was diagnosed in a person who had an epidemiologic link to a person who had laboratory-confirmed hepatitis A (i.e., household or sexual contact with an infected person during the 15--50 days before the onset of symptoms). AnalysesIncidence Calculations For this analysis, crude rates per 100,000 population were calculated using Bureau of the Census estimates of the U.S. resident population in 2006. The following U.S. geographic regions were used: Midwest, Northeast, South, and West.* Frequency Analysis For this analysis, the percentage of persons who reported a specific risk factor was determined by using the number of persons who reported any information, positive or negative, regarding that exposure as the denominator. Depending on the type of hepatitis, the percentage of case reports that included any risk factor information ranged from 30%--40%. Multiple risk factors may be reported for a single person. Consequently, the percentages of persons with specific risk factors might total >100%. ResultsAcute Viral Hepatitis AOverall Incidence Historically, acute hepatitis A rates have varied cyclically, with nationwide increases every 10--15 years. The national rate of hepatitis A has declined steadily since the last peak in 1995. In 2006, a total of 3,579 acute symptomatic cases of hepatitis A were reported, the national incidence (1.2 per 100,000 population) was the lowest ever recorded (Figure 1; Tables 2 and 3). After asymptomatic infection and underreporting were taken into account, an estimated 32,000 new infections occurred in 2006 (8). Rates by Region In addition to temporal variation, historically, hepatitis A rates have varied geographically, with higher rates reported in the western region of the United States. However, incidence in the West has declined substantially, most notably after issuance in 1999 of recommendations for routine childhood vaccination in states with consistently elevated rates of hepatitis A (2). In 2006, rates in the West were approximately equal to those in other regions of the United States (Figures 2 and 3). Rates by Age Incidence of hepatitis A varies by age. Since the last nationwide increase in 1995, rates have declined among all age groups, but the greatest decreases have occurred among children. Historically, the highest rates were observed among children and young adults; the lowest rates were among persons aged >40 years. However, since 1997, rates among children have declined more rapidly than rates among adults, and, in 2006, rates were similar across all age groups, ranging from 0.7 cases per 100,000 population among children aged <5 years to 1.4 cases per 100,000 population among persons aged 5--14 years (Figure 4). Since 2000, the lowest rates have occurred among children aged <5 years. However, asymptomatic infection is common among young children, and symptomatic cases in children aged <5 years represent only a limited proportion of infections that occur in this age group. Rates by Sex Rates of hepatitis A consistently have been higher among males than among females, and, during the late 1990s through 2001, the difference in the sex-specific rates increased until nearly two male cases were observed for every female case. However, beginning in 2001, rates declined more among males than among females, and, since 2003, the ratio of the number of male cases to female cases has ranged from 1.2 to 1.3. In 2006, overall incidence among males was 1.3 cases per 100,000 population compared with 1.1 cases per 100,000 population among females. The difference in hepatitis A rates by sex was highest among persons aged 30--49 years (Figures 5 and 6). Rates by Race and Ethnicity Hepatitis A rates have differed historically by race; the highest rates occurred among American Indian/Alaska Natives (AI/ANs), and the lowest rates have occurred among Asians/Pacific Islanders (APIs). However, rates among AI/ANs, which were >60 cases per 100,000 population before 1995, have decreased dramatically, and, since 2003, have been lower than those for other races. In 2006, the rate for AI/ANs was 0.5 cases per 100,000 population. Hepatitis A rates also have differed by ethnicity; rates among Hispanics have consistently been higher compared with non-Hispanics. Rates among Hispanics have decreased since 1997 but remain higher than those for non-Hispanics (Figure 7). Reported Risk Factors In 2006, among cases for which information regarding exposures during the incubation period was collected, the most frequently identified risk factor for hepatitis A was international travel (reported by 15% of case patients overall). As in previous years, the majority of travel-related cases were associated with travel to Mexico and Central/South America (72%). As HAV transmission in the United States has decreased, cases among travelers to countries in which hepatitis is endemic have accounted for an increased proportion of all cases. Sexual and household contact with another person with hepatitis A has been among the most frequently identified risks; in 2006, such contact was reported for 10% of cases. During 2004--2006, the proportion of cases reported among MSM increased from 3% to 9%, and the proportion of cases in persons reporting IDU declined from 13% to 2% (Table 4; Figure 8). Clinical Characteristics In 2006, the clinical characteristics of reported hepatitis A cases were similar to previous years; 73% of infected persons had jaundice, 33% were hospitalized for hepatitis A, and 0.3% died from hepatitis A. The proportion of persons hospitalized increased with age, from 22% among children aged <5 years to 52% among persons aged >60 years (Table 5). Acute Hepatitis BOverall Incidence In 2006, a total of 4,713 acute, symptomatic cases of hepatitis B were reported nationwide. The overall incidence (1.6 cases per 100,000 population) was the lowest ever recorded and represents a decline of 81% since 1990 (Tables 2 and 6; Figure 9). After asymptomatic infection and underreporting were taken into account, an estimated 46,000 new infections occurred in 2006 (8). Rates by Region Hepatitis B rates continued to decline in all U.S. regions (Figures 10 and 11). Since 2001, the highest rates have occurred in the South. Rates by Age Hepatitis B rates varied by age, with the highest rate in 2006 (3.1 cases per 100,000 population) reported among persons aged 25--44 years and the lowest (0.02 cases per 100,000 population) reported among persons aged <15 years. Rates declined in all age groups. Since 1990, the greatest percentage declines have occurred among persons aged <15 years (98%) and those aged 15--24 years (93%). Although not as large as the declines in the younger age groups, substantial decreases also have occurred among older persons; the rates observed for persons aged 25--44 years and >45 years have decreased 78% and 61%, respectively (Figure 12). Rates by Sex As in previous years, in 2006, the rate of acute hepatitis B for males (2.0 cases per 100,000 population) was higher than that for females (1.1 case per 100,000 population). Since 1990, male-to-female ratio of cases has increased gradually. In 2006, the rate for males was approximately 1.8 times higher than that for females (Figure 13). This difference in hepatitis B rates by sex occurred primarily among persons aged >19 years and increased with age (Figure 14). Rates by Race and Ethnicity In 2006, rates of hepatitis B continued to decline among all racial/ethnic populations; however, recent declines have been less than earlier in the decade (Figure 15). Rates of hepatitis B are similar across racial/ethnic populations, except for non-Hispanic blacks; the rate for this population (2.3 cases per 100,000 population) was higher than for other populations. The downward trend in the rate among APIs continues, and, in 2006, the rate for this population (1.2 cases per 100,000 population) was similar to Hispanics and to non-Hispanic whites (1.1 case per 100,000 population, for both populations). Reported Risk Factors for Infection Of persons for whom information regarding exposures during the incubation period was available, approximately one third reported at least one sexual risk factor (i.e., 8%, sexual contact with a person known to have hepatitis B; 34%, multiple sexual partners; and 15%, MSM). IDU was reported for 16% of persons. Since 2001, the proportion of persons who reported either a sexual risk or IDU has increased gradually as the number of cases attributable to other sources of transmission (e.g., blood transfusions and dialysis) has declined. The proportion of persons who reported receiving hemodialysis or a blood transfusion (both of which historically were major sources of infection) or having had occupational exposure to blood was low (0.2%, 0.6%, and 0.5%, respectively) (Table 7; Figure 16). Clinical Characteristics In 2006, of persons reported with hepatitis B, 77% had jaundice, 40% were hospitalized, and 0.8% died. The proportion of persons hospitalized for hepatitis B increased with age, from 12% among children aged <15 years to 51% among persons aged >60 years (Table 8). Acute Hepatitis COverall Incidence During 2005--2006, the number of confirmed cases of acute hepatitis C reported increased 19%, from 671 to 802. The overall national rate for 2006 was 0.3 cases per 100,000 population. After asymptomatic infection and underreporting were taken into account, approximately 19,000 new HCV infections occurred in 2006 (8) (Tables 2 and 9; Figure 17). Rates by Age Since the mid-1990s, hepatitis C rates have declined in all age groups. However, rates appear to have reached a plateau since 2003. The greatest decline has occurred among persons aged 25--39 years, the age group that historically has had the highest rates of disease. Among this age group, incidence has declined 58% since 2000. In 2006, rates increased slightly among persons aged 25--39 years (0.47 per 100,000 population) and those aged 15--24 years (0.37 per 100,000 population). Few cases are reported among persons aged <15 years (Figure 18). Rates by Sex In 2006, as in previous years, the rate of hepatitis C was higher for males (0.29 cases per 100,000 population) than for females (0.25 cases per 100,000 population). However, this differential in rates has declined over the decade. In 2006, the male-to-female ratio was the smallest since reporting began (Figures 19 and 20). Rates by Race and Ethnicity Since 1995, the incidence of hepatitis C has declined in all racial populations. In 2006, rates were similar across racial/ethnic populations and ranged from 0.62 cases per 100,000 population among AI/ANs to 0.07 cases per 100,000 population among APIs (Figure 21). Reported Risk Factors for Infection Of the cases reported in 2006 for which information concerning exposures during the incubation period was available, the most common risk factor identified was IDU (54%). During the previous decade, IDU was reported for an average of 42% of persons (range: 31%--54%). In 2006, 36% reported having had multiple sexual partners during the incubation period, and 10% reported sexual contact with another known HCV-infected person. Having had surgery was reported for 16% of persons with hepatitis C. A total of 1.5% reported occupational exposure to blood (Table 10; Figure 22). Clinical Characteristics In 2006, of persons reported with hepatitis C, 66% had jaundice, 41% were hospitalized, and 0.2% died (Table 11). DiscussionNational surveillance data for acute viral hepatitis provides the information needed for developing prevention strategies and monitoring their effectiveness. Since national surveillance for acute viral hepatitis in the United States began in 1966, major changes in the epidemiology of these diseases have occurred. During 1995--2006, rates for all three types of acute viral hepatitis declined dramatically. These declines partially resulted from implementation of comprehensive prevention strategies for each disease, including the introduction of effective vaccines against hepatitis A and hepatitis B. Hepatitis AHepatitis A rates have varied cyclically, with peaks occurring approximately every 10--15 years; the last peak in morbidity occurred in 1995. The incidence of hepatitis A began to decline after the introduction of licensed hepatitis A vaccines in the United States in 1995 and the issuance in 1996 of the first public health recommendations for the use of vaccine to prevent transmission of HAV (1). The greatest declines have occurred since 1999, when recommendations were made for routine vaccination of children living in states with consistently elevated rates of hepatitis A. These recommendations called for 1) routine vaccination of children living in states and communities where the average hepatitis A rate during the baseline period (1987--1997) was >20 cases per 100,000 population (twice the national average) and for 2) consideration of vaccination of children in those states and communities where the average rate during the baseline period was at least 10 cases per 100,000 but not as high as 20 cases per 100,000 population (2). After implementation of the recommended vaccination strategy, major changes occurred in the geographic distribution of hepatitis A. Relative to their prevaccine-era rates, a substantially greater decline occurred for the 17 western and midwestern states that were included in the 1999 recommendation than for the remainder of the country (9). As a result of this decline, hepatitis A rates now are similar across all regions. After the implementation of routine childhood vaccination, changes in the age distribution also occurred. During the prevaccine era, the reported incidence of hepatitis A was highest among children aged 5--14 years; approximately one third of reported cases occurred among children aged <15 years. Since implementation of routine childhood vaccination, incidence has declined more sharply among the age groups (i.e., 2--18 years) covered by the recommendations than among older age groups. As a result, rates now are similar among all age groups (9). In 2006, the highest rates of disease occurred among adults, particularly among males aged 20--44 years. The low and relatively stable rates among persons aged >40 years reflect the higher proportion of persons in this age group who had immunity as a result of previous infection. Data from the Third National Health and Nutrition Examination Survey (NHANES III) conducted during 1988--1994 indicated that approximately 30% of the U.S. population had serologic evidence of immunity to HAV, reaching a high of 75% among persons aged >70 years (10). Disparities in rates among racial/ethnic populations also decreased after the introduction of hepatitis A vaccine. In particular, rates among AI/ANs were five times those of other racial/ethnic population during the prevaccine era. Widespread use of hepatitis A vaccine in Native American communities began in 1996 (11), and rates in this population now are lower than those of other racial/ethnic populations. Hispanics also historically have had elevated hepatitis A rates, and although incidence among Hispanics declined >85% during 1996--2006, the 2006 rate for Hispanics (2.3 cases per 100,000 population) is two to four times higher than the rate for non-Hispanics. The observed declines in the incidence of hepatitis A were accompanied by shifts in epidemiologic profile of this disease. The substantial communitywide outbreaks that occurred as a result of person-to-person contact in households and extended family settings have become increasingly rare. The disappearance of these outbreaks can be attributed to declining rates of infection among children who, because they frequently have asymptomatic infection, have often played a key role is sustaining HAV transmission. As this type of transmission has decreased, the proportion of cases among persons in high-risk populations (particularly international travelers, injection-drug users, and MSM) has increased. Although the absolute number of cases associated with international travel has remained nearly unchanged, the proportion of cases attributable to this exposure has increased, accounting for 15% of all cases in 2006. Approximately 70% of all travel-related cases were associated with travel to Mexico and to Central or South America. Outbreaks of hepatitis A among injection-drug users and MSM also have continued to occur although hepatitis A vaccine has been recommended for these populations since 1996. In 2005, the licensing of hepatitis A vaccines was revised to allow vaccination of children aged 12--23 months, which has made feasible the incorporation of hepatitis A vaccine into the schedule of other routinely recommended childhood vaccines. In 2006, ACIP recommended that all children in the United States aged 12--23 months receive hepatitis A vaccine (3). Nationwide hepatitis A vaccination of children is likely to result in further narrowing of current demographic disparities and in lower overall rates of infection. The 2006 recommendations provide the foundation for eventual consideration of elimination of indigenous HAV transmission in the United States. Ongoing surveillance for acute hepatitis A provides the data needed to measure the progress toward that goal. Hepatitis BThe decline in hepatitis B incidence began in the mid-1980s and has coincided with the stepwise implementation of the national vaccination strategy to eliminate HBV transmission. The 2006 rate of 1.6 cases per 100,000 population was the lowest recorded since surveillance began in 1966 and represents an estimated decline of >80% since the national strategy was implemented in 1991. The greatest declines have occurred among the cohort of children to whom the recommendations for routine infant and adolescent vaccination have applied. During 1990--2006, incidence among children aged <15 years declined 98%, from 1.2 cases per 100,000 population to 0.02 cases per 100,000 population. This decline correlates with high vaccine coverage rates among young children, with the most recent data indicating that coverage among children aged 19--35 months is >93% (12). Although incidence also has declined among persons aged 25--44 years, rates in this age group, particularly among males, still remained substantially higher than in any other age group. A high proportion of these cases occurred among persons with risk factors for HBV infection (e.g., injection-drug users, MSM, and persons with multiple sex partners). The male-to-female ratio has increased gradually; in 2006, approximately 1.8 male cases were reported for every female case. Few cases now occur in certain populations that previously were considered to be at high risk (e.g., dialysis patients and health-care workers) as a result of continued improvements in infection control and ongoing hepatitis B vaccination in these groups. A 2003 survey indicated that approximately 75% of health-care workers have been vaccinated against hepatitis B (13). In 2002, coverage among dialysis patients was 56% (14). Transmission associated with transfusions is rare as a result of required screening of blood products. In contrast, the continued occurrence of cases among injection-drug users and persons with sexual risk factors indicates a need to strengthen efforts to reach these populations with vaccine. In 2007, in collaboration with state and local health agencies, CDC launched the Adult Hepatitis B Vaccination Initiative to provide approximately $20 million of funding for grantees to purchase hepatitis B vaccine and begin or expand delivery of viral hepatitis prevention services in public health settings serving adults at risk for viral hepatitis. Since 1990, progress has been made in reducing racial/ethnic disparities in hepatitis B rates. Before 1990, APIs had disproportionately higher rates of hepatitis B. The decrease in disparity between APIs and other racial/ethnic populations was consistent with observed declines in the seroprevalence of HBV infection among high-risk Asian children after the successful implementation of routine hepatitis B vaccination (15,16). Although rates among non-Hispanic blacks have declined, they remain more than twofold higher than those among other racial/ethnic populations. Although progress has been made in reducing disparities in incidence of new infection, the impact of these disparities in the past are reflected in current prevalence patterns, with higher prevalences of chronic HBV infection among APIs and non-Hispanic blacks than among other populations. Health-care--related transmission of hepatitis B is documented infrequently in the United States but should be considered when cases of acute viral hepatitis are identified in persons without traditional risk factors. The declining incidence of hepatitis B has been associated with increasing recognition of sporadic cases associated with medical care (17,18). State and local health authorities should consider strategies to improve detection of health-care--associated cases, such as targeting intensive follow-up for persons who typically are at low risk for infection (e.g., persons aged >60 years). Surveillance data for acute hepatitis B are needed for measuring the effectiveness of the HBV-elimination strategy. However, to describe completely the burden of HBV infection in the United States and to better assess the effectiveness of certain components of the prevention strategy, other types of surveillance data also are needed. Data from a national seroprevalence survey indicate that approximately 1.3 million persons in the United States are living with chronic HBV infection (19). As incidence of acute hepatitis B continues to decline, seroprevalence surveys are needed to validate incidence data and describe the burden of chronic HBV infection. Hepatitis CAfter peaking in the late 1980s, the incidence of hepatitis C declined steadily through the 1990s. However, since 2003, hepatitis C rates have plateaued, with IDU remaining the most commonly identified risk factor for infection. Transmission of HCV associated with transfusion, an important risk for infection in previous years, was rare as a result of required blood screening. The investigation of persons without typical risk factors will help to ensure the detection of transmission associated with medical care and other uncommon sources of infection. Since 1992, the greatest declines in incidence of acute hepatitis C have occurred among persons aged 25--39 years, the age group that historically had the highest rates of infection. In 2006, cases among children continued to be rare. Progress has been made in reducing disparities in racial/ethnic-specific rates; in 2006, the incidence of acute hepatitis C was similar across all racial/ethnic populations. However, previous racial/ethnic disparities in incidence were demonstrated by disparities in prevalence, with a higher prevalence of chronic infection among non-Hispanic blacks than among other racial/ethnic populations. Although the number of new cases of acute hepatitis C has declined, a substantial burden of disease as a result of chronic infection still persisted in 2006. Approximately 3.2 million persons in the United States were chronically infected with HCV; the peak prevalence occurred among persons aged 40--49 years, the majority of whom likely became infected in the 1970s and 1980s, when incidence was highest (4). Data on both the incidence of acute disease and the prevalence of chronic infection are needed to assess the burden of disease attributable to HCV infection in the United States comprehensively. However, surveillance for acute hepatitis C remains critical as the best means to assess the impact of primary prevention strategies, determine where transmission continues to occur, and identify and control outbreaks. LimitationsThe analyses summarized in this report were performed on the basis of cases of symptomatic, serologically confirmed, acute viral hepatitis reported to NNDSS. NNDSS is a passive surveillance system and subject to at least two limitations. First, the cases reported represent only a portion of all infections. Surveillance for acute disease is not intended to identify asymptomatic infections, and certain persons with symptomatic illness also are not identified and reported. Studies have estimated that for each hepatitis case reported to NNDSS, two to five cases that would meet the case definition are not reported (20,21). Second, completeness of case reports also can vary. However, available evidence suggests that no systematic changes have occurred in reporting patterns since 1990 (CDC, unpublished data, 2007). The national trends in this report also are reflected in CDC's Sentinel Counties Study of Acute Viral Hepatitis, in which the accuracy and completeness of reporting were assessed and known to be high (22). Rates based on NNDSS data represent a lower estimate of the incidence of acute viral hepatitis in the United States because not all cases of acute hepatitis are reported. However, because the proportion of cases not reported has not changed systematically over time, these estimates accurately reflect changing trends in these diseases in the United States. ConclusionSurveillance for acute viral hepatitis accomplishes multiple key public health objectives. Surveillance detects outbreaks, identifies persons in need of postexposure prophylaxis, and provides information on trends in the incidence and risks for recent infection that is needed to develop and evaluate prevention strategies. The minimum data required to conduct surveillance for acute viral hepatitis are laboratory confirmation of cases to distinguish the types of acute hepatitis and clinical information to verify the case definition. The collection of risk data provides valuable information for identifying modes of hepatitis transmission and for implementing and evaluating prevention strategies. With continuing declines in the incidence of all types of acute viral hepatitis, surveillance efforts should be enhanced to ensure complete and accurate reporting of all cases so that the impact of strategies for preventing or eliminating transmission of these diseases can be monitored and evaluated. In addition, effective and feasible systems for conducting surveillance for chronic hepatitis virus infections are needed to characterize the burden of chronic disease that remains in the United States as a result of these infections. AcknowledgmentData for this report were provided by State and Territorial Health Departments. References
* Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont; South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; and West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming. Table 1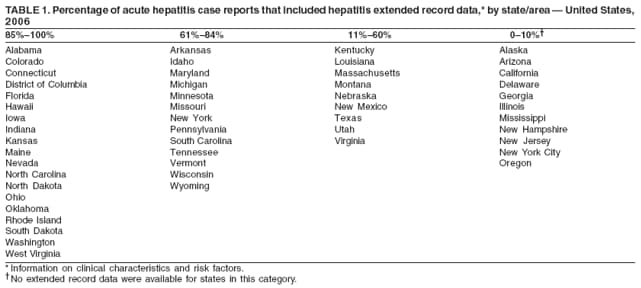 Return to top. Figure 1 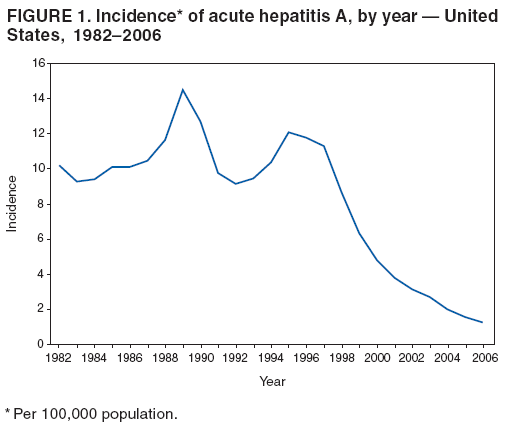 Return to top. Table 2 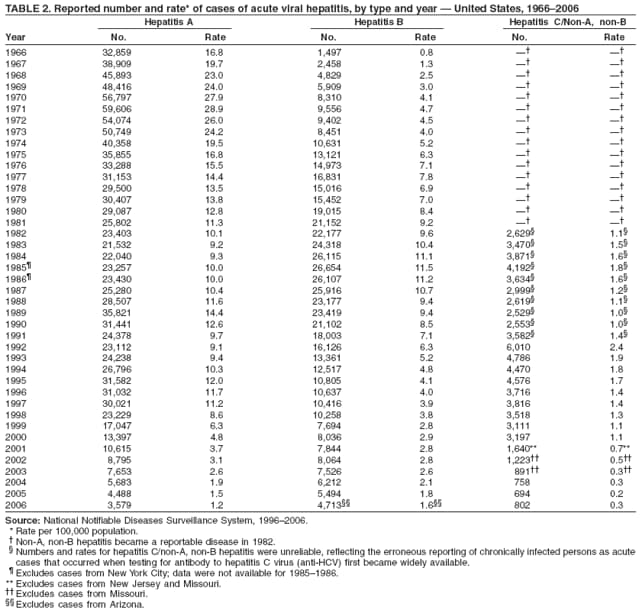 Return to top. Figure 2 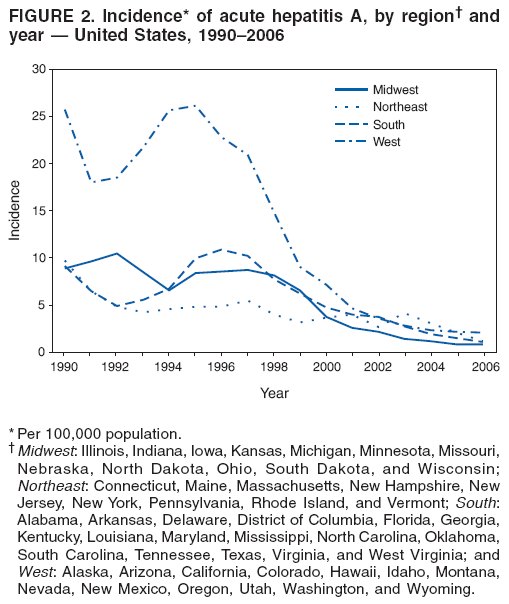 Return to top. Table 3 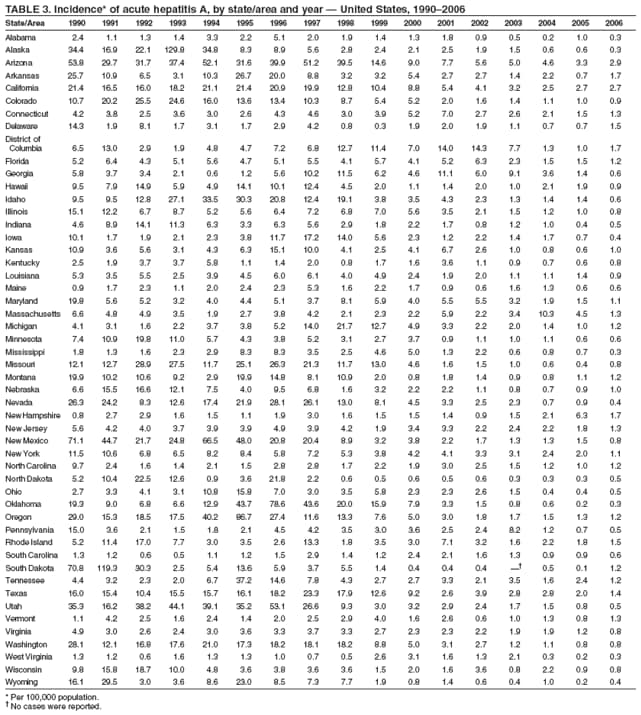 Return to top. Figure 3 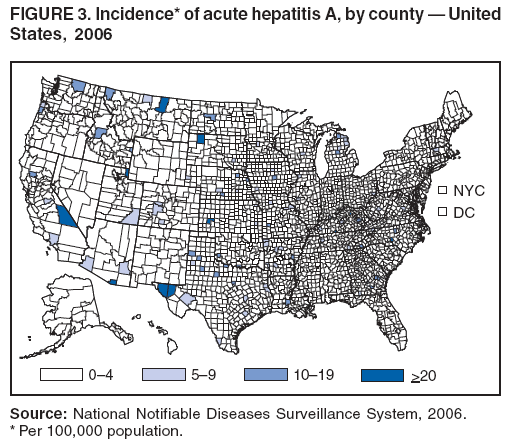 Return to top. Table 4 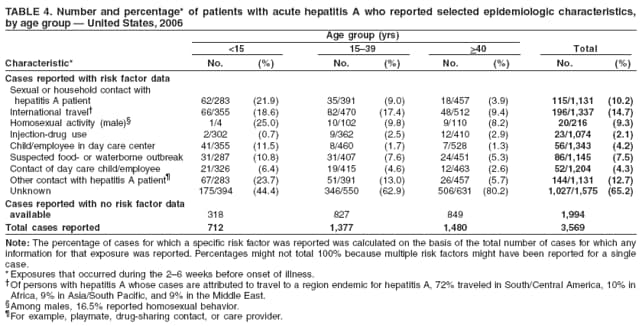 Return to top. Figure 4 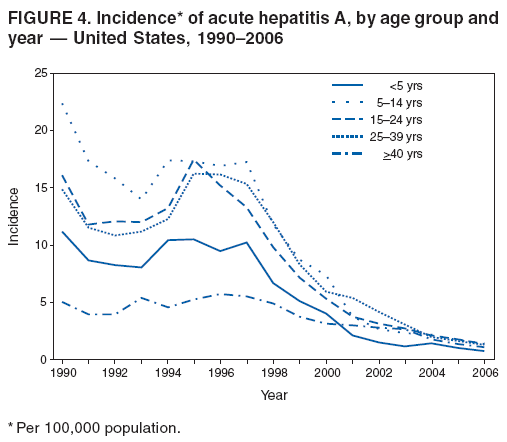 Return to top. Table 5 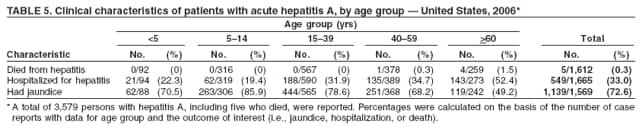 Return to top. Figure 5 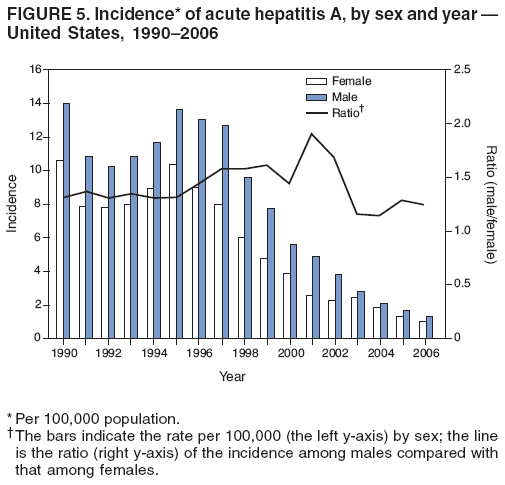 Return to top. Table 6 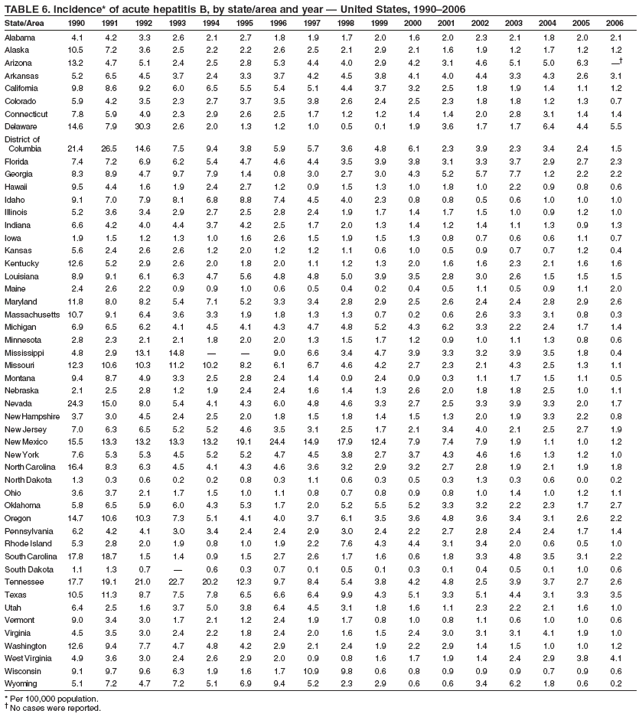 Return to top. Figure 6 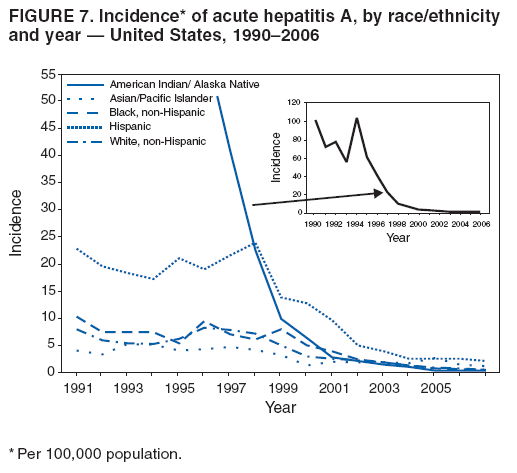 Return to top. Table 7 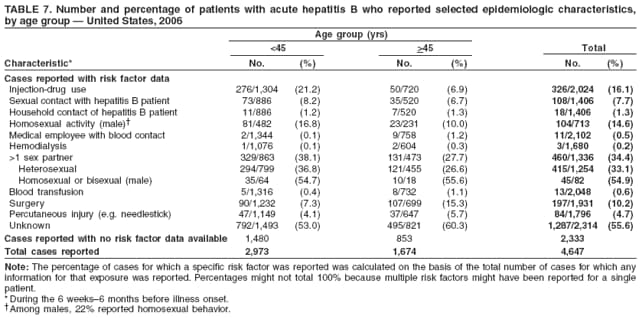 Return to top. Figure 7 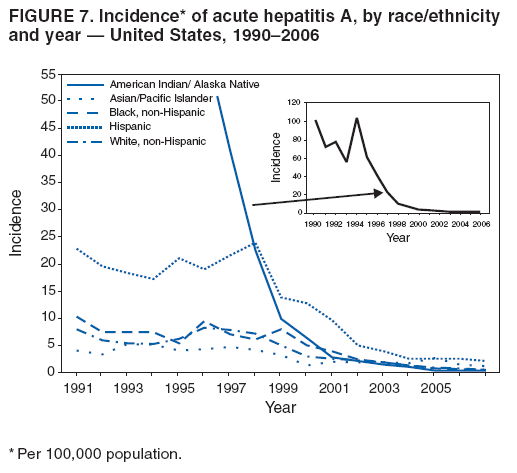 Return to top. Table 8 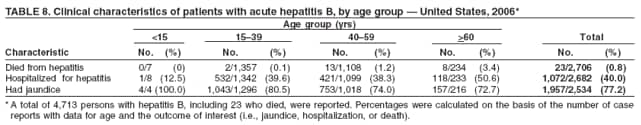 Return to top. Figure 8 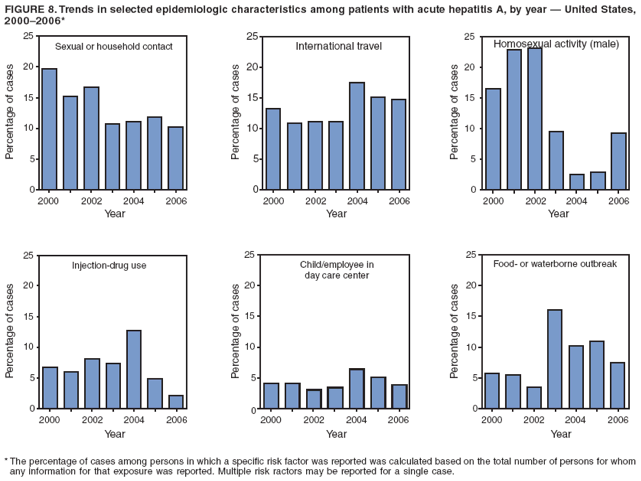 Return to top. Table 9 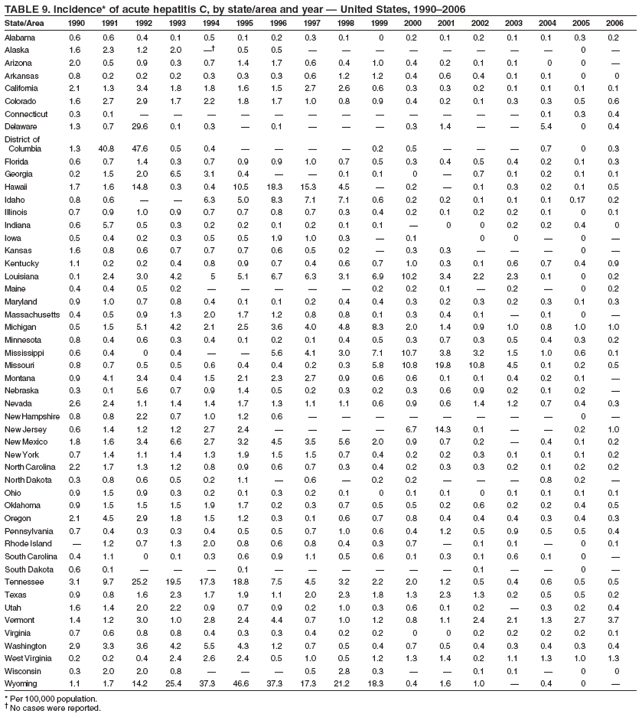 Return to top. Figure 9 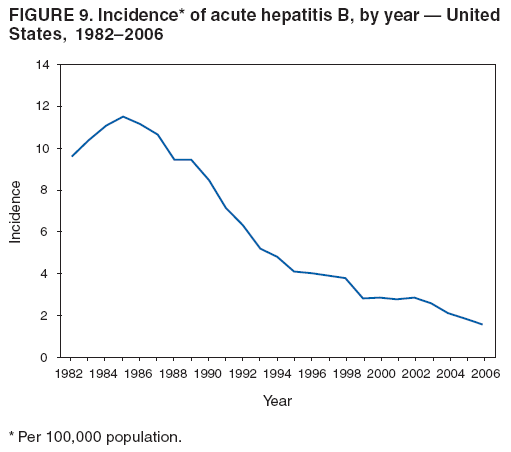 Return to top. Table 10 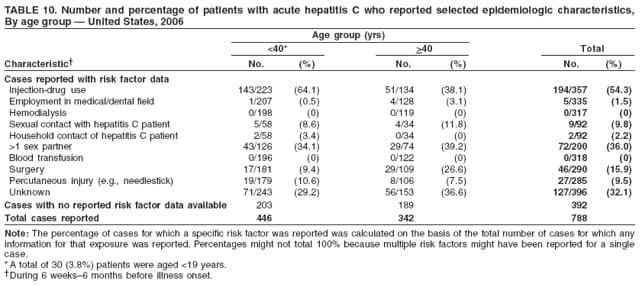 Return to top. Figure 10 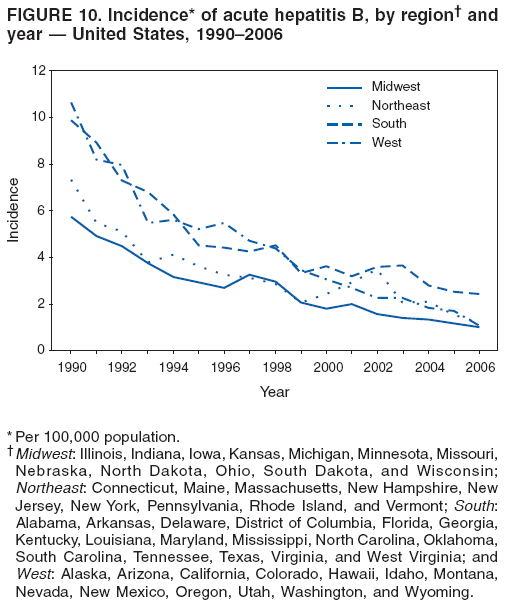 Return to top. Table 11 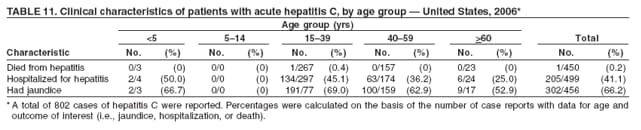 Return to top. Figure 11 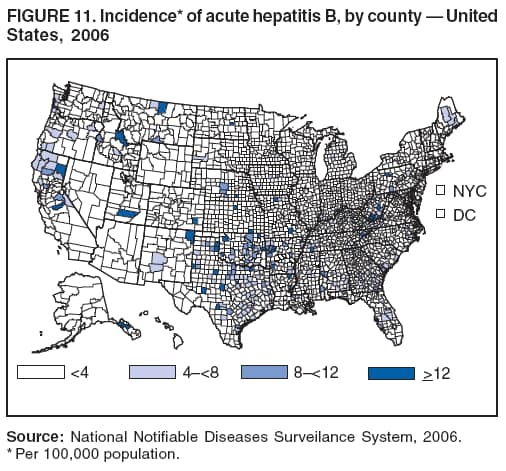 Return to top. Figure 12 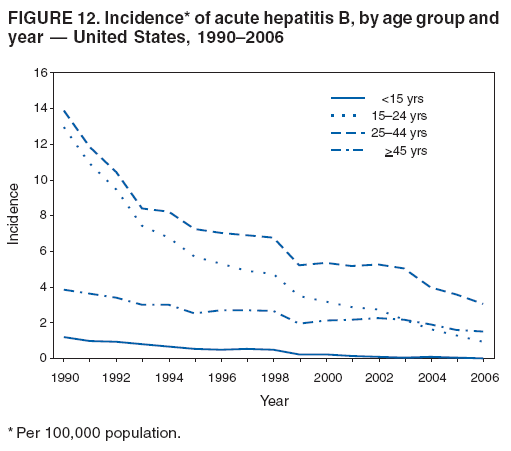 Return to top. Figure 13 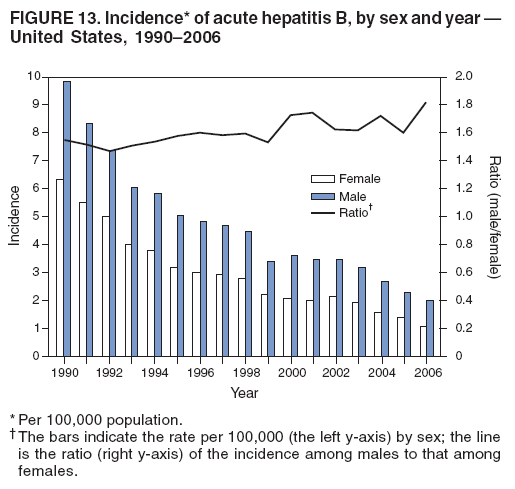 Return to top. Figure 14 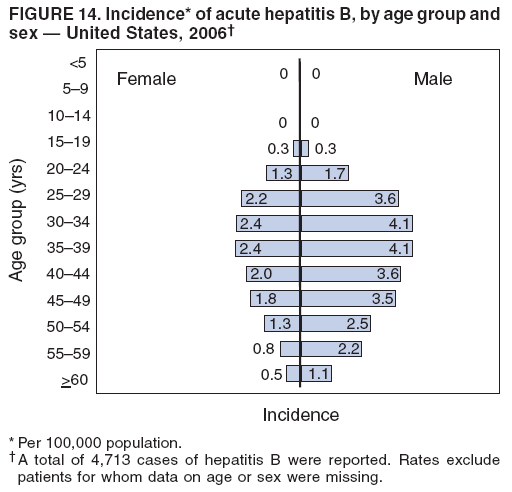 Return to top. Figure 15 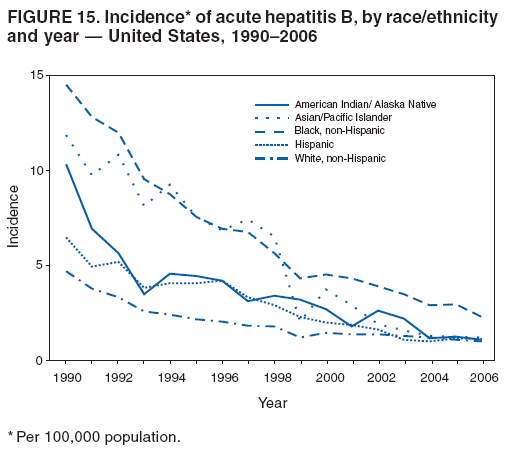 Return to top. Figure 16 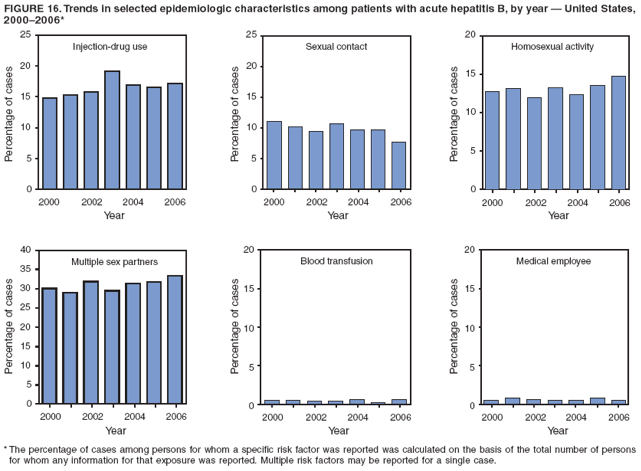 Return to top. Figure 17 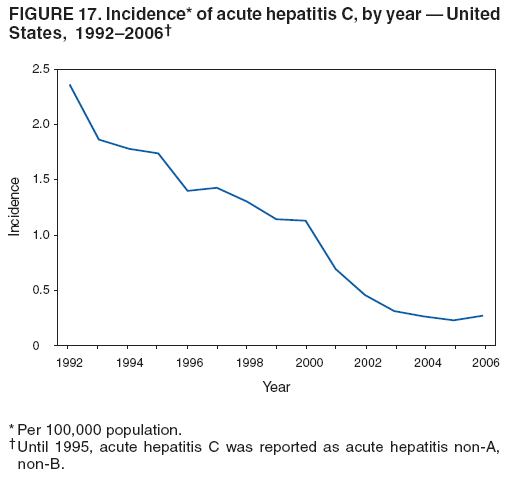 Return to top. Figure 18 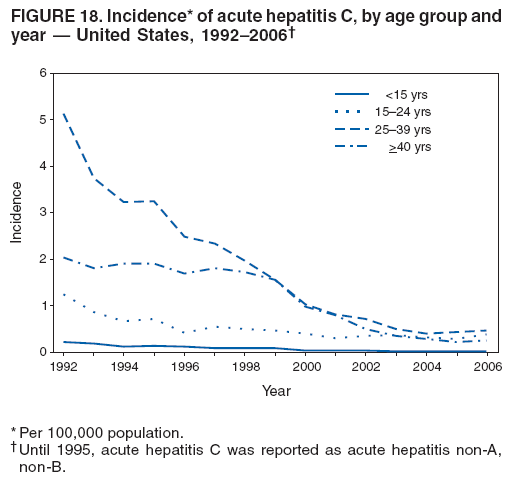 Return to top. Figure 19 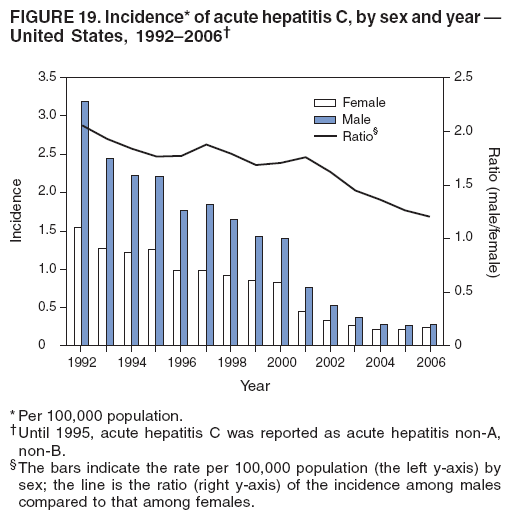 Return to top. Figure 20 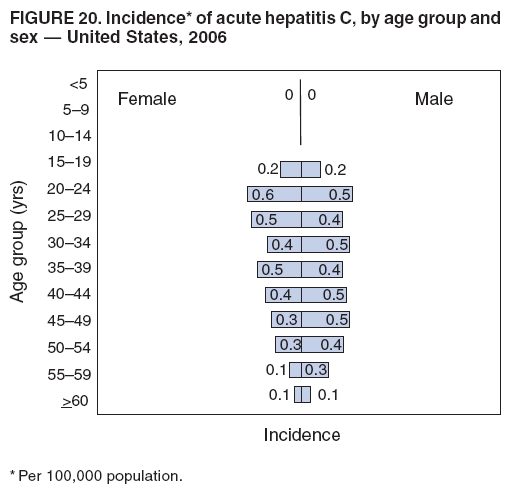 Return to top. Figure 21 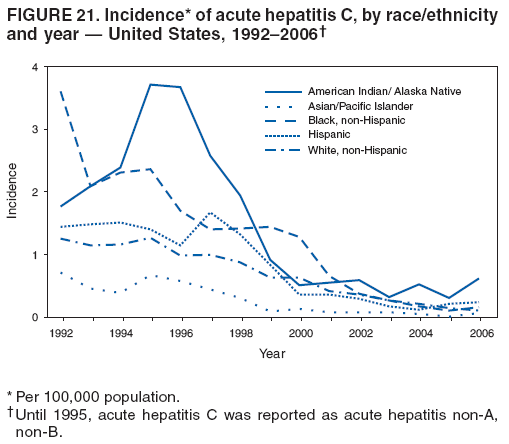 Return to top. Figure 22 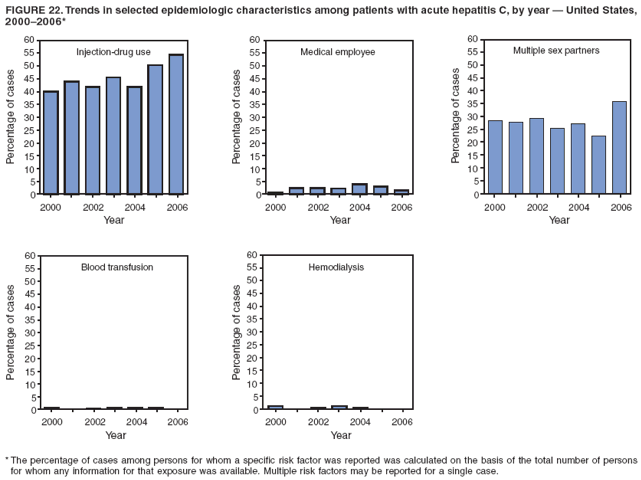 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 3/10/2008 |
|||||||||
|